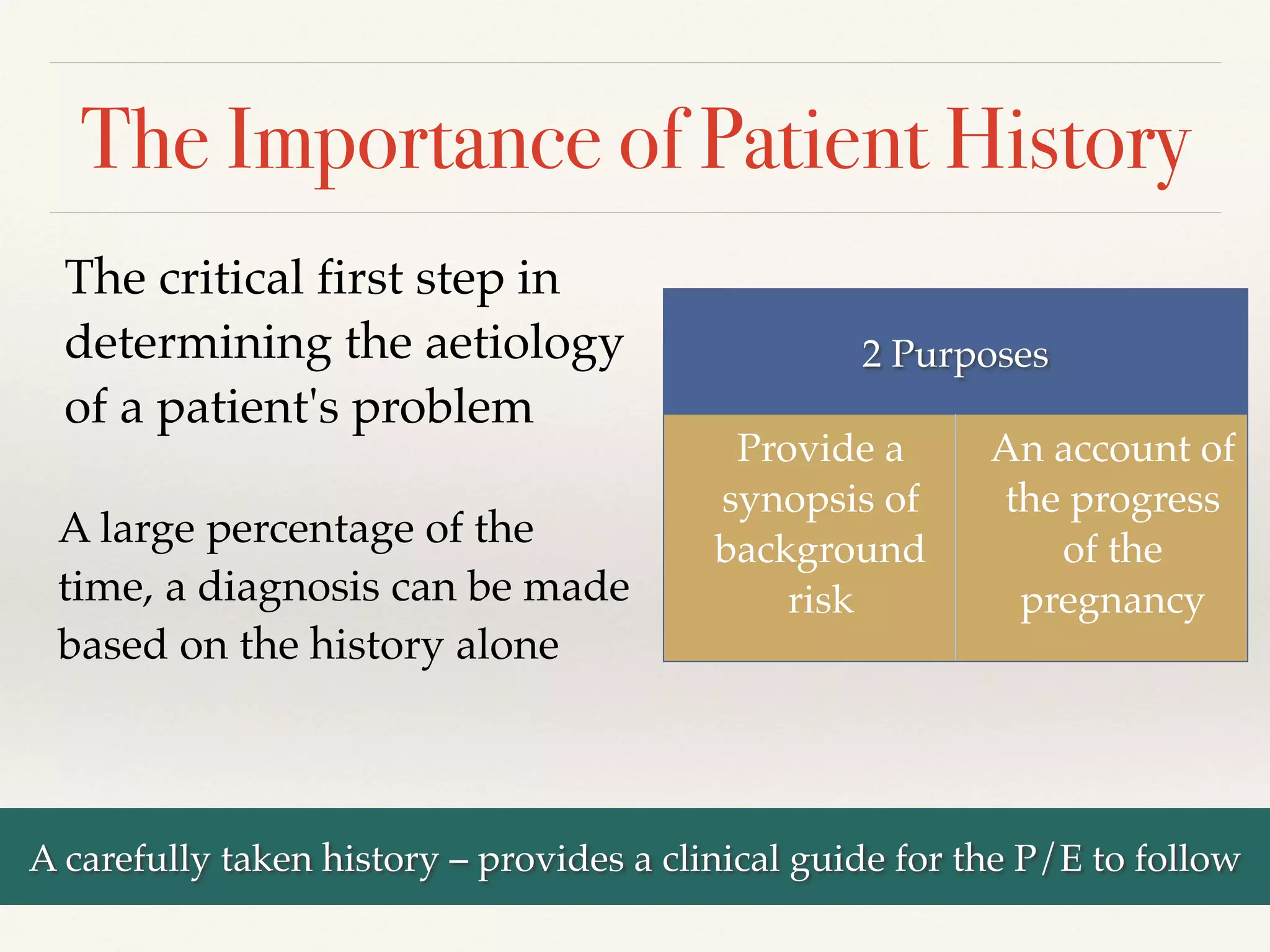
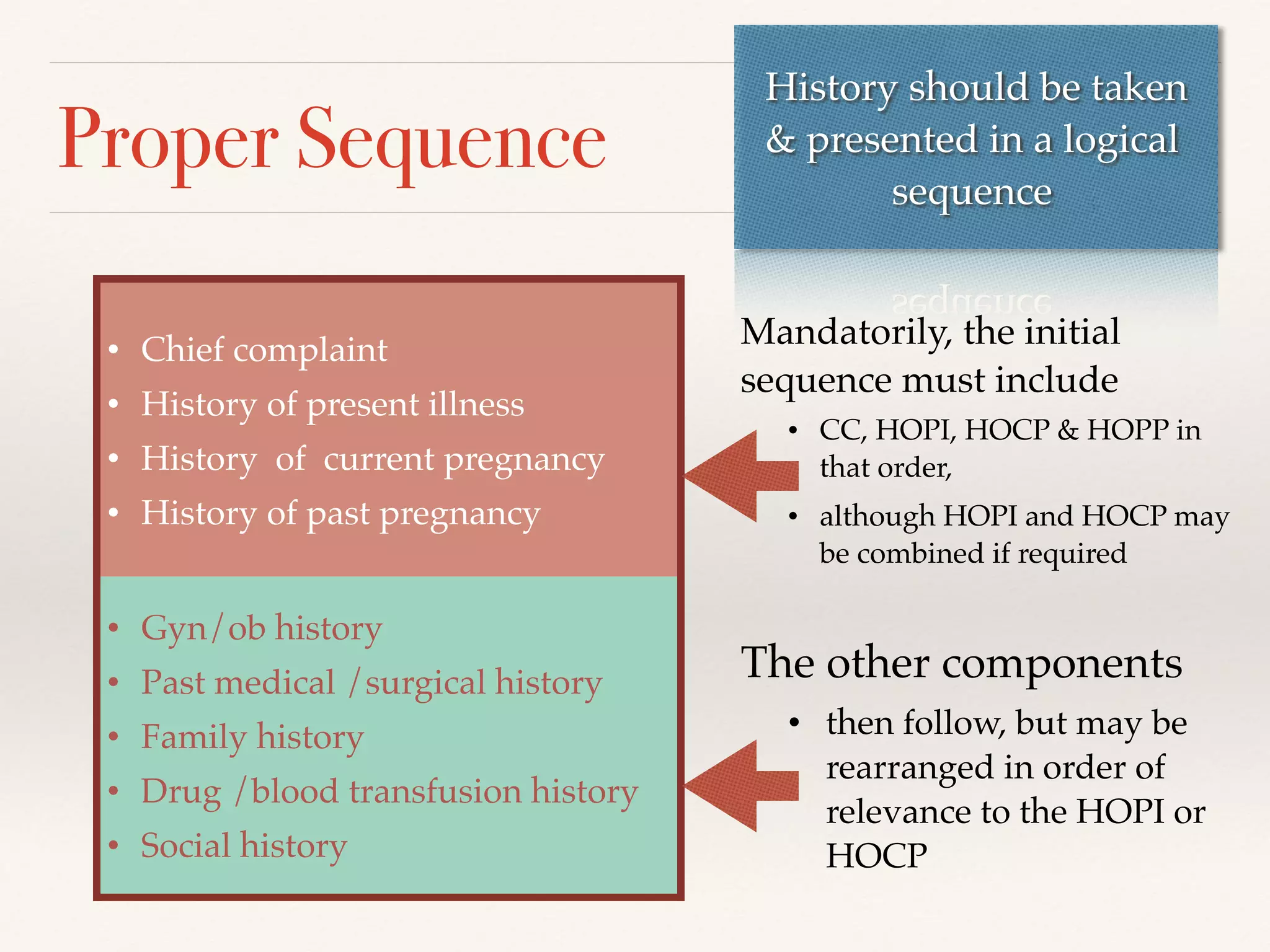
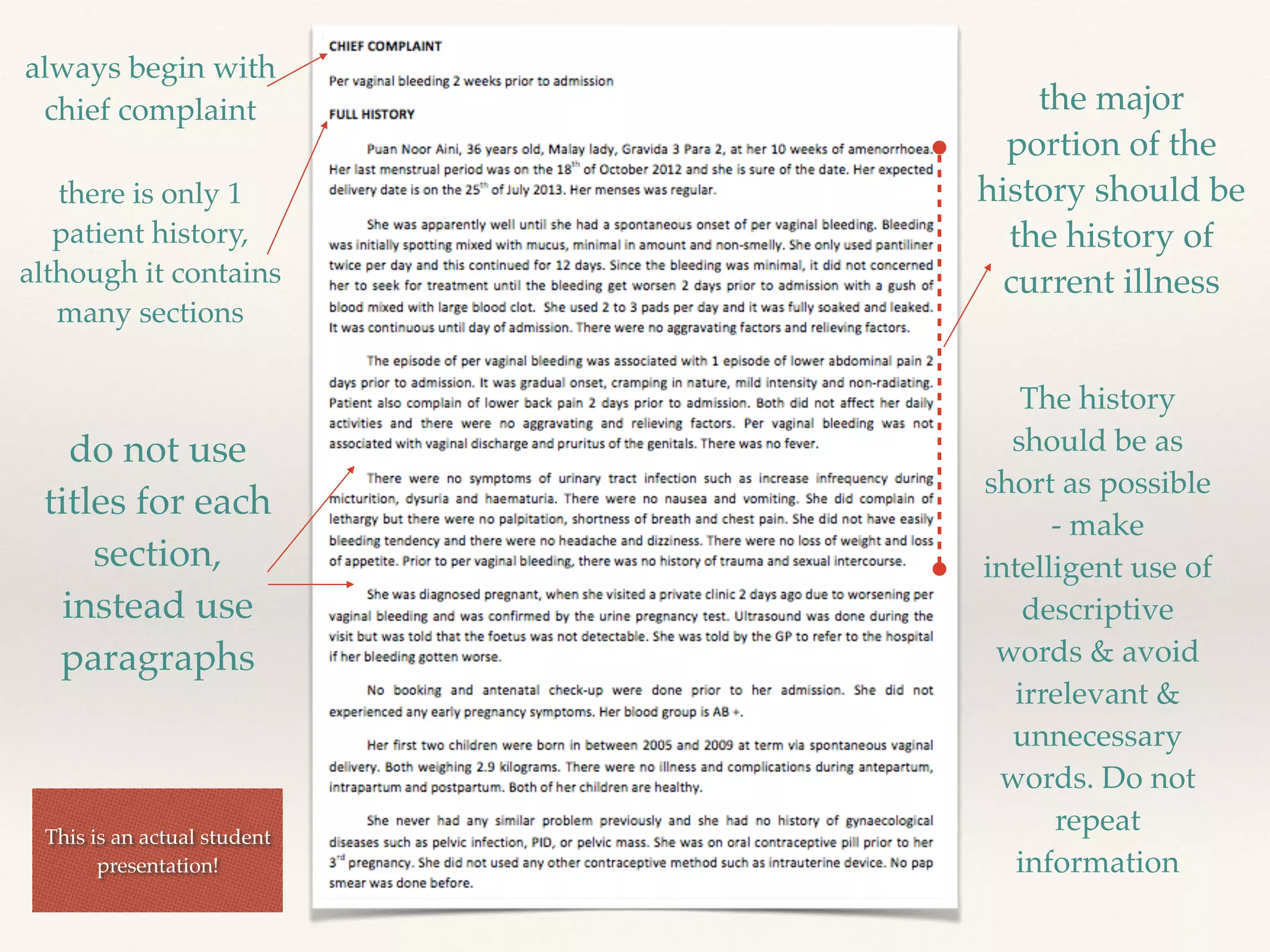
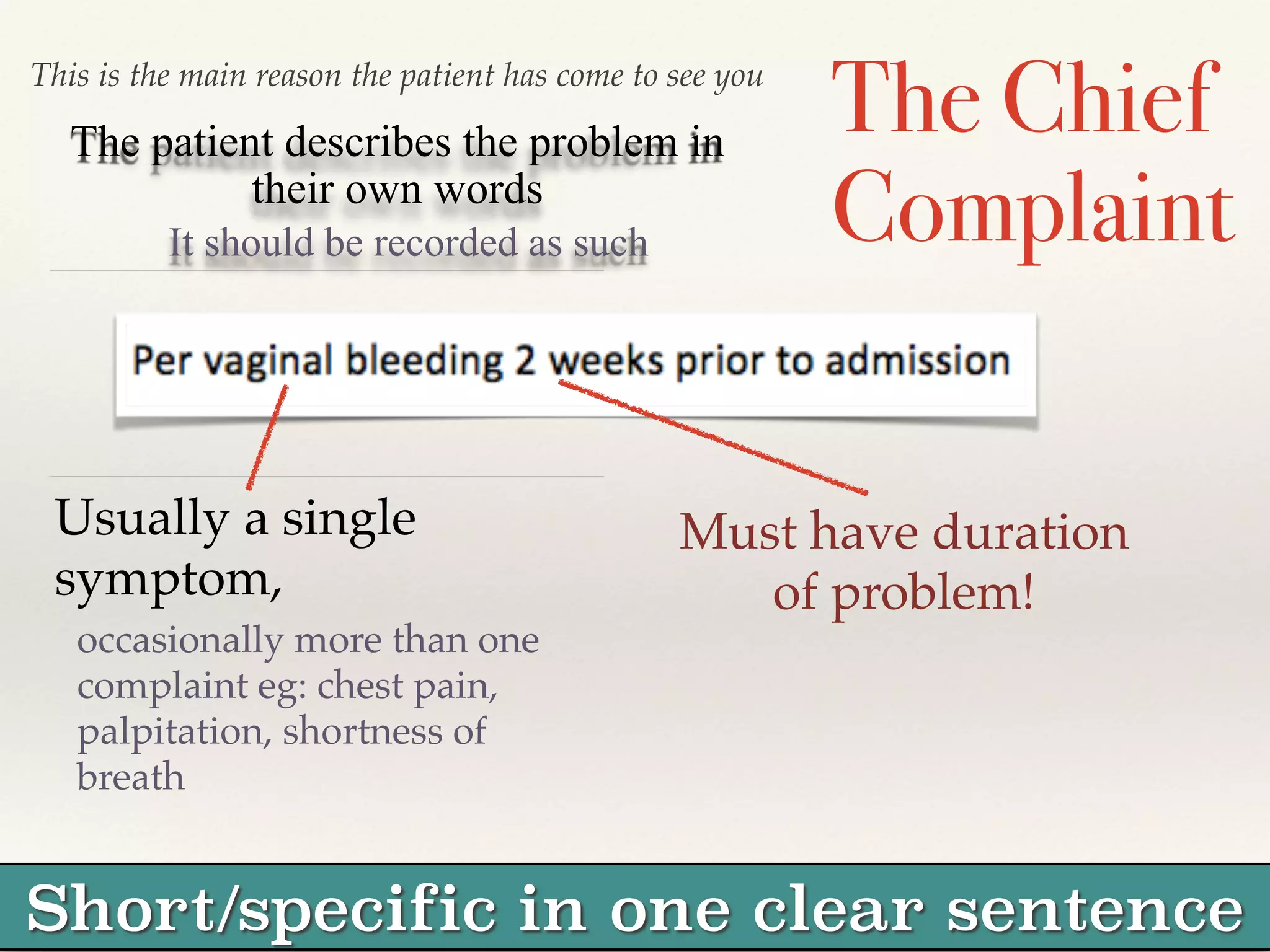
