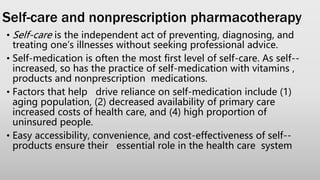
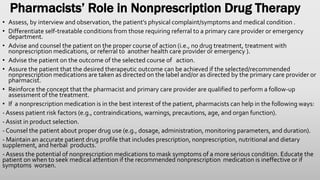
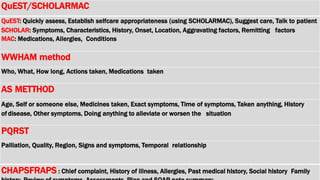
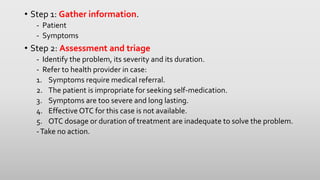
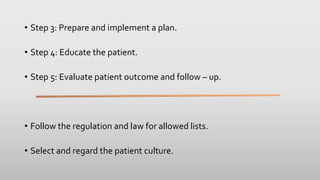
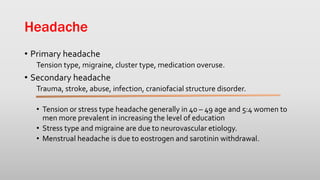
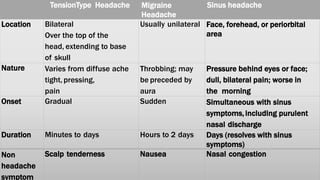
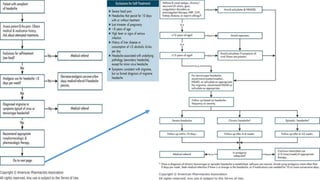
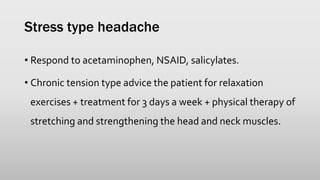
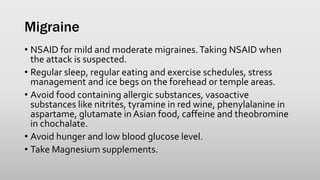
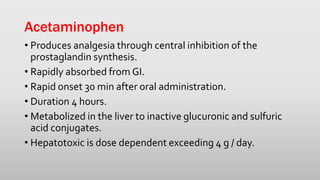
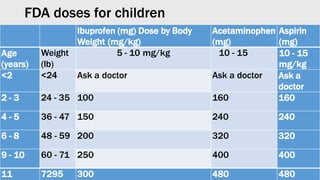
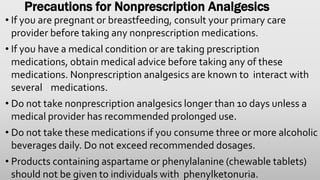
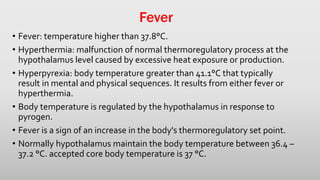
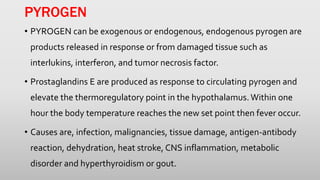
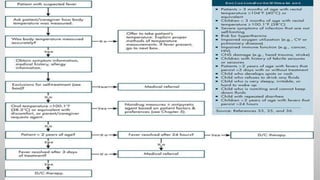
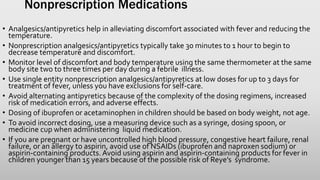
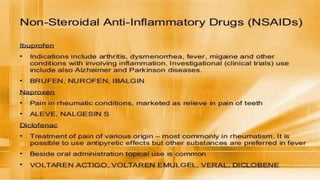
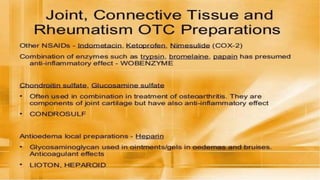
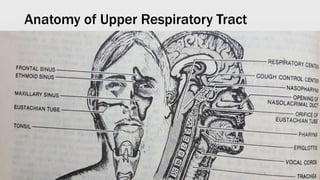
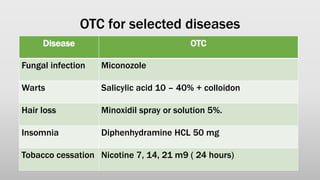
This document discusses nonprescription medications and the pharmacist's role in nonprescription drug therapy. It provides information on different types of nonprescription medications (OTC, BTC), factors driving self-medication, and the pharmacist's steps to assess patients and recommend appropriate self-treatable conditions or referrals. It also covers guidelines for treating common conditions like headaches, fever, and drug interactions to consider with nonprescription analgesics. The pharmacist's role is to properly assess patients, advise on treatment options, educate on proper use and monitoring of OTC medications, and evaluate treatment outcomes.








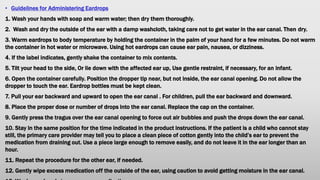
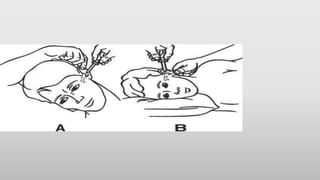
![The use of ceruminolytics and irrigation together may improve overall removal of impacted cerumen. The ceruminolytic
agent is administered first. Then follow the irrigation technique as described below, paying special attention to cautionary
instructions.
1. Prepare a warm solution of plain water or other solution as directed by your primary care provider. Eight ounces of
solution should be sufficient to clean out the ear canal.
2. To catch the returning solution, hold a container under the ear being cleaned. An emesis basin is ideal because it fits
the contour of the neck. Tilt the head down slightly on the side where the ear is being cleaned.
3. Gently pull the earlobe down and back to expose the ear canal.
4. Place the open end of the syringe into the ear canal with the tip pointed slightly upward toward the side of the ear
canal Do not aim the syringe into the back of the ear canal. Use caution and make sure the syringe does not obstruct
the outflow of solution.
5. Squeeze the bulb gently—not forcefully—to introduce the solution into the ear canal and to avoid rupturing the
eardrum. (Note: Only health professionals trained in aural hygiene should use forced water sprays [e.g., Water Pik] to
remove cerumen.)
6. Do not let the returning solution come into contact with the eyes.
7. If pain or dizziness occurs, remove the syringe and do not resume irrigation until a health care provider is consulted.
8. Make sure all water is drained from the ear to avoid predisposing to infection from waterclogged ears.
9. Rinse the syringe thoroughly before and after each use, and let it dry.
10. Store the syringe in a cool, dry place (preferably, in its original container) away from hot surfaces and sharp
instruments
11. If cerumen still remains, consult a provider.](https://image.slidesharecdn.com/otclectures-201104140959/85/OTC-lectures-137-320.jpg)