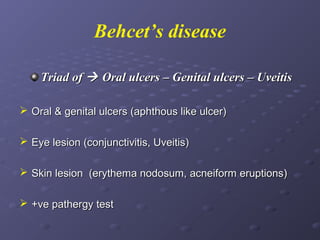
This document describes various types of oral lesions including macules, papules, plaques, vesicles, bullae and pustules. It then discusses important causes of oral mucosal ulcers, separating them into those that involve preceding vesiculation like herpes simplex, herpes zoster, chickenpox, hand-foot-and-mouth disease and herpangina, and those without preceding vesiculation such as cytomegalovirus, tuberculosis, syphilis, traumatic ulcers, aphthous stomatitis, Behcet's disease, Reiter's syndrome, lichen planus and some mucosal drug reactions. Specific features of each condition are described in detail with examples