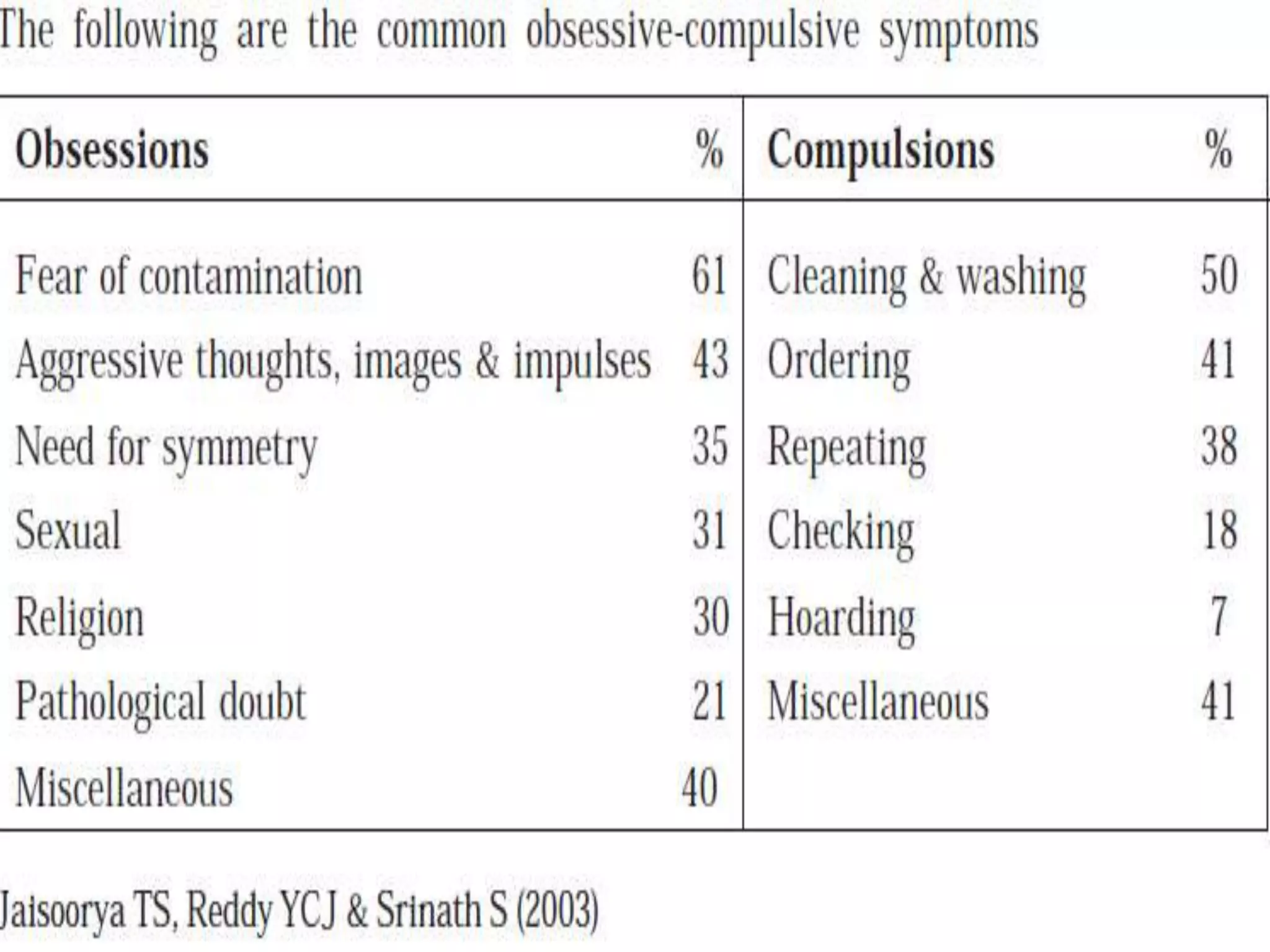
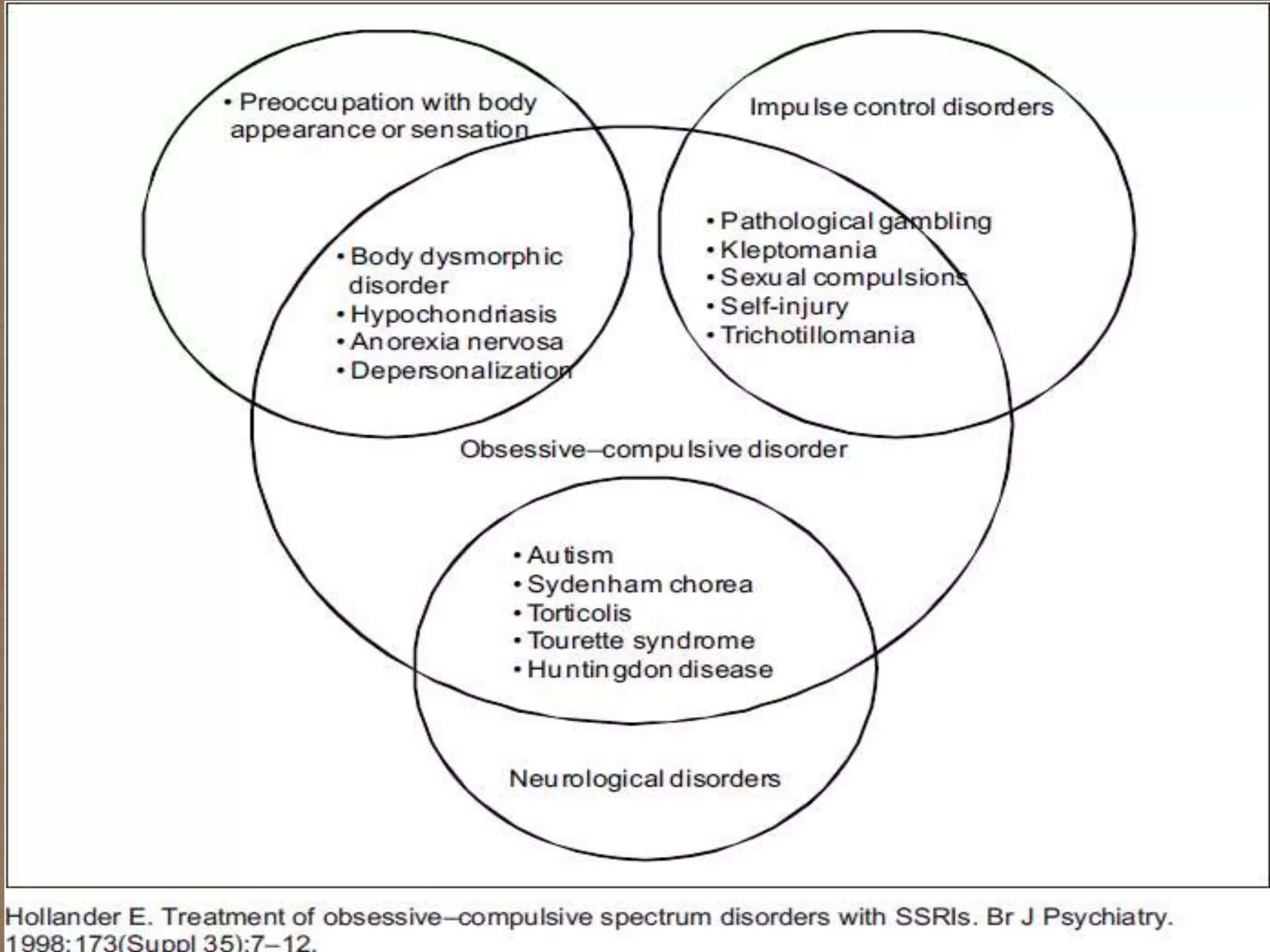
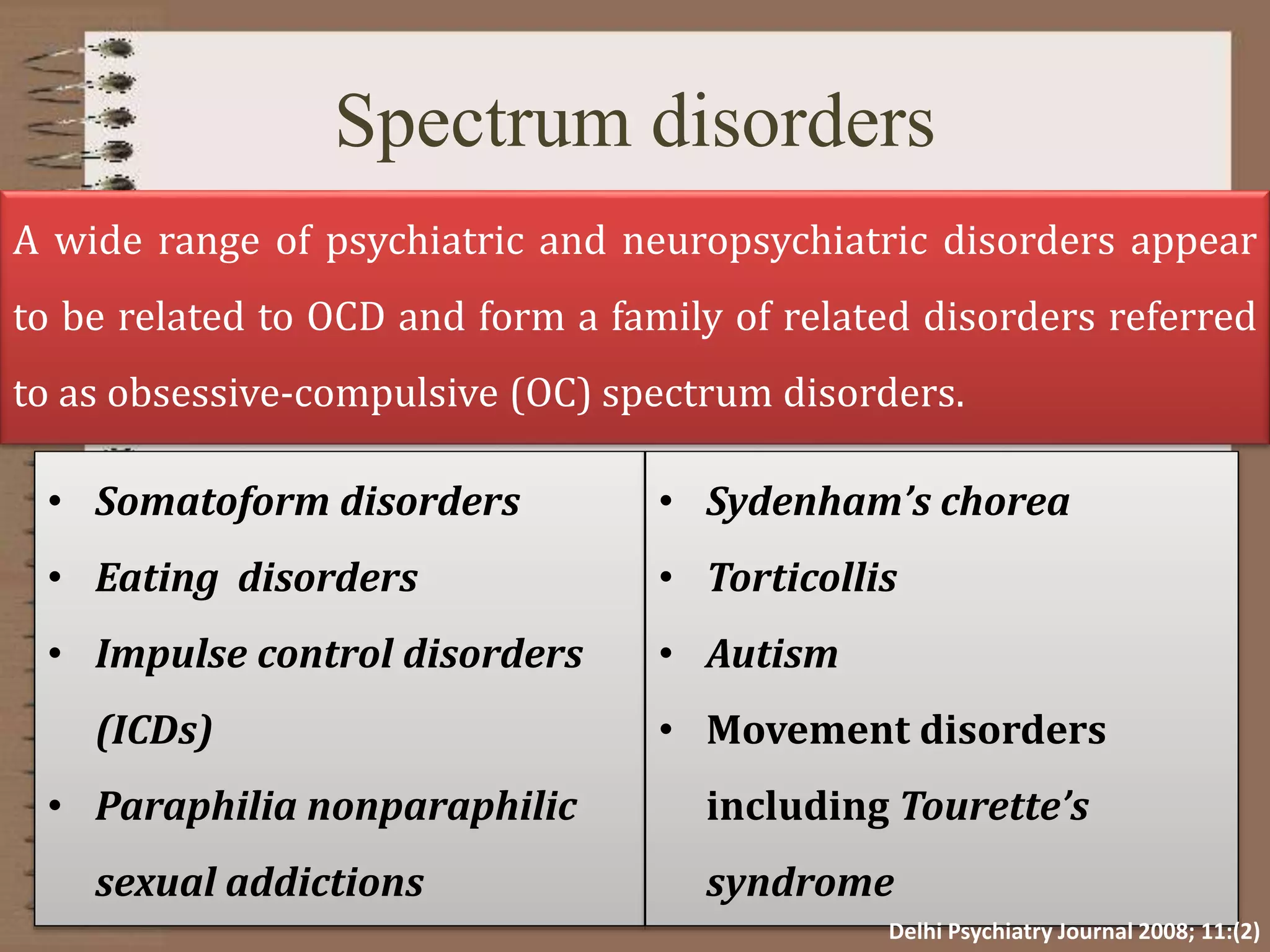
