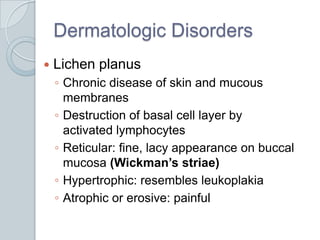
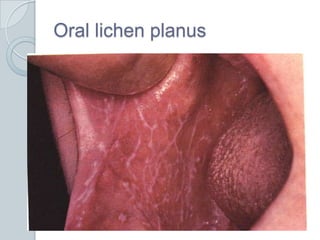
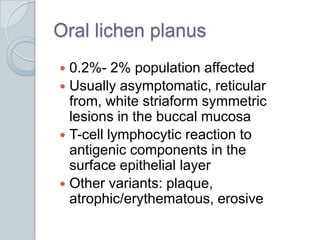
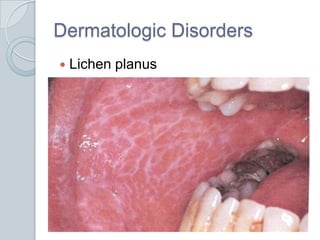
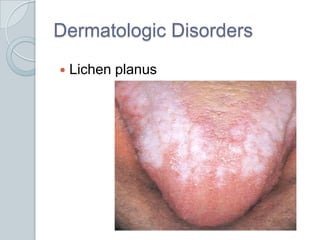
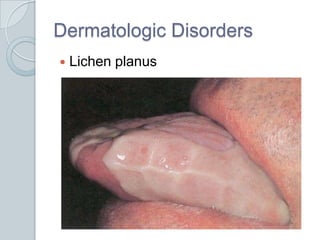
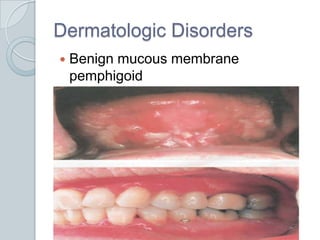
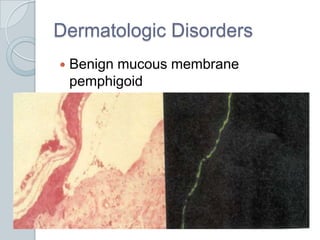
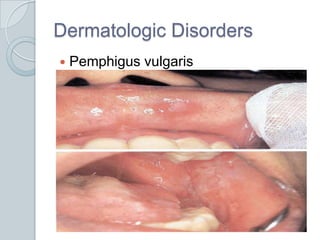
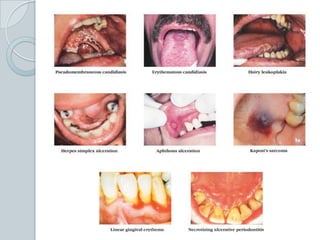
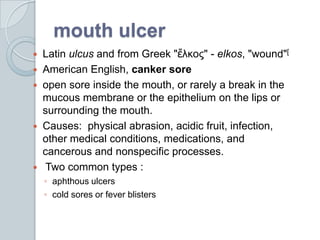
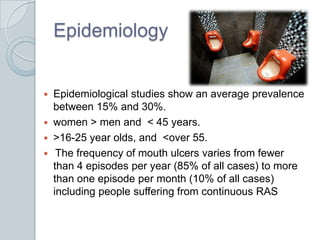
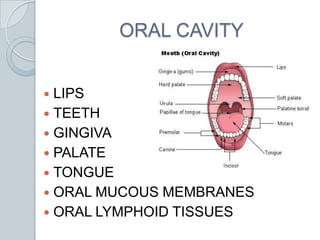
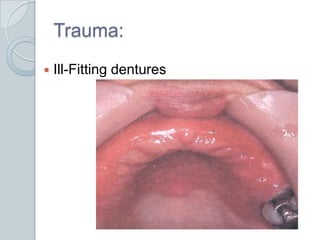
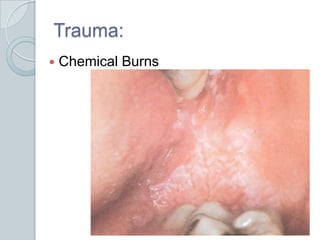
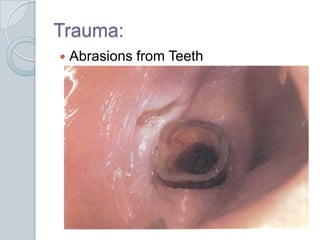
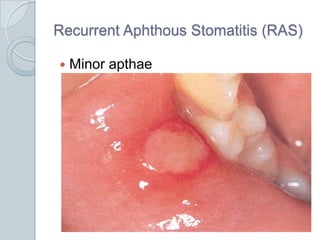
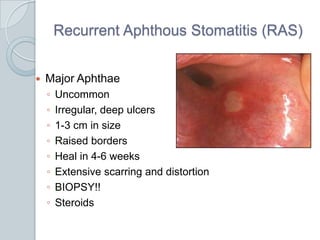
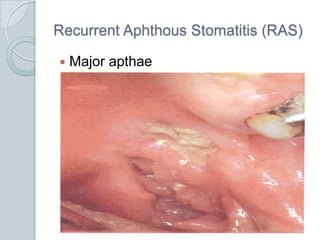
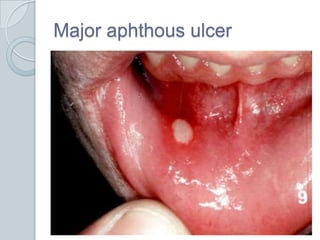
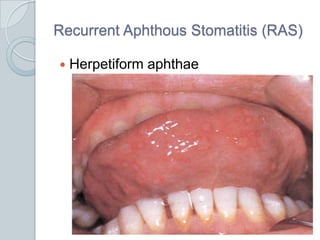
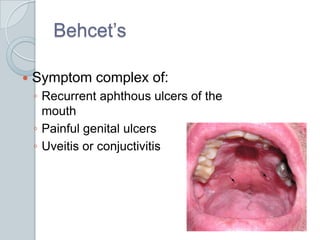
