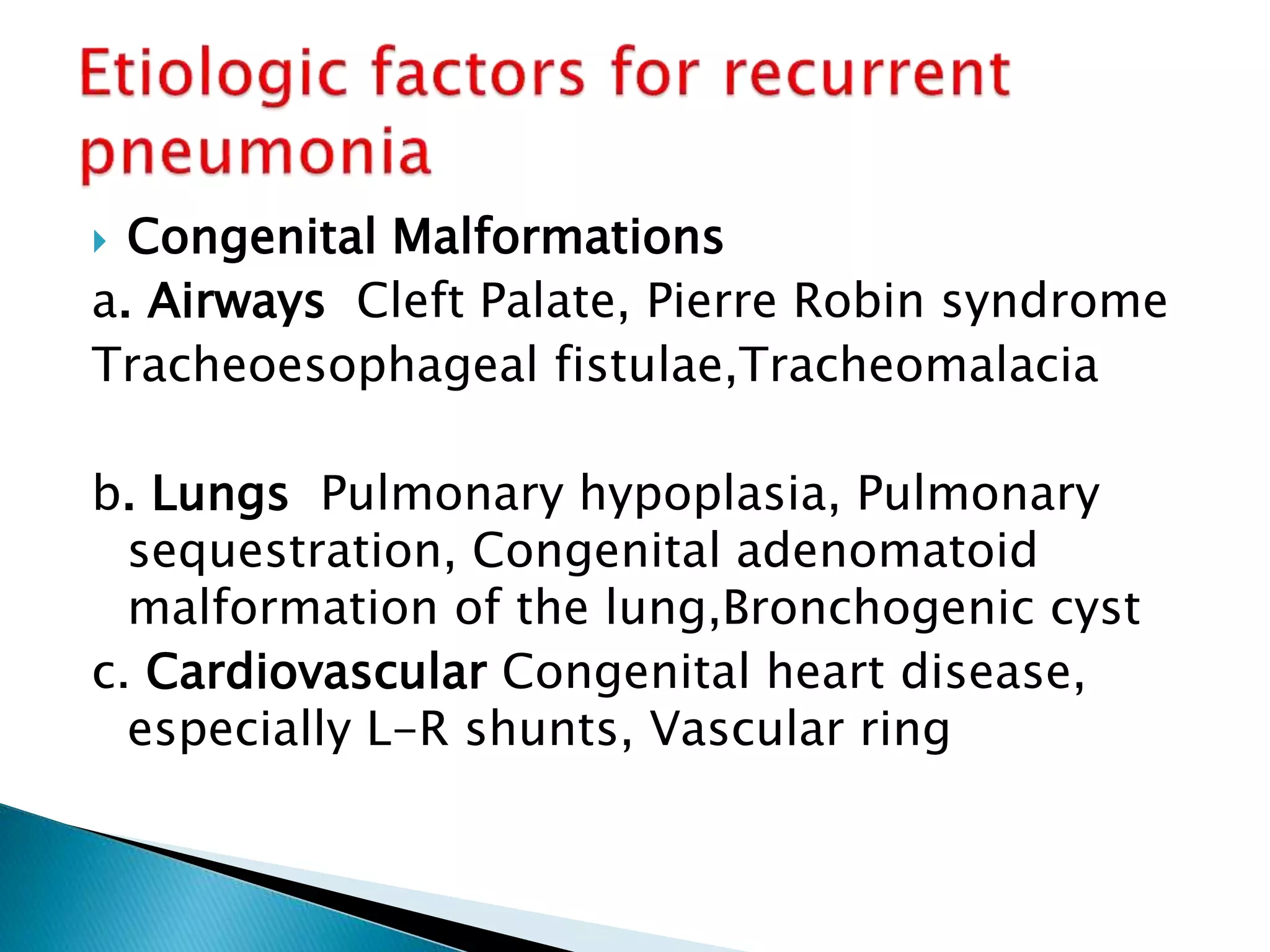
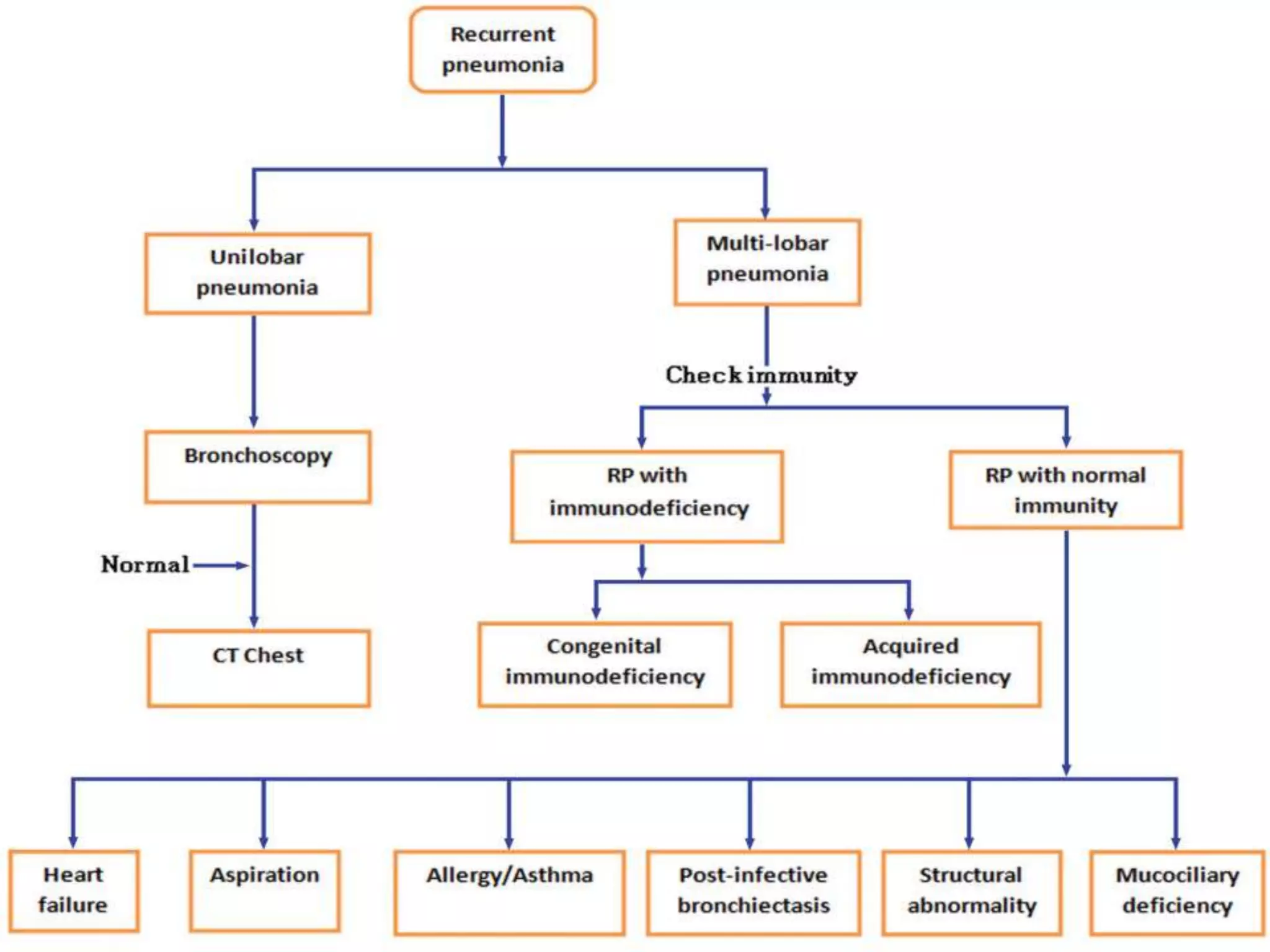
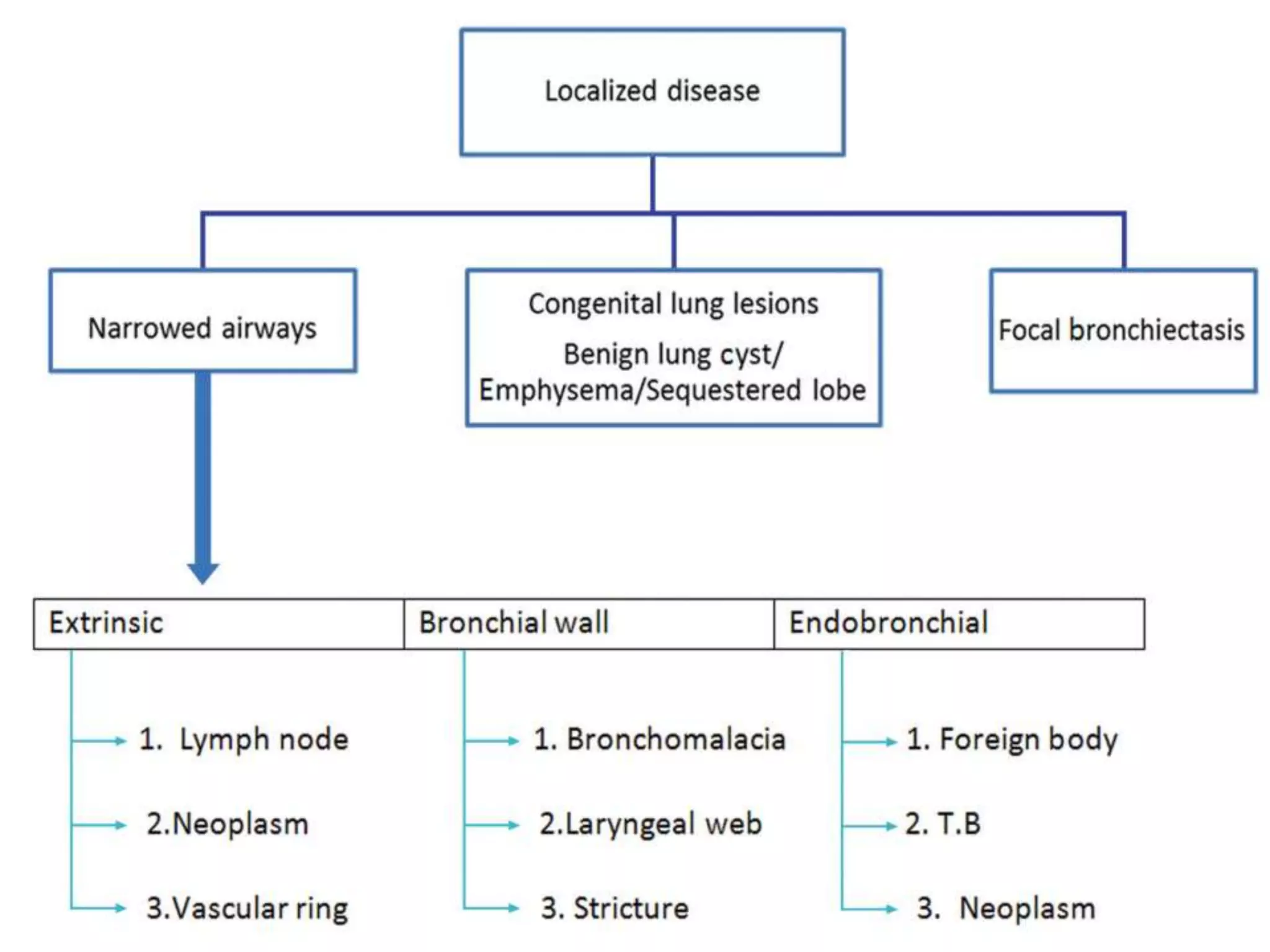
This document provides information on evaluating and diagnosing children with recurrent pneumonia. It discusses obtaining a thorough medical history including details of pneumonia episodes, risk factors, and associated symptoms. A complete physical exam focuses on the respiratory system and signs of underlying conditions. Initial tests include a CBC, chest X-ray, and Mantoux test. Further tests like CT, PFTs, bronchoscopy may help identify structural abnormalities, aspiration, or immunodeficiencies causing recurrent pneumonia. Treatment involves managing the specific illness and providing nutritional/respiratory support.