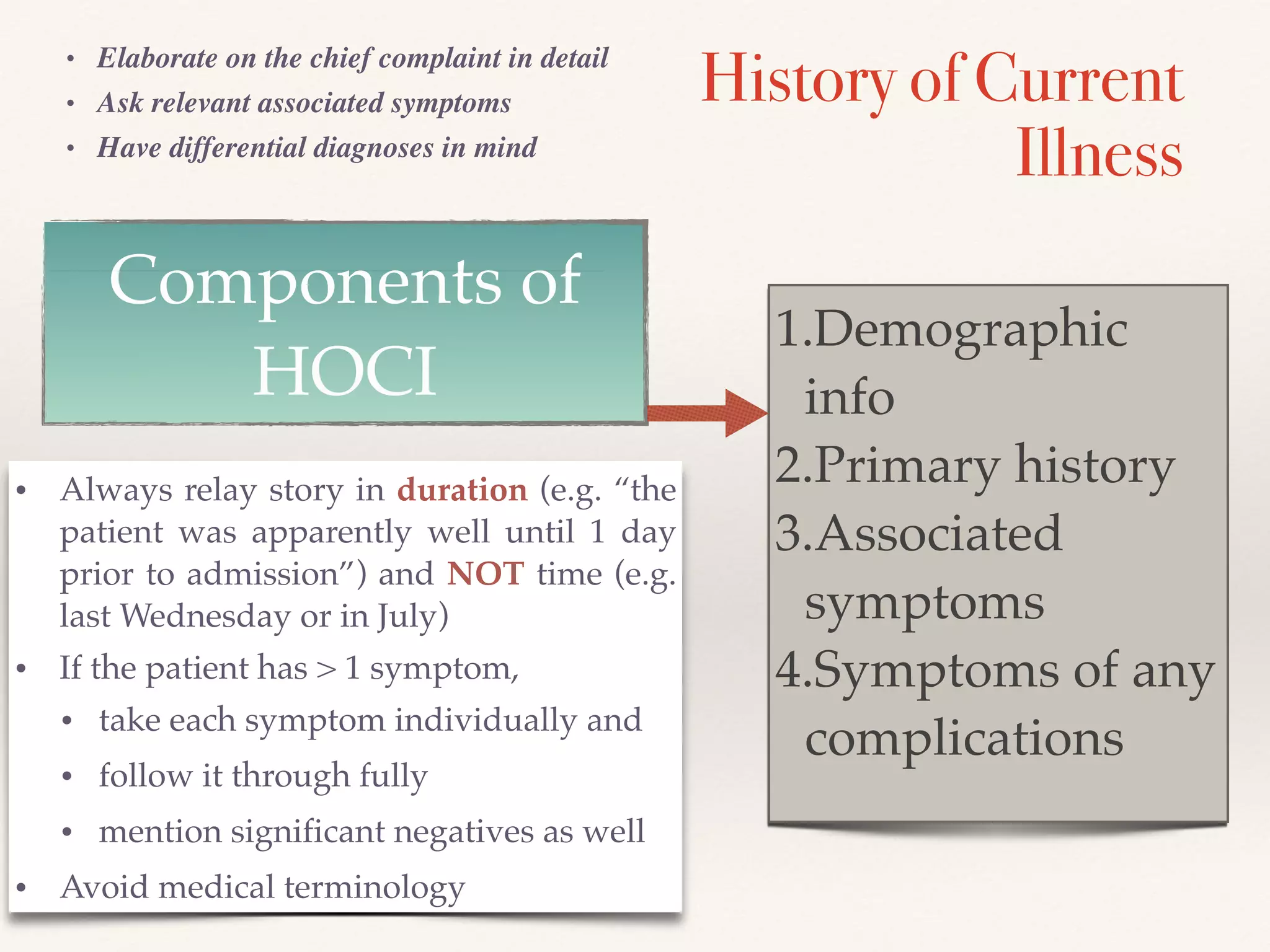
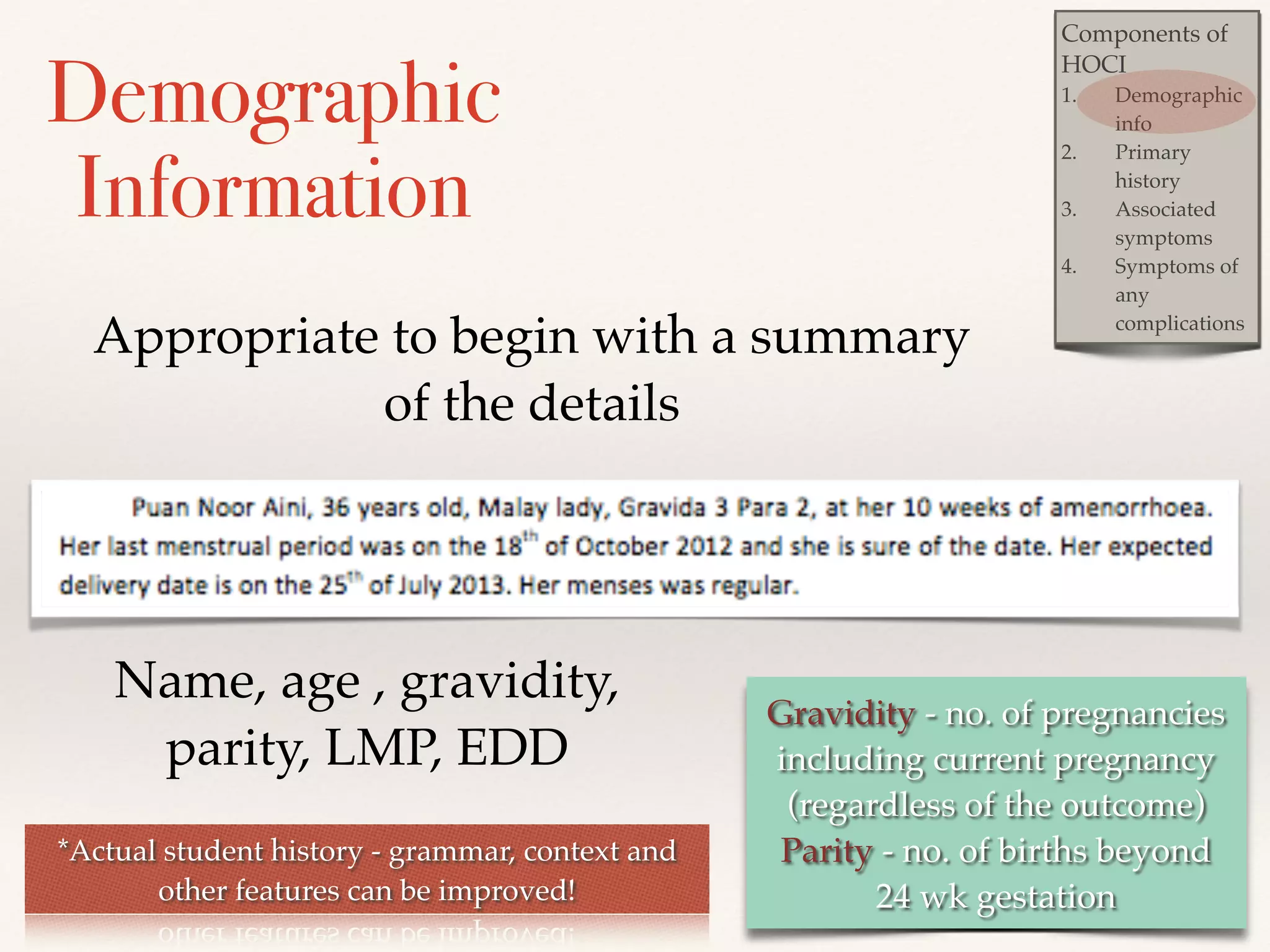
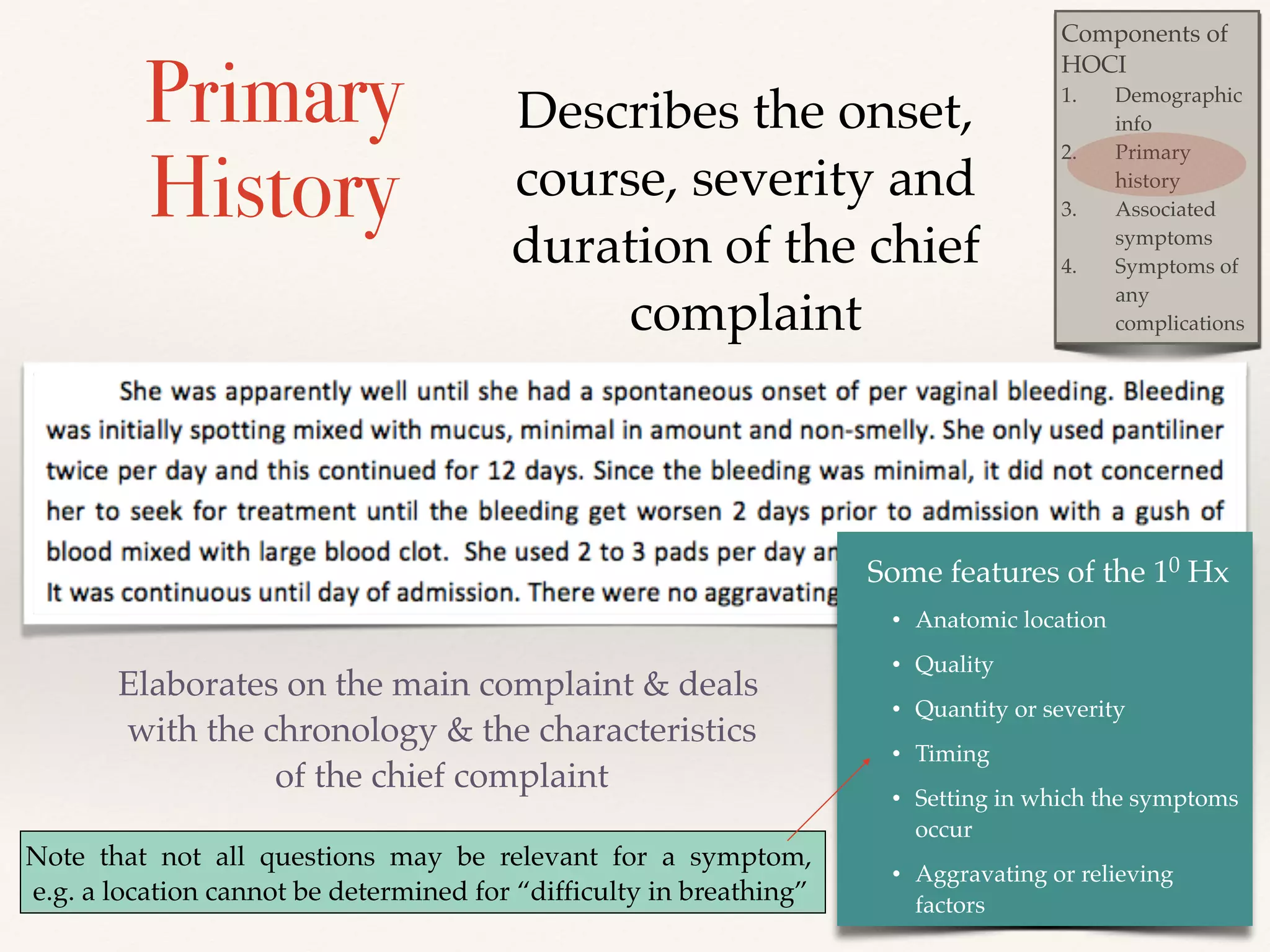
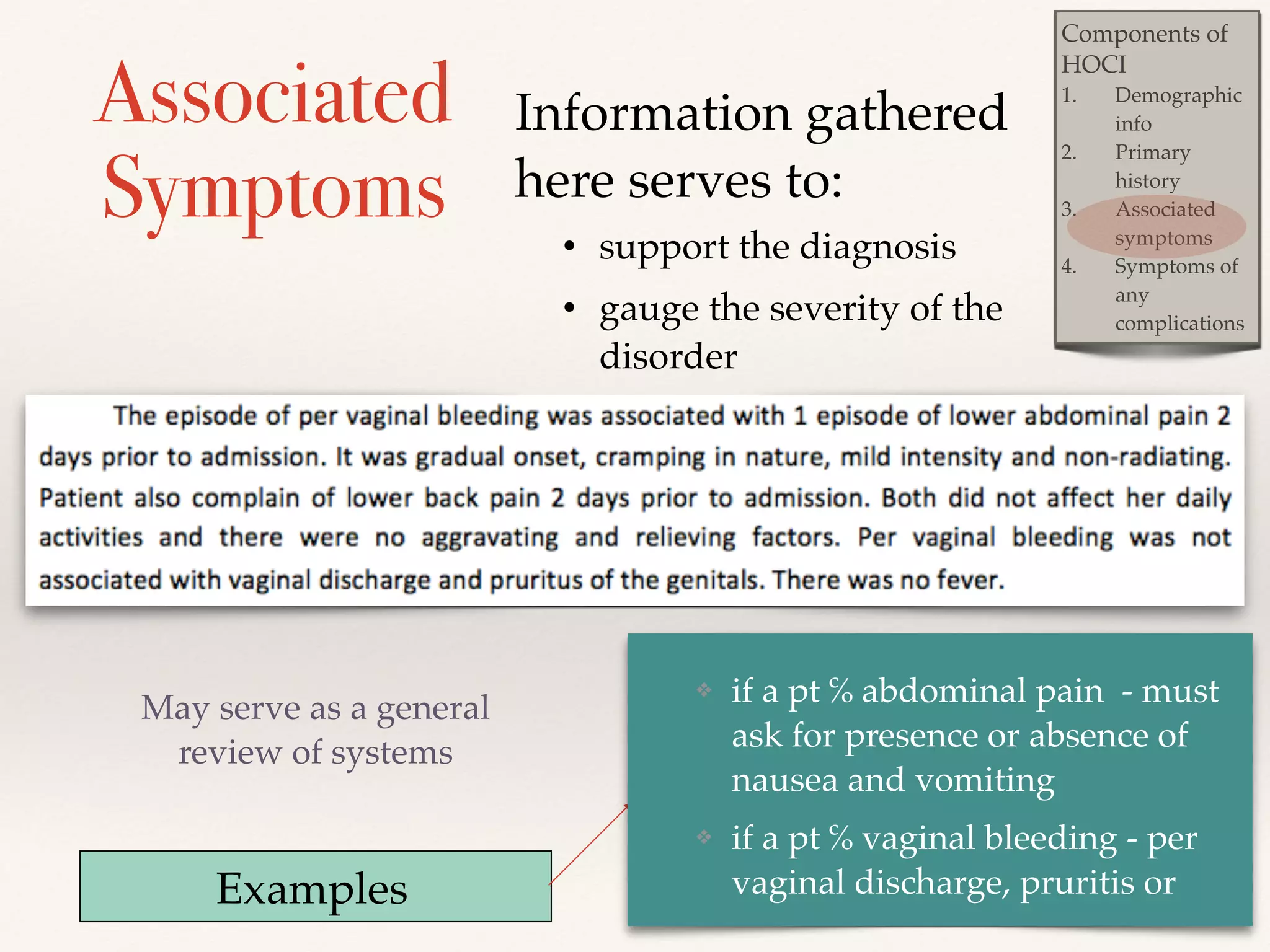
