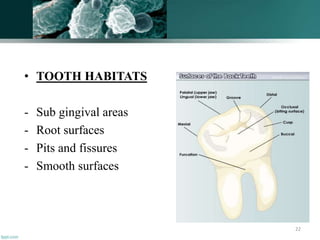
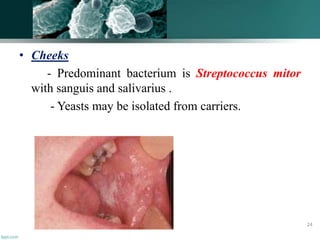
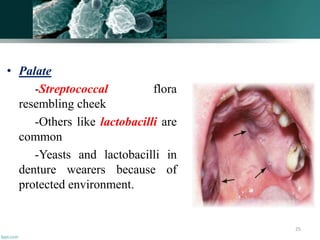
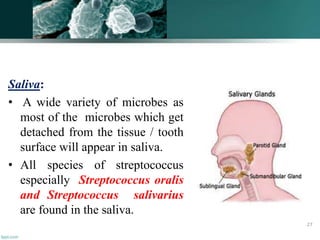
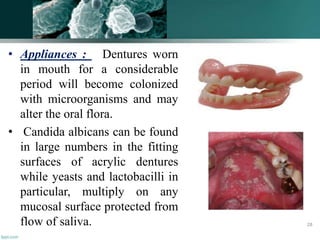
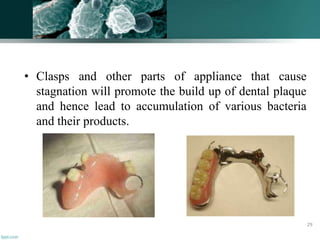
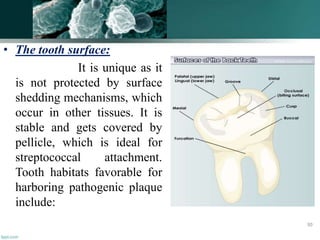
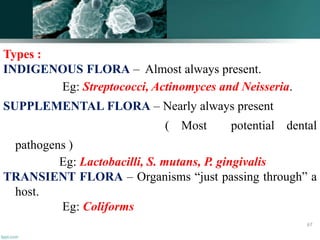
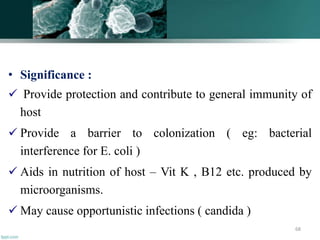
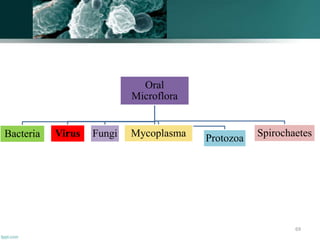
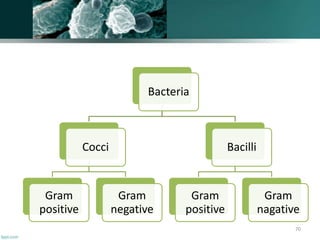
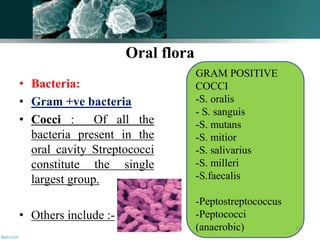
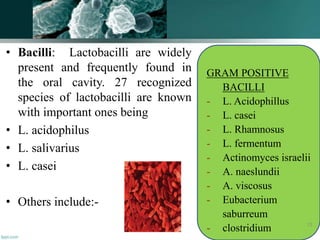
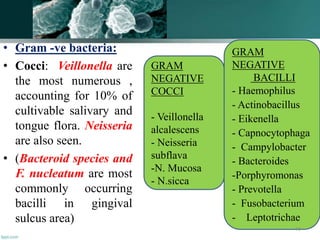
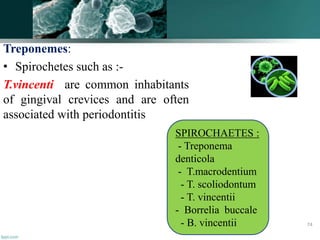
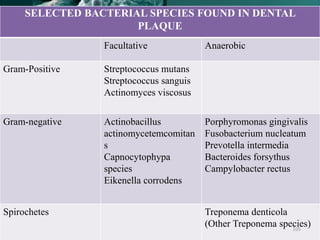
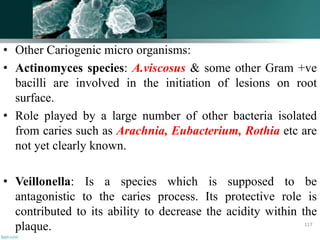
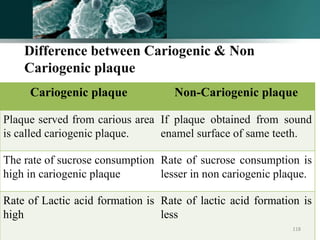
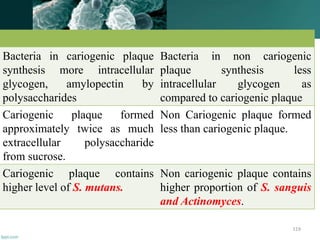
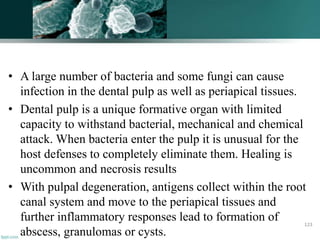
The document discusses the oral microflora, including the different oral habitats that microorganisms inhabit, such as the teeth, oral mucosa, tongue, and saliva. It describes the various microorganisms commonly found in the oral cavity, including streptococci, actinomyces, and candida albicans. It also defines several terms related to oral microflora and their ecology.

![]
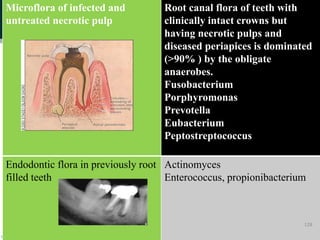
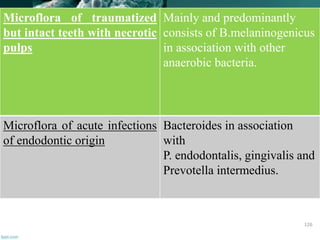
Microflora of endodontic
‘flare-up’ infections
Obligate Anaerobes Such As
Veillonella
Capnocytophaga
Eiknella
Bacteroides
Fusobacterium
Treponema.
Microflora on refractory
endodontic cases are
E. faecalis
Candida albicans
Actinomyces israelii
127](https://image.slidesharecdn.com/oralmicroflora-180728192716/85/Oral-microflora-127-320.jpg)