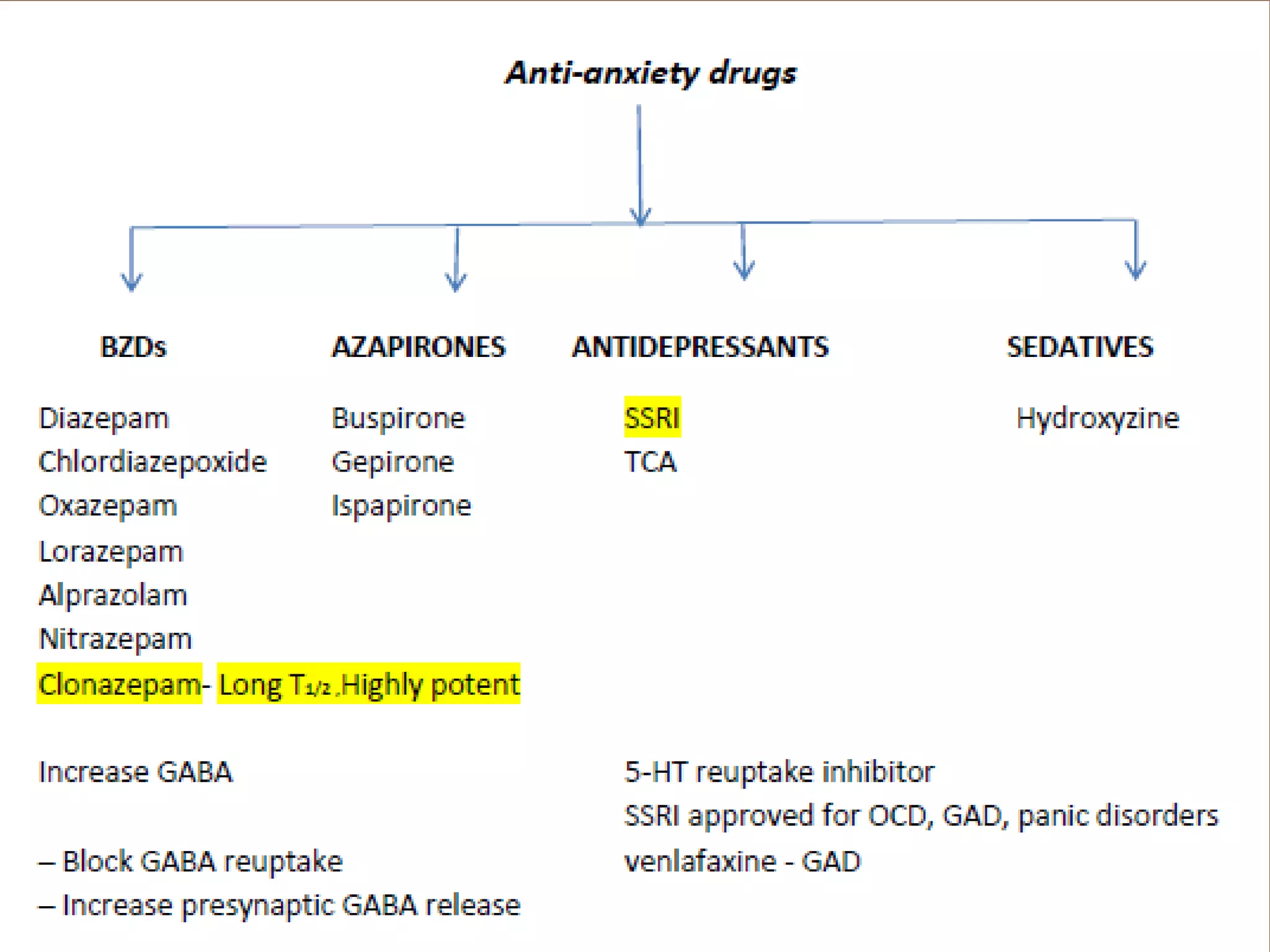
OCD is an anxiety disorder characterized by obsessive thoughts and compulsive behaviors that interfere with daily life. It is caused by abnormalities in brain circuits involving serotonin, dopamine, and glutamate. Treatment involves SSRIs, cognitive-behavioral therapy, and exposure therapy. OCD is part of a spectrum of related disorders involving similar obsessions and compulsions.

