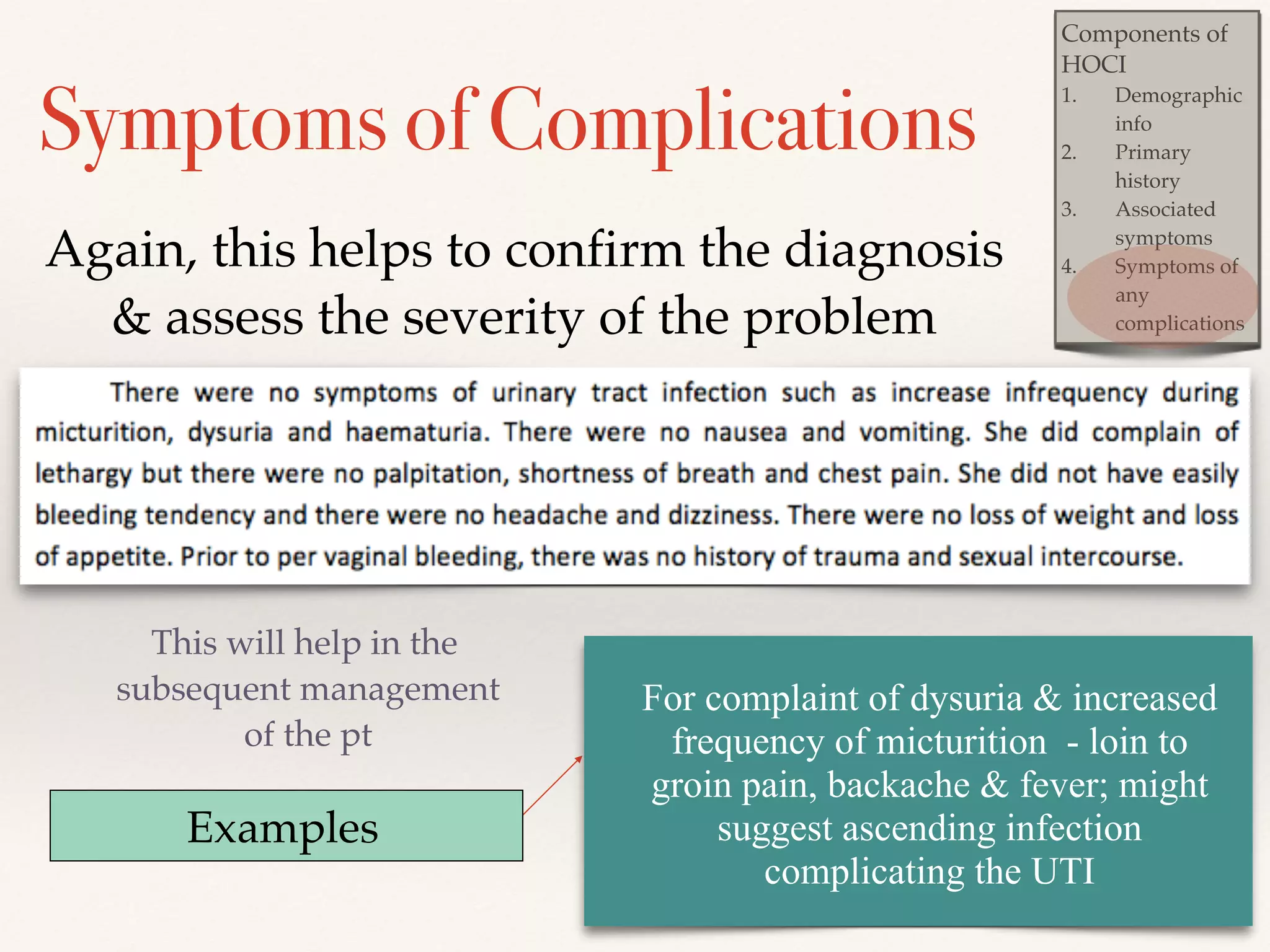
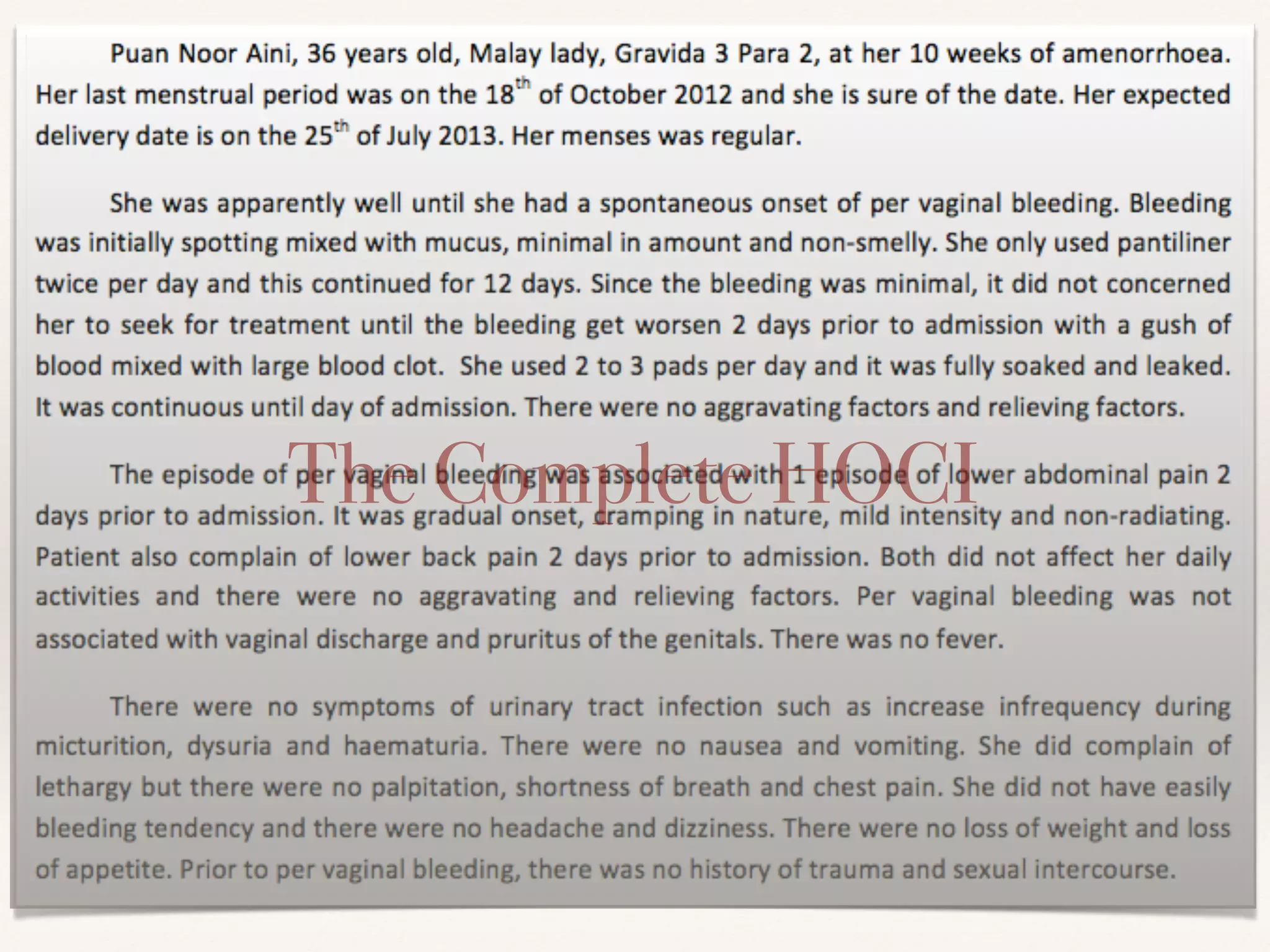
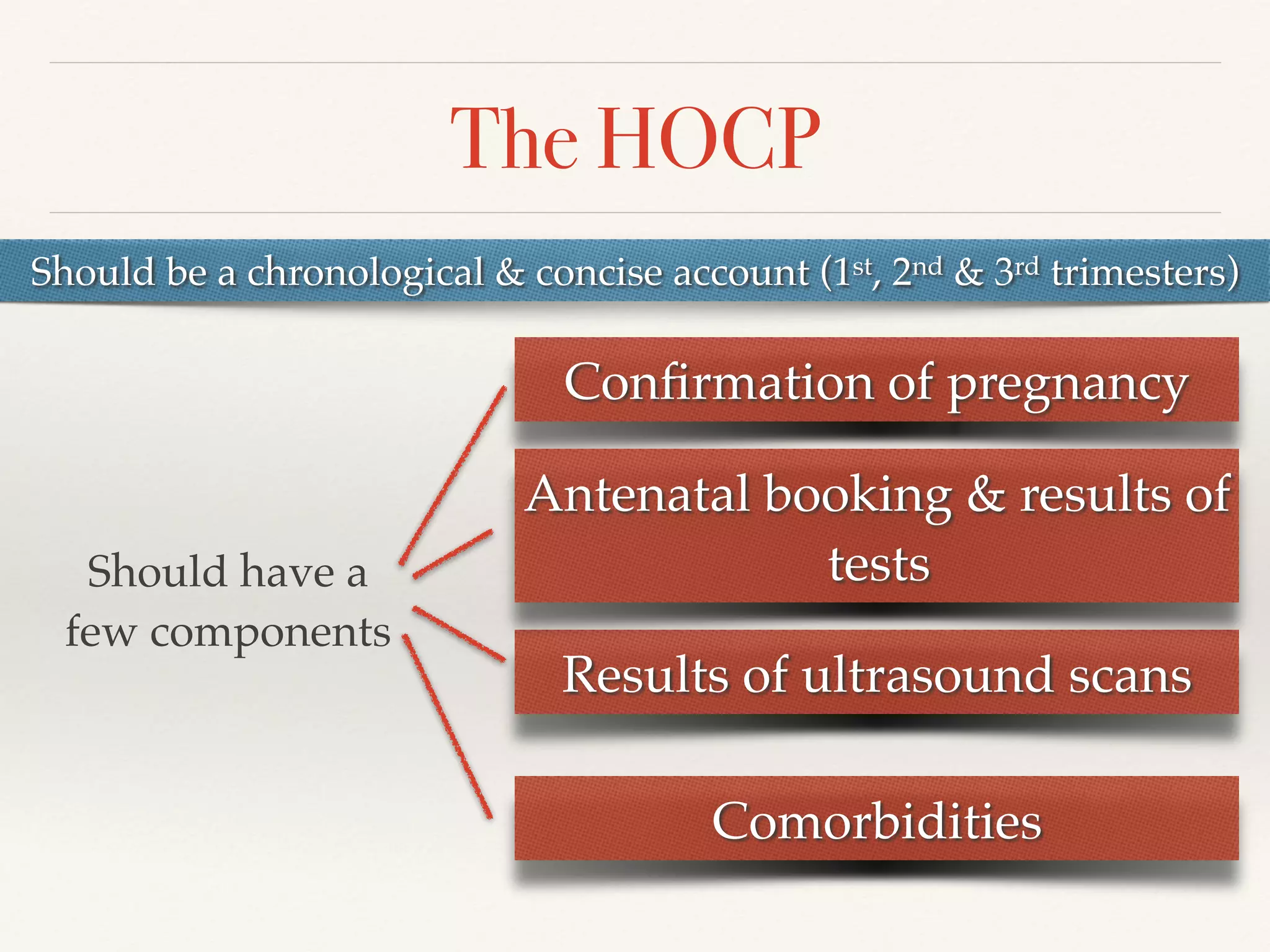
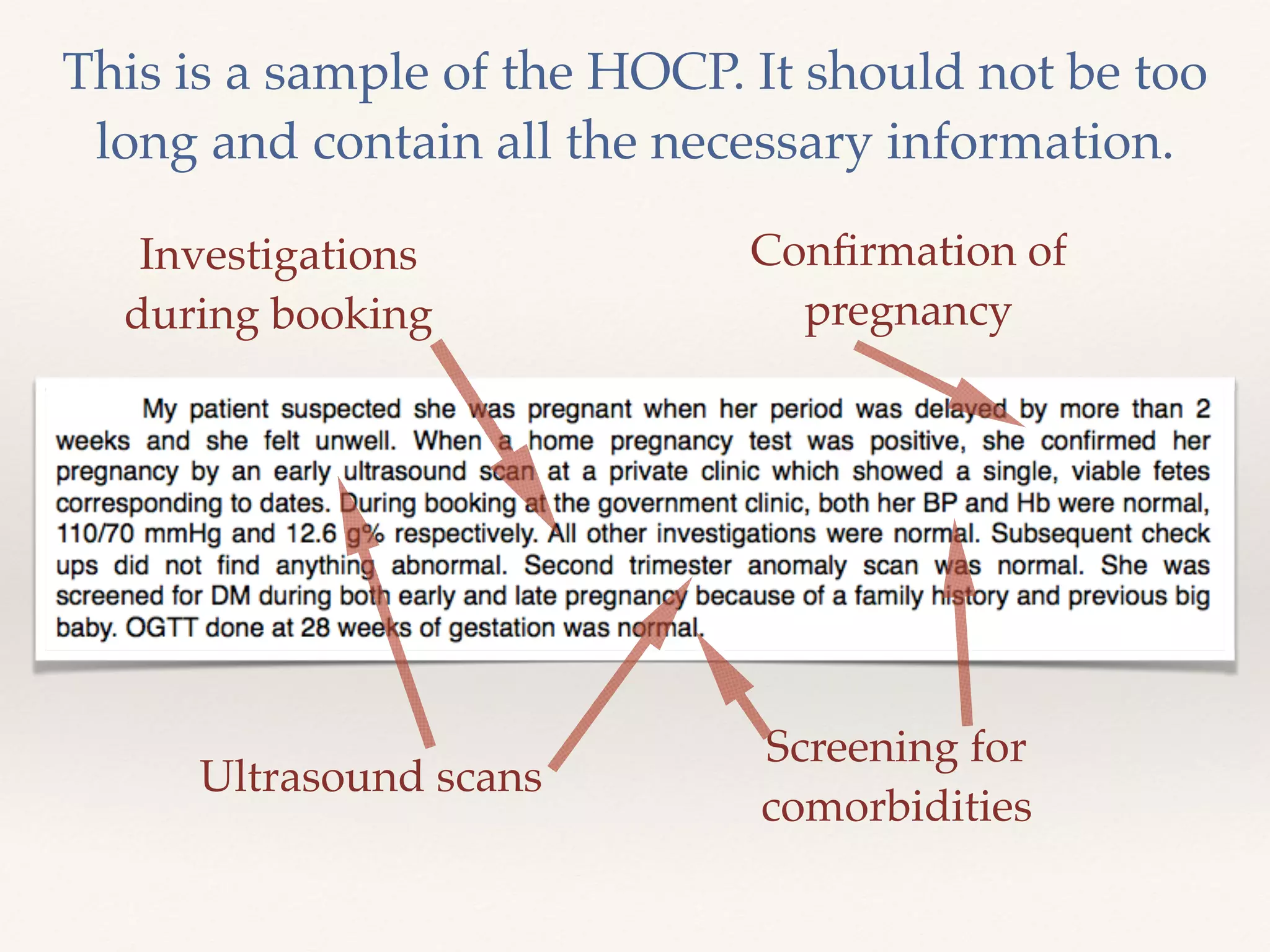
