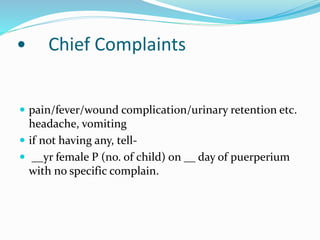
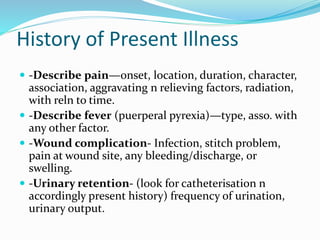
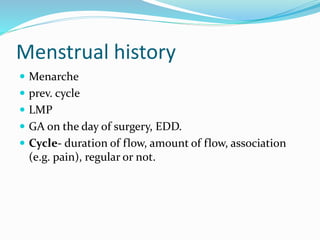
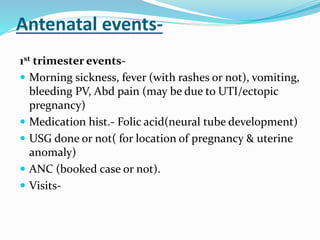
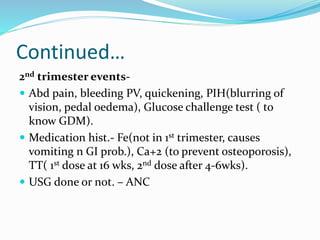
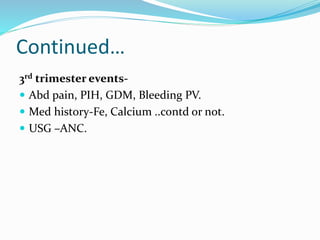
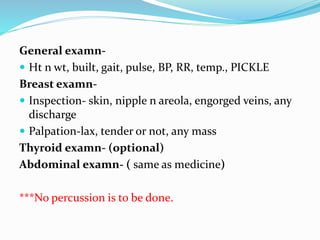
This document outlines the components and considerations for taking a thorough obstetric history. It details sections to cover such as chief complaints, history of present illness, past medical history, menstrual history, obstetric history including details of previous pregnancies, deliveries and puerperiums, antenatal events separated by trimester, labour events, puerperal events, fetal outcome, and physical examination guidelines. The goal is to obtain a comprehensive history addressing any current issues or complications as well as past medical, surgical, menstrual, pregnancy, delivery and postpartum health to properly evaluate and manage the patient's care.