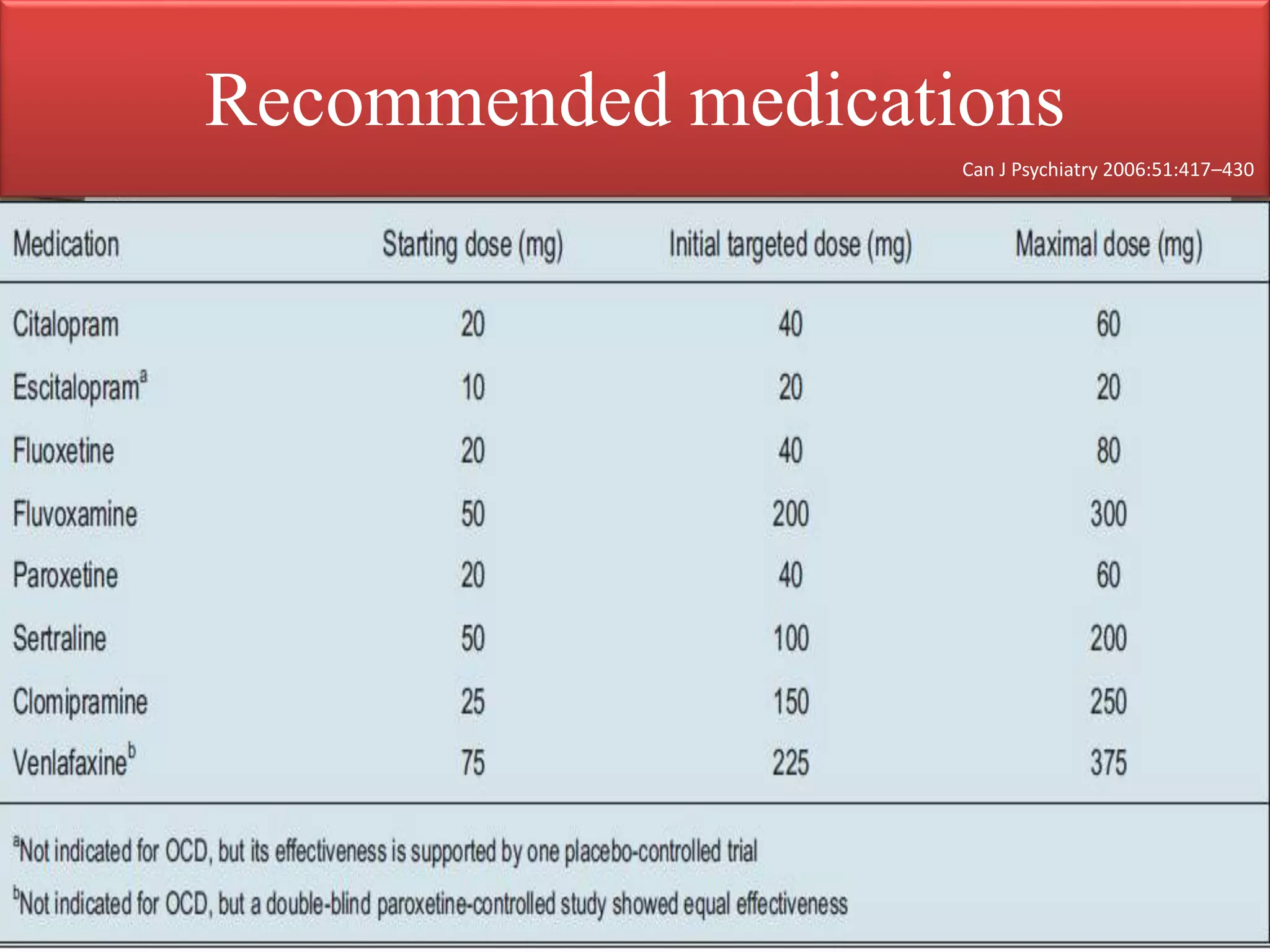
![SSRI
Selective serotonin reuptake inhibitors
(SSRI) considered to be first choice of drug for management
of OCD and related disorders.
SSRI Inhibits the reuptake of serotonin back into the nerve
terminal
At the present time, each of five selective SSRIs fluoxetine
[Prozac], paroxetine [Paxil], fluvoxamine [Luvox],
sertraline [Zoloft], and citalopram [Celexa] have shown
efficacy for OCD in randomized controlled trials
Essent Psychopharmacol 5:4, 2004](https://image.slidesharecdn.com/ocdspectrumdisorder-150828081751-lva1-app6892/75/Ocd-spectrum-disorder-34-2048.jpg)