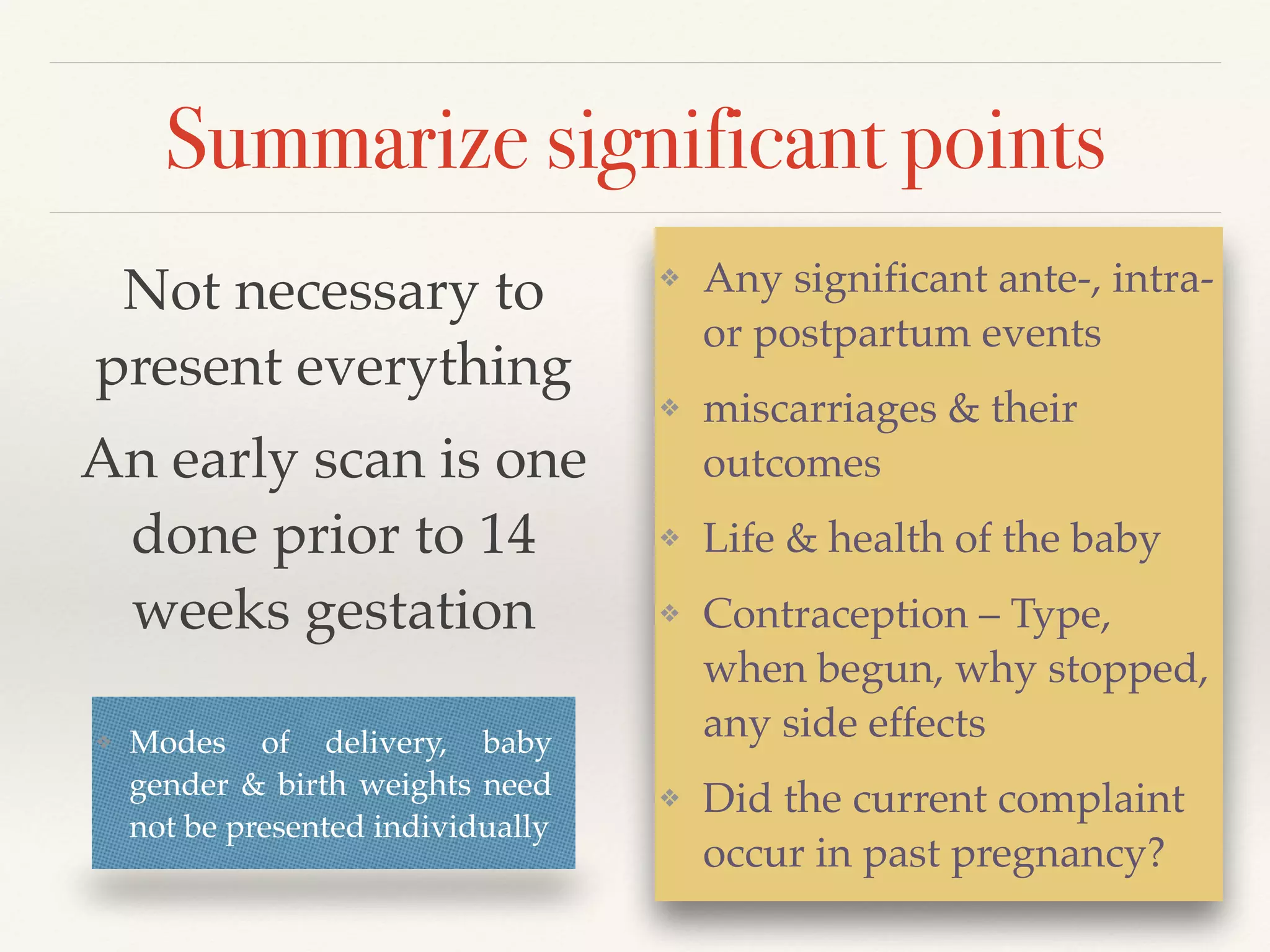
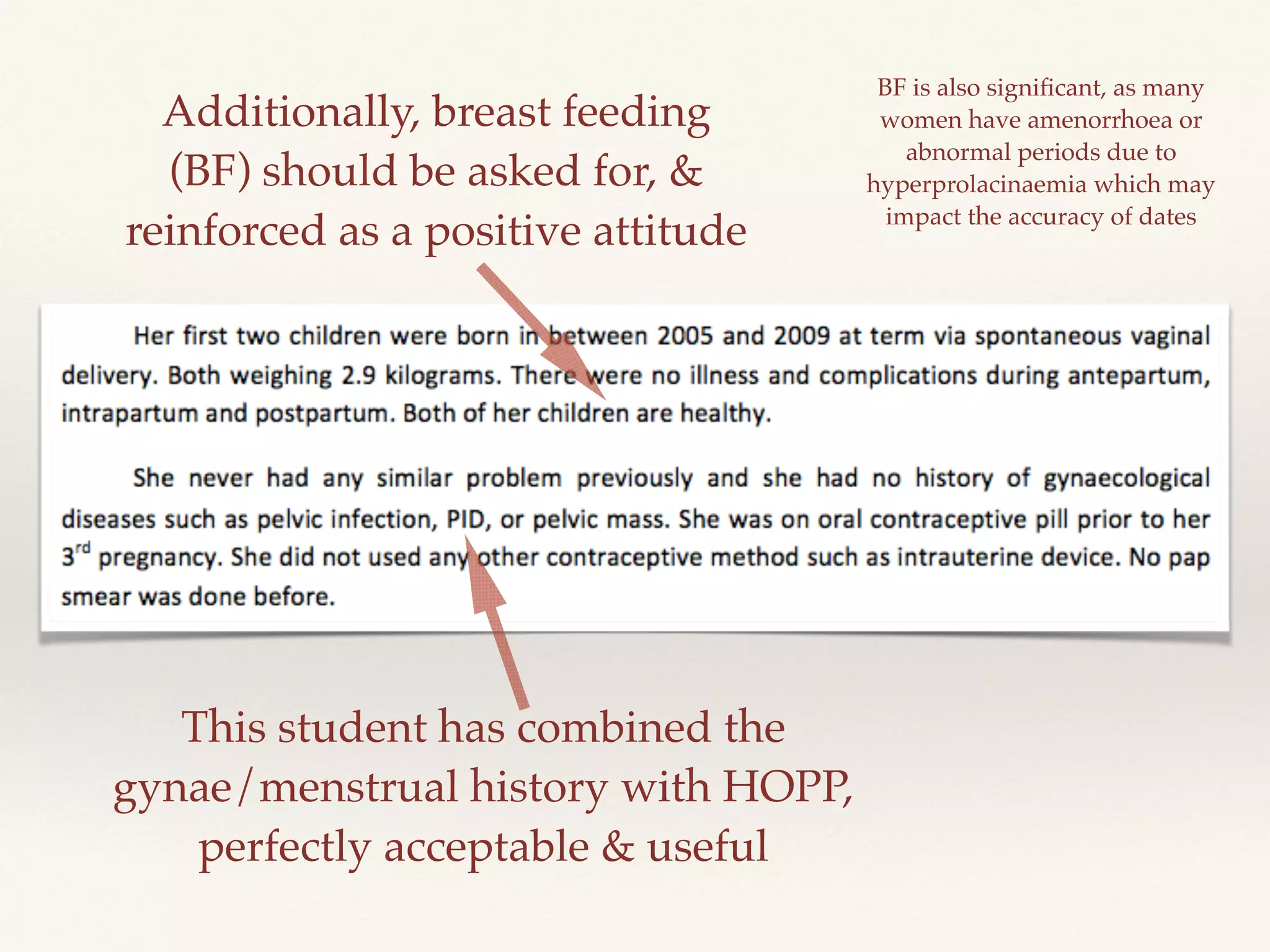
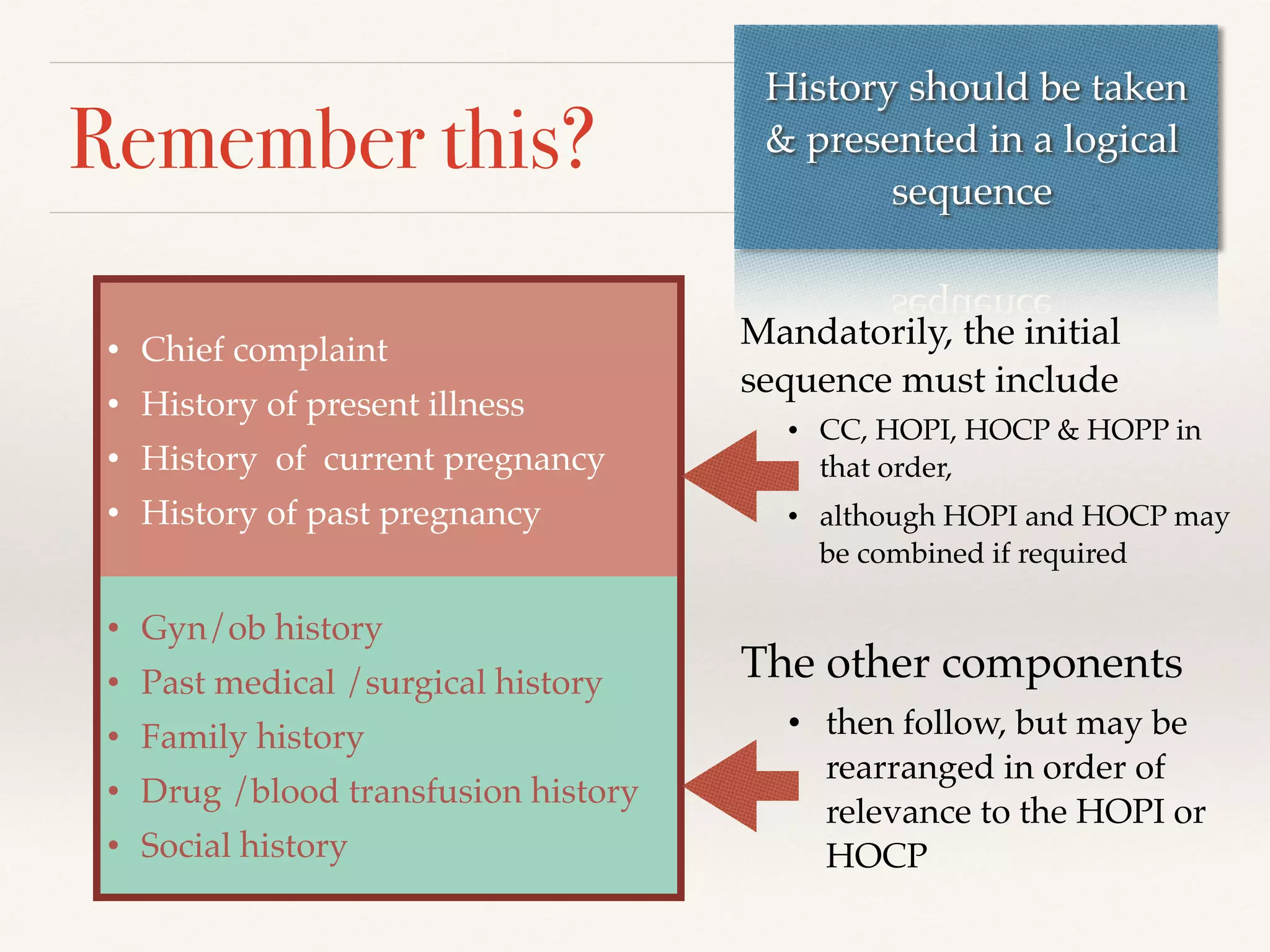
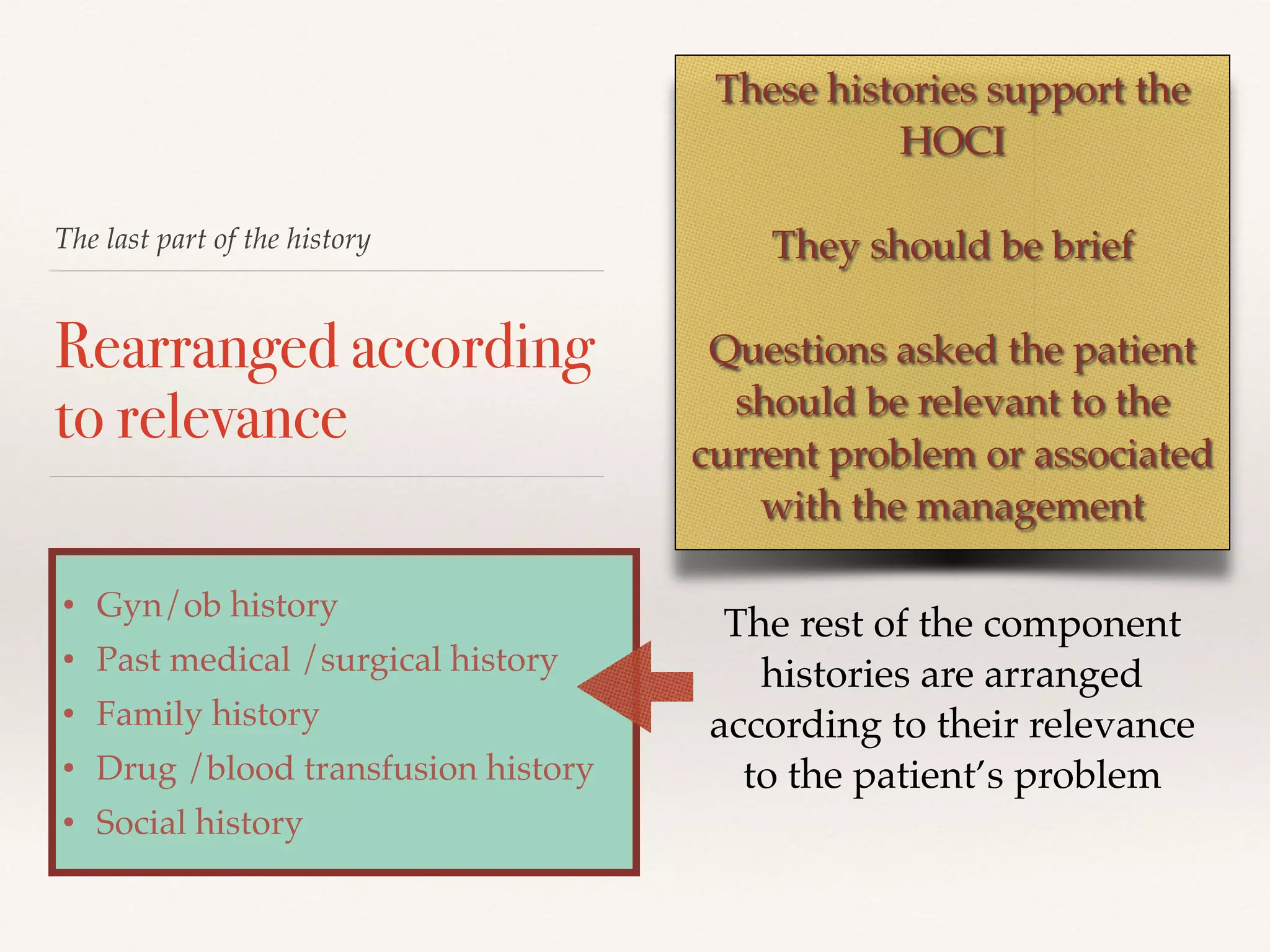
