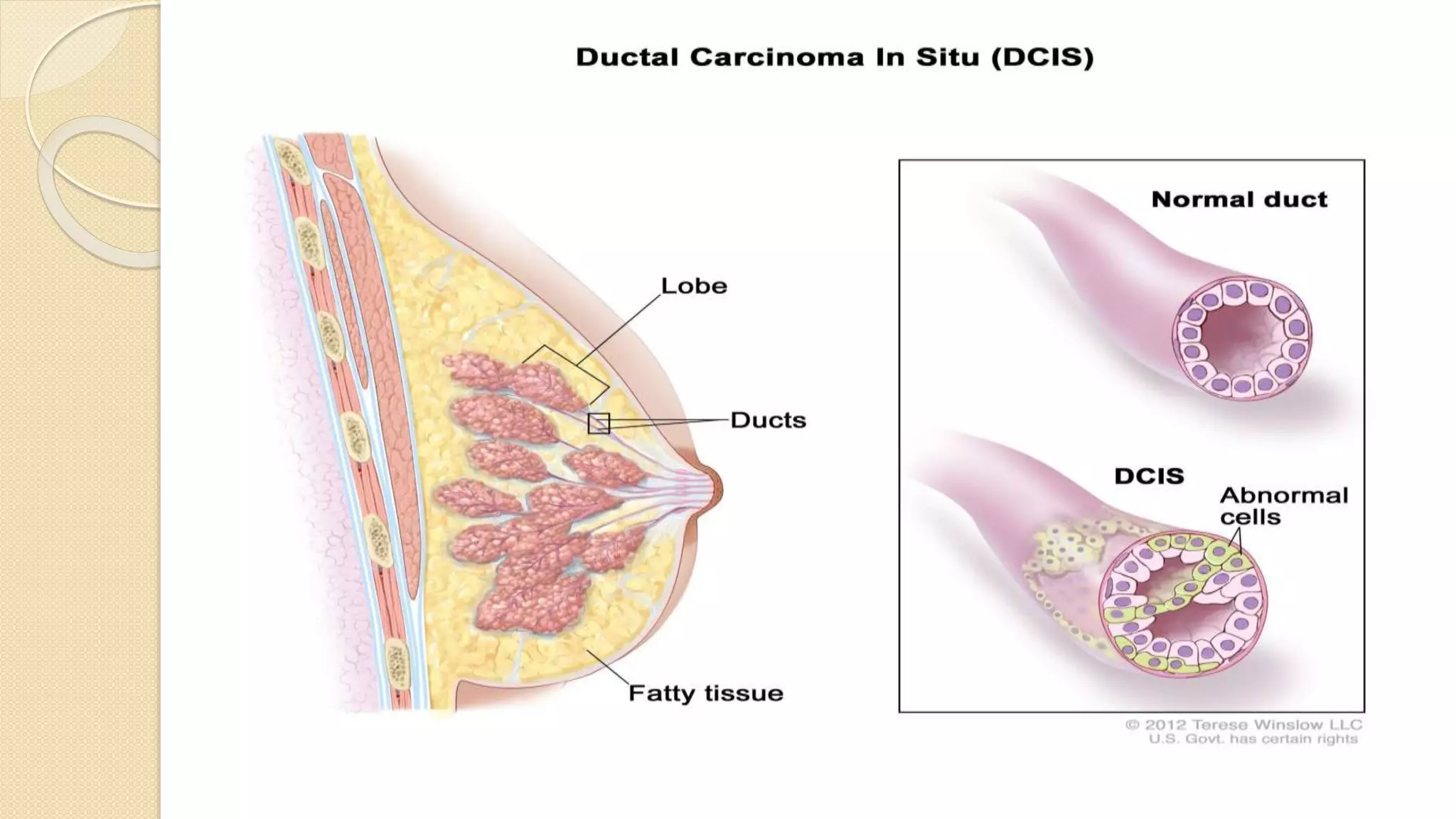
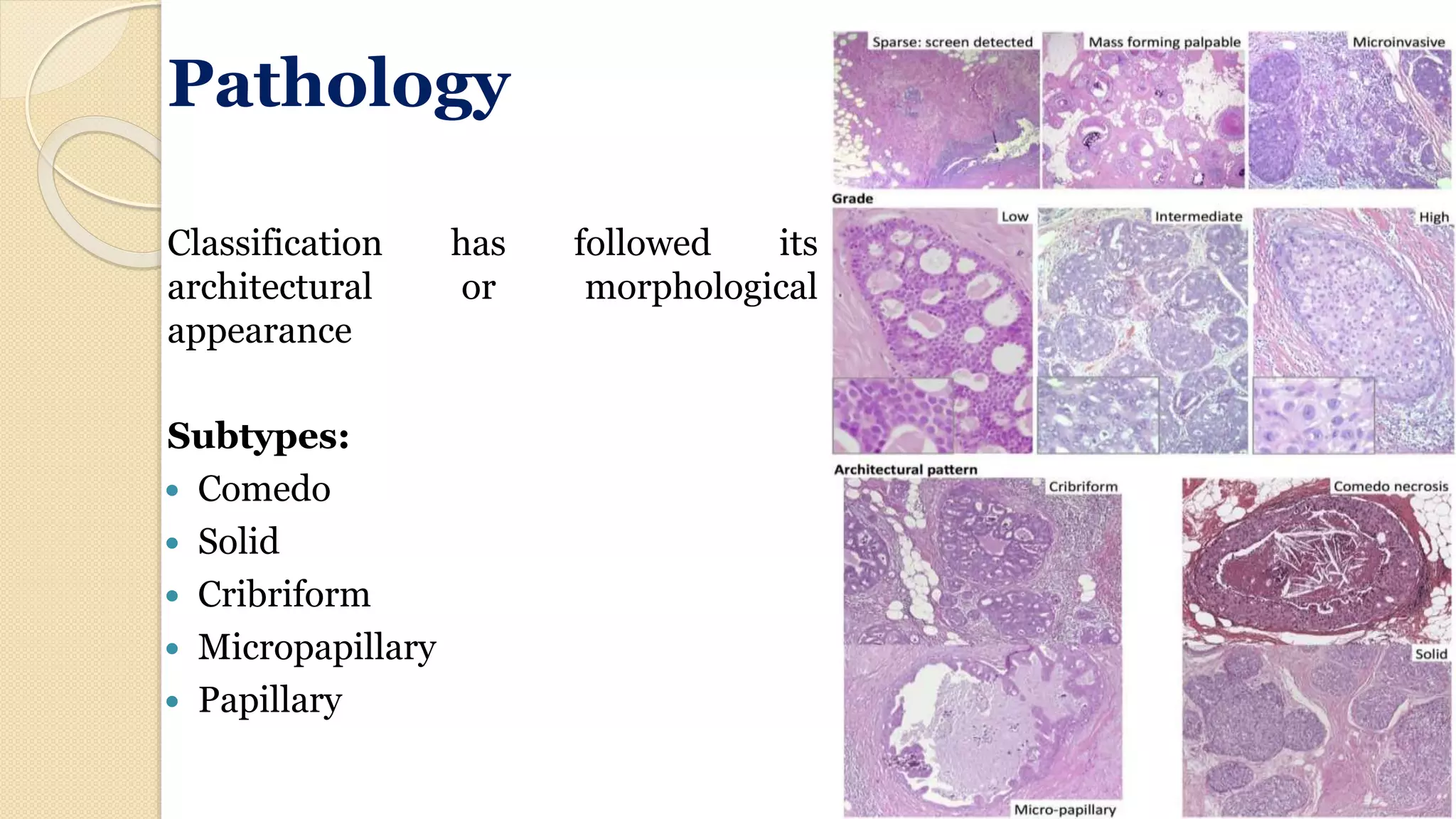
Ductal carcinoma in situ (DCIS) is an early, non-invasive form of breast cancer confined to the breast ducts. It affects approximately 25% of newly diagnosed breast cancers and is typically detected by mammography. While DCIS has no ability to metastasize, it can progress to invasive breast cancer if left untreated. Treatment options include mastectomy or breast-conserving surgery with radiation therapy. Factors like tumor size, grade, and margin status can predict recurrence risk. With advances in screening and treatment, long-term survival rates for DCIS patients now approach 100%.