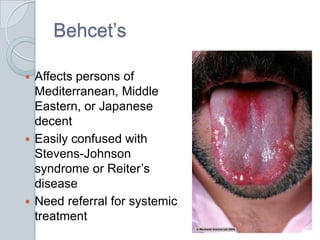
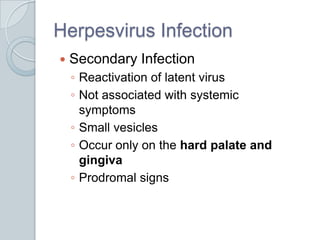
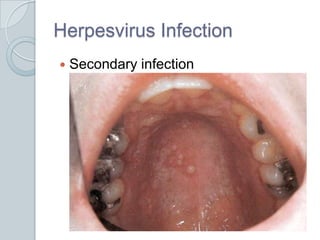
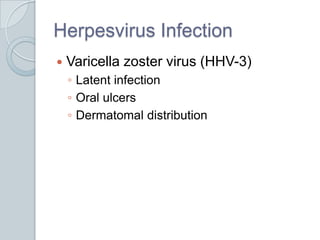
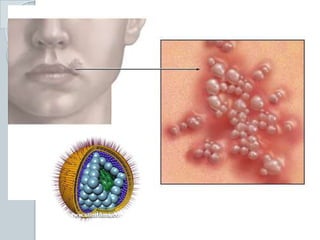
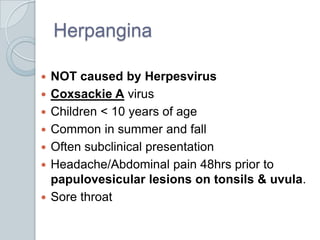
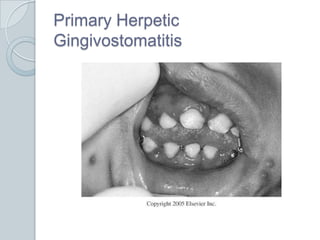
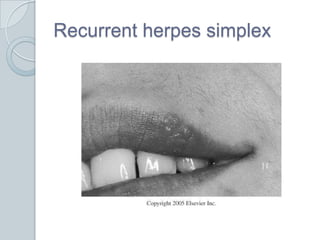
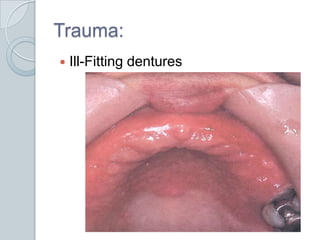
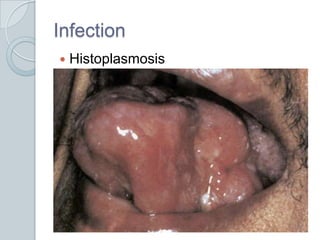
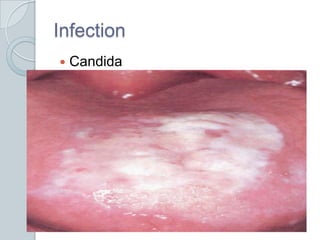
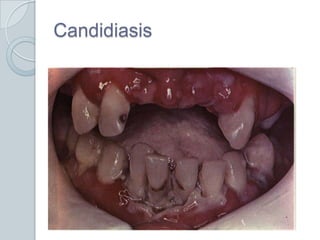
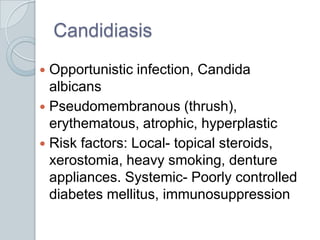
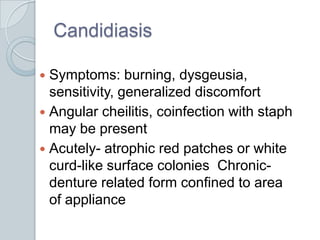
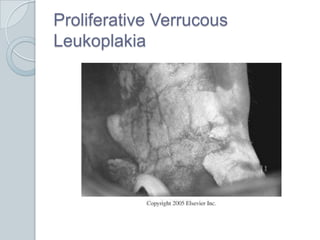
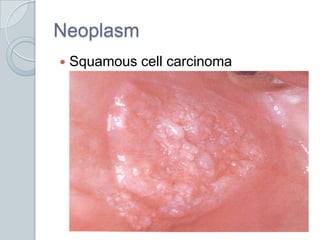
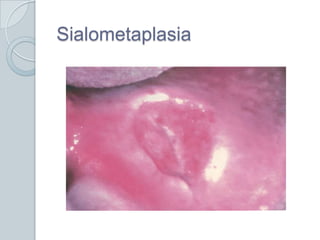
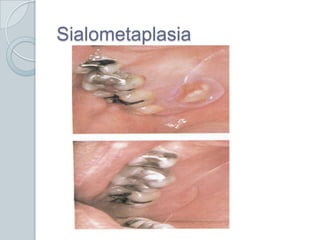
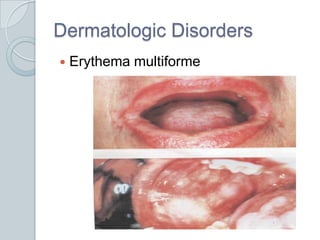
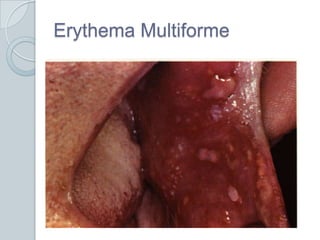
This document discusses various lesions that can occur in the oral cavity. It begins by defining mouth ulcers and listing common causes such as physical abrasion, infection, and cancer. It then covers specific conditions like recurrent aphthous stomatitis, lichen planus, pemphigus vulgaris, and necrotizing sialometaplasia. It provides details on symptoms, appearance, epidemiology, treatment and pathogenesis for each condition. In general, the document provides a comprehensive overview of acute and chronic ulcerative lesions that can present in the oral cavity.














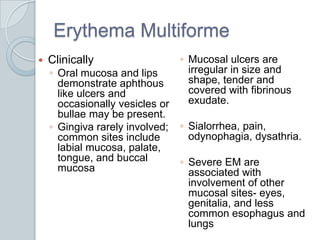
![Erythema MultiformeHistopathology]Intense lymphocytic infiltration in a perivascular distribution and edema from submucosa into the lamina propria, epithelium lack antibodies, blood vessels contain fibrin, C3, IgM Treatment- with oral involvement only can treat symptomatically/short course of corticosteroids](https://image.slidesharecdn.com/oralcavitylesions-101206120534-phpapp02/85/Oral-cavity-lesions-91-320.jpg)