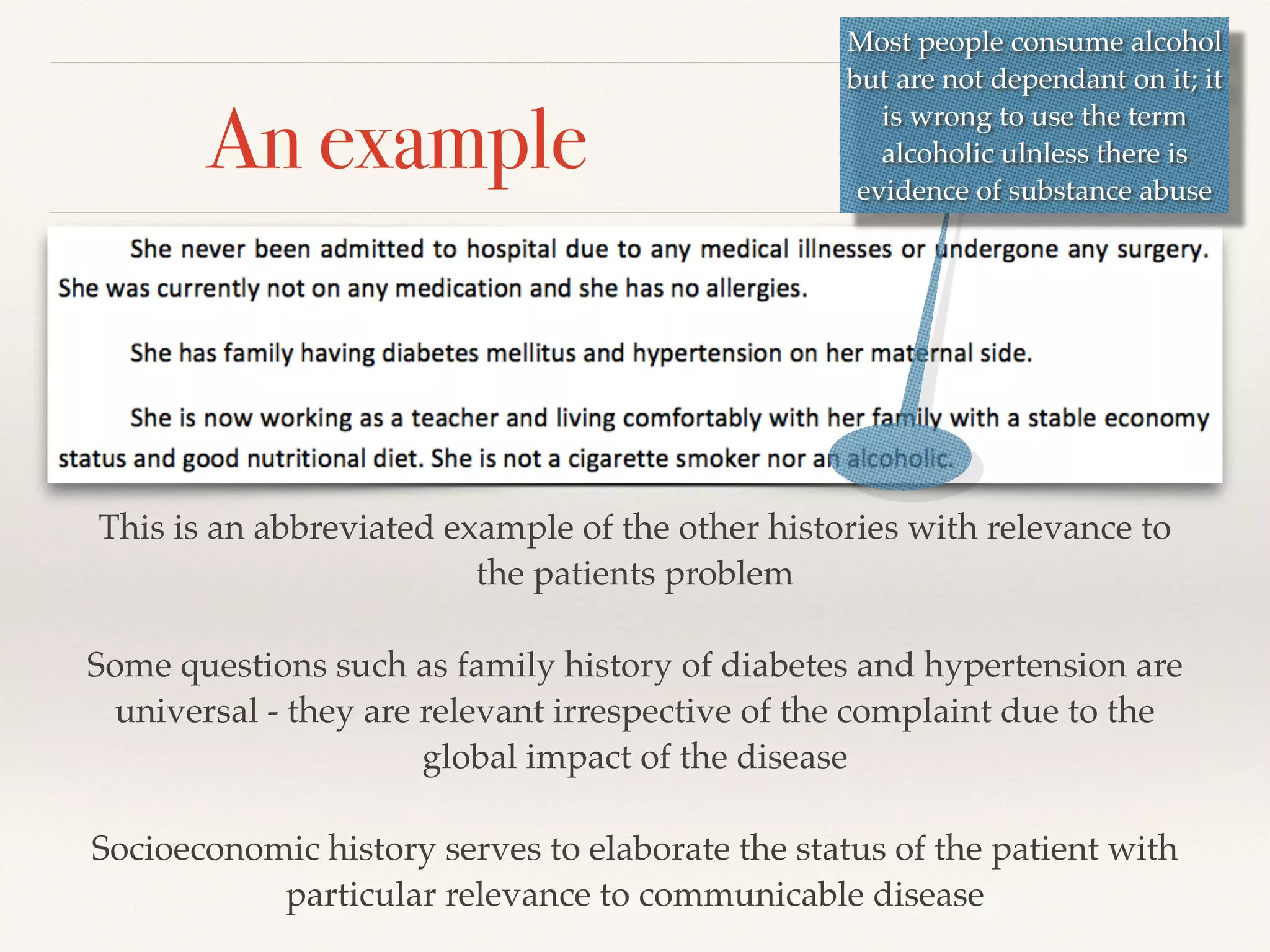
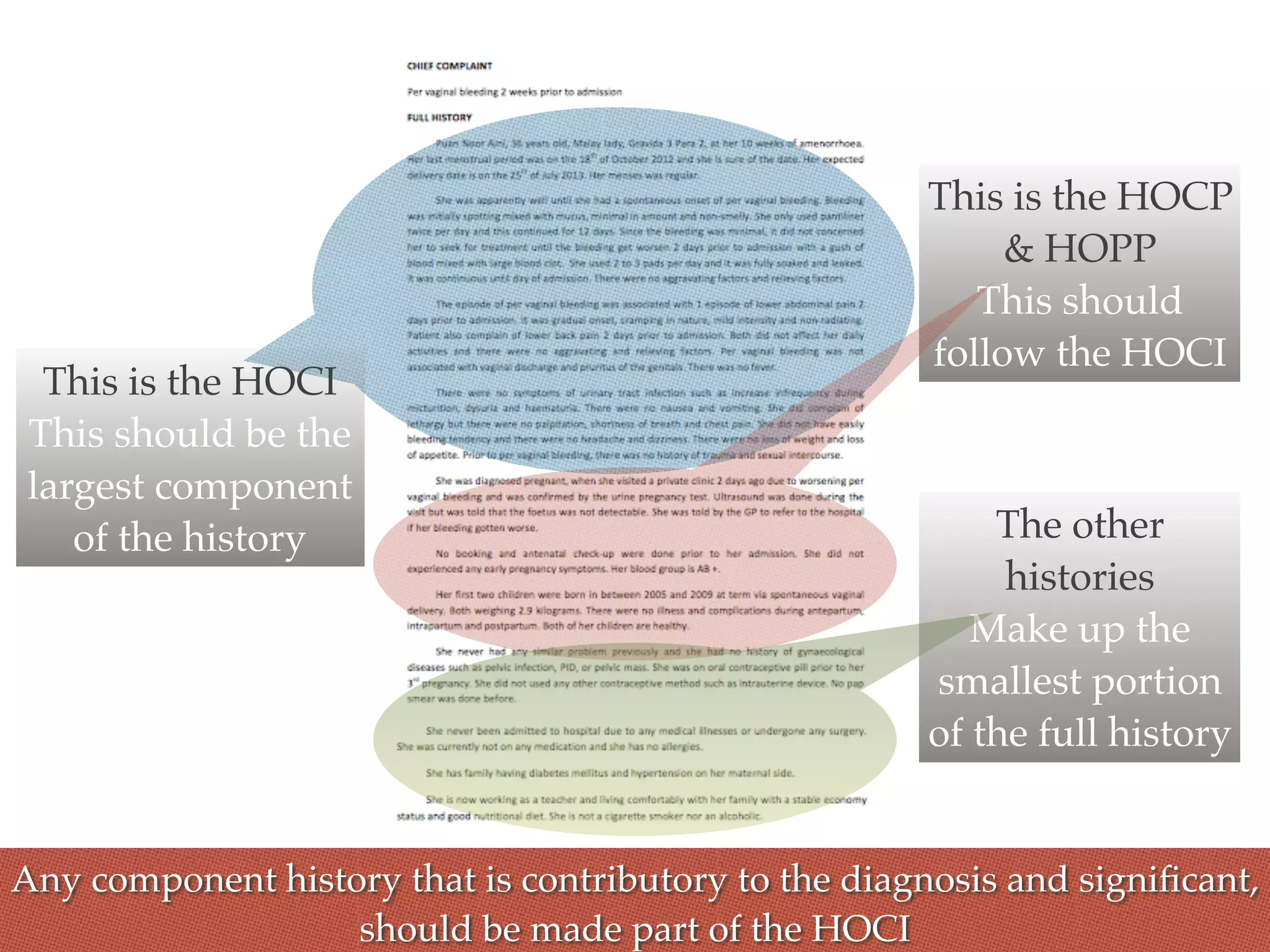
The document serves as a comprehensive guide for presenting obstetric history in a clinical setting, emphasizing the crucial role of a well-taken patient history in diagnosing issues. It outlines the logical sequence of components to include, such as chief complaint, history of present illness, and past pregnancies, while highlighting the importance of conciseness and relevance in documentation. Additionally, it details the necessary assessments and inquiries related to the current pregnancy and any comorbidities, reinforcing the connection between past and current health events.