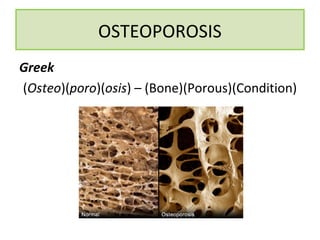
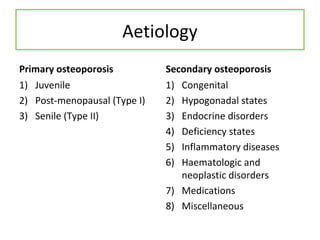
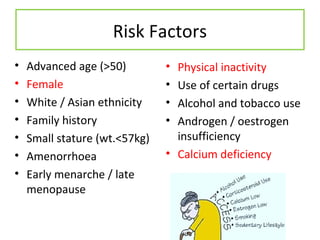
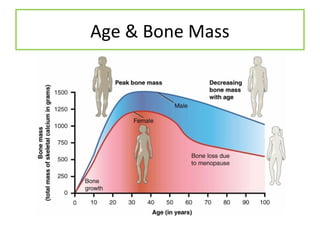
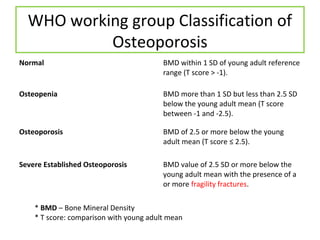
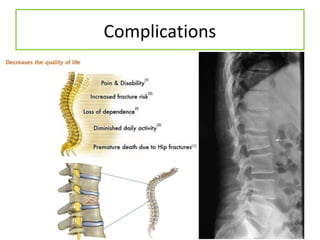
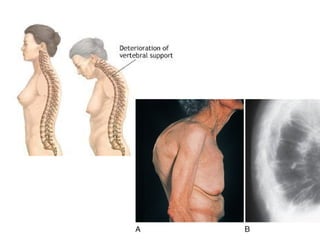
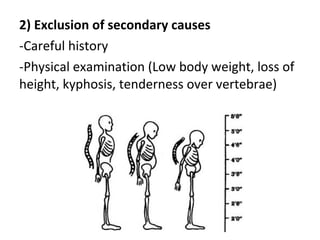
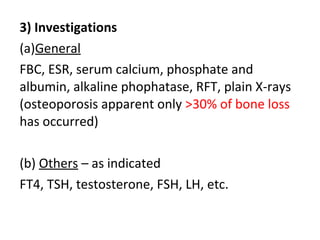
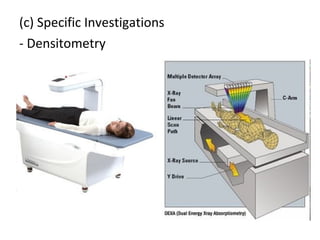
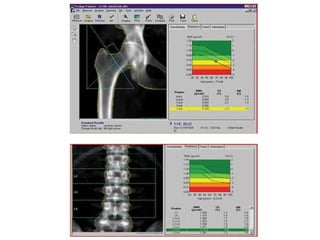
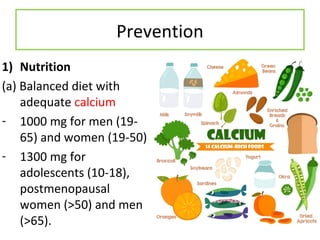
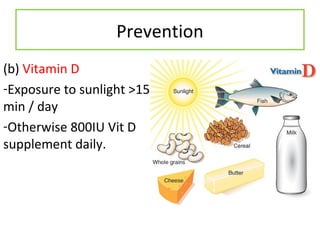
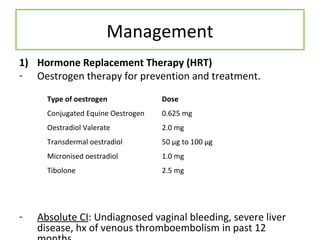
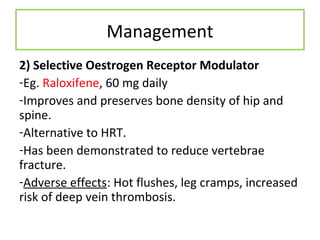
Osteoporosis is a systemic skeletal disease characterized by low bone mass and deterioration of bone tissue, leading to fragile bones that are prone to fracture. It is primarily caused by age-related bone loss after peak bone mass has been achieved. Diagnosis involves excluding secondary causes, and may include blood tests, imaging like DEXA scans to measure bone mineral density. Management focuses on lifestyle factors like nutrition, exercise, and medications to prevent bone loss and fractures.