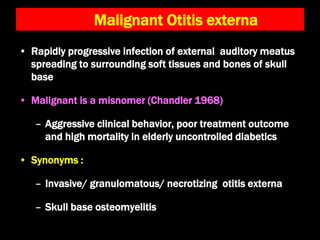
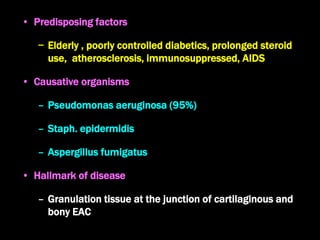
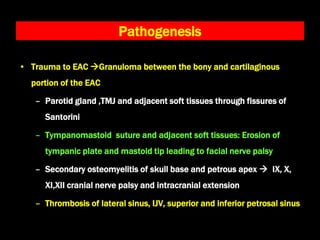
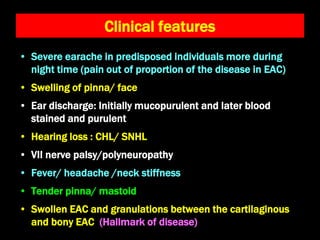
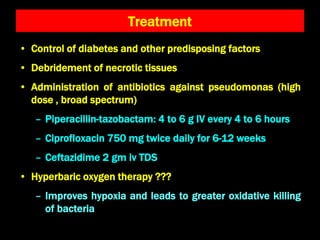
The document discusses malignant otitis externa, a rapidly progressive infection primarily affecting elderly, uncontrolled diabetics, with Pseudomonas aeruginosa as the main causative organism. It outlines clinical features such as severe earache, hearing loss, and facial nerve palsy, as well as diagnostic methods and treatment recommendations including managing diabetes and administering antibiotics. Key pathological consequences can include cranial nerve palsies and secondary osteomyelitis of the skull base.