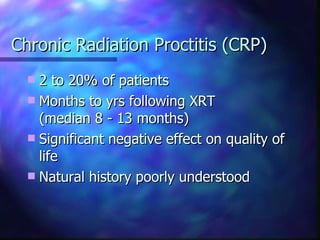
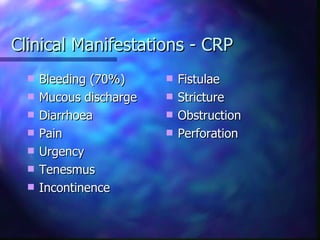
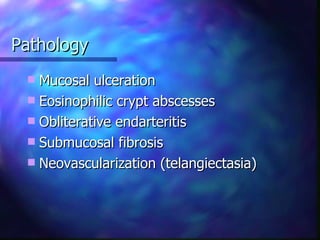
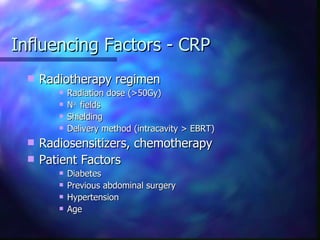
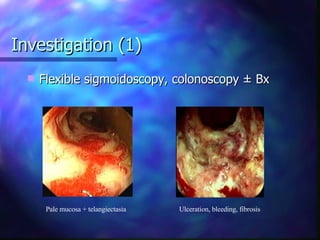
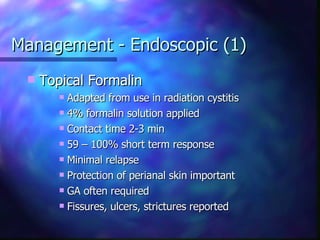
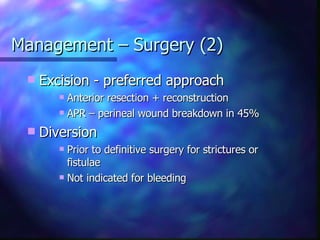
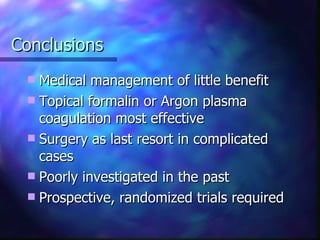
Radiation proctitis is inflammation of the rectum caused by radiation therapy for pelvic cancers. Acute radiation proctitis occurs during and shortly after radiation treatment and causes mild, self-limiting symptoms. Chronic radiation proctitis develops months to years later and significantly reduces quality of life, with bleeding being the main symptom. Flexible sigmoidoscopy and biopsy can identify ulceration, fibrosis, and other changes. Topical formalin application or argon plasma coagulation provides short-term relief but multiple treatments are often needed and relapse is common. Surgery is reserved for complicated cases that fail other management. Further research through prospective randomized trials is still needed.