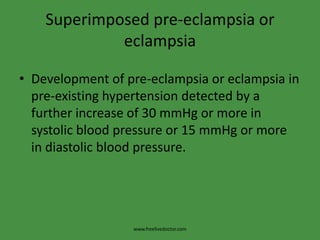
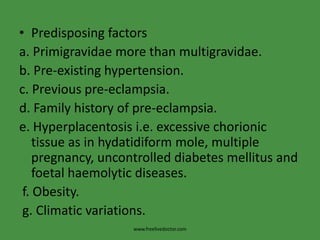
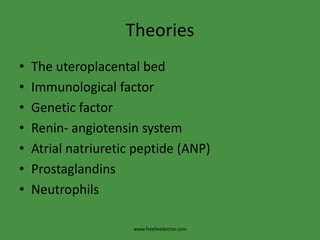
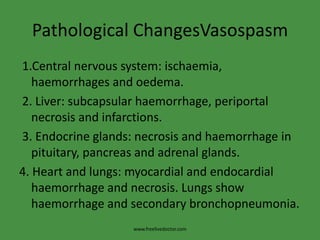
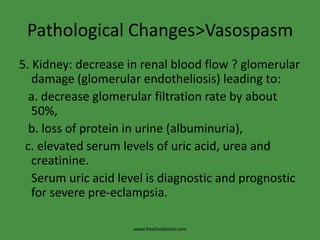
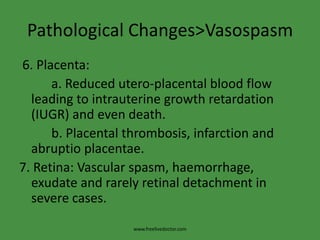
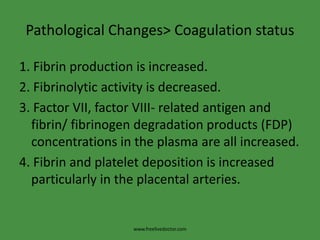
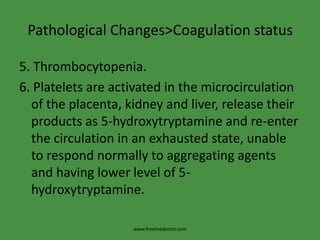
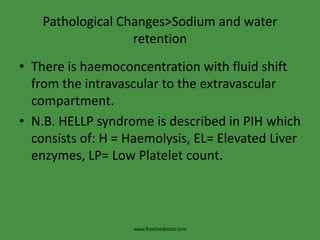
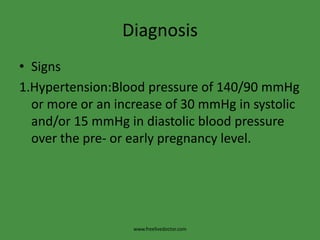
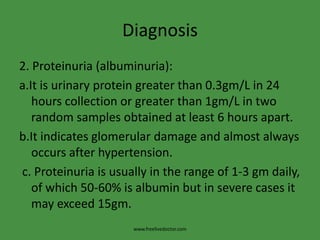
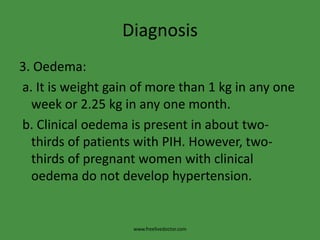
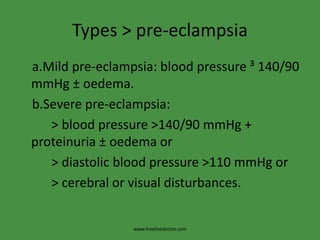
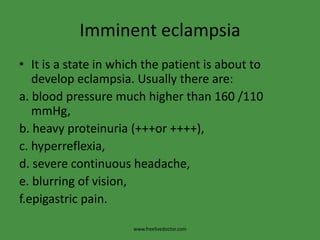
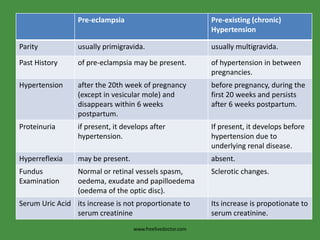
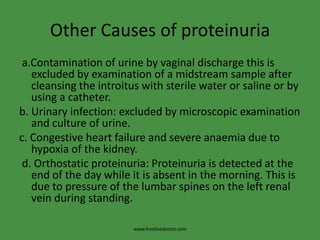
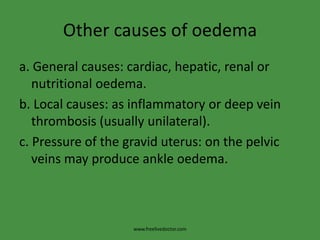
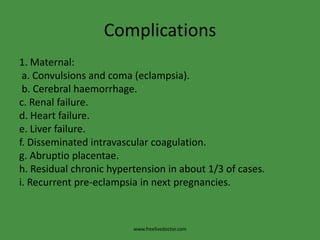
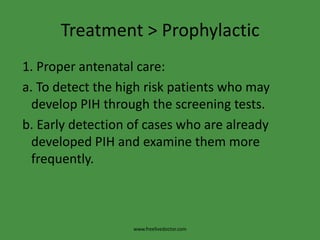
