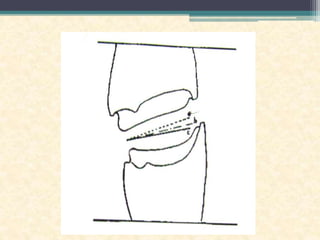
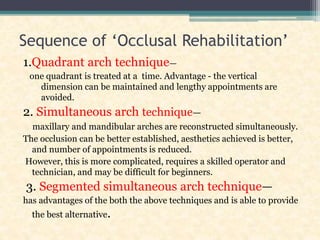
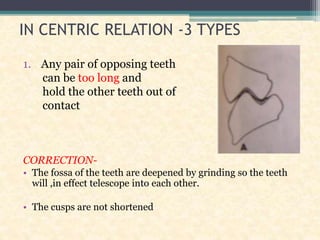
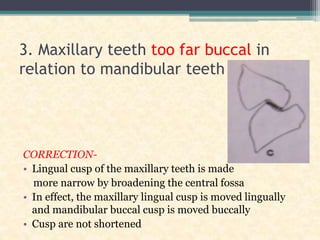
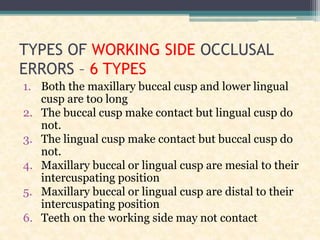
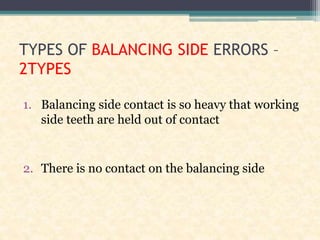
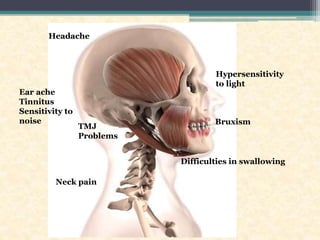
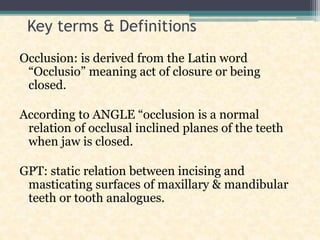
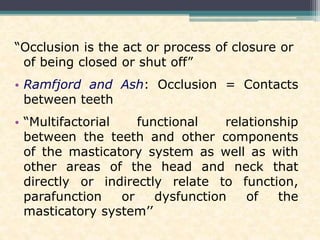
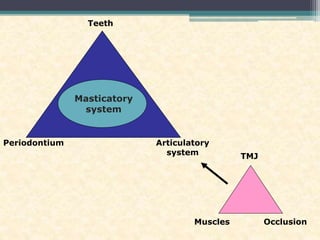
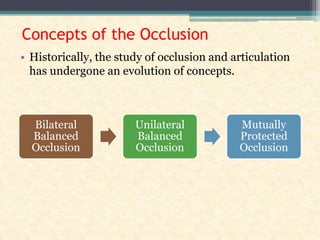
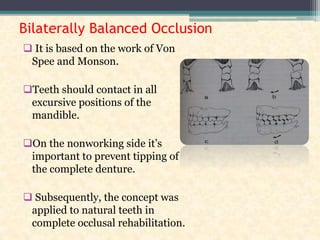
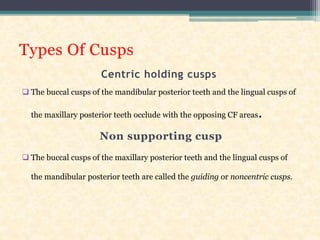
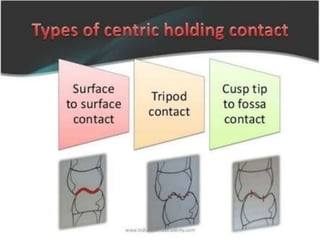
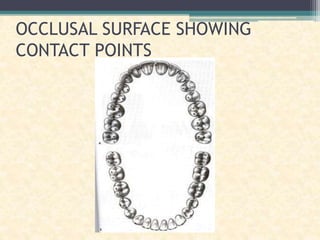
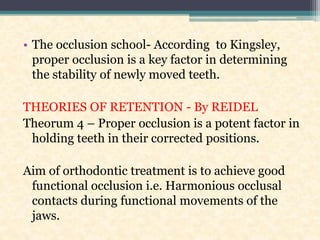
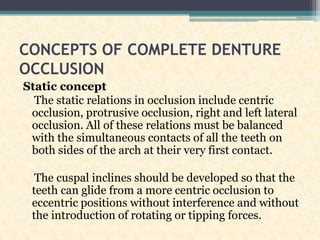
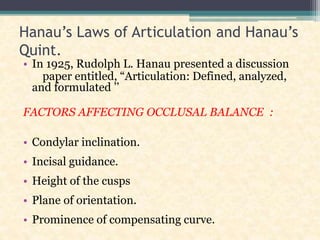
This document provides an overview of occlusion in dentistry. It defines key terms like occlusion and discusses concepts of occlusion including bilaterally balanced, unilaterally balanced, and canine guided occlusion. The importance of occlusion is described for various dental specialties like pedodontics, orthodontics, oral surgery, restorative dentistry and prosthodontics. Basic occlusion principles from dental anatomy are covered. The document also discusses types of occlusal errors and their correction as well as Hanau's laws of articulation.






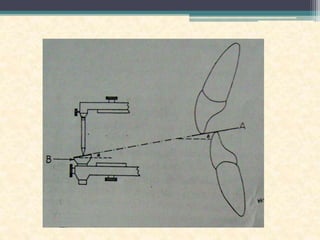
![INCISAL GUIDE ANGLE [GPT9]
1: anatomically, the angle formed by the
intersection of the plane of occlusion and a line
within the sagittal plane determined by the
incisal edges of the maxillary and mandibular
central incisors when the teeth are in maximum
intercuspation
2: on an articulator, that angle formed, in the
sagittal plane, between the plane of reference
and the slope of the anterior guide table, as
viewed in the sagittal plane](https://image.slidesharecdn.com/occlusionindentistry-210615051045/85/Occlusion-in-dentistry-51-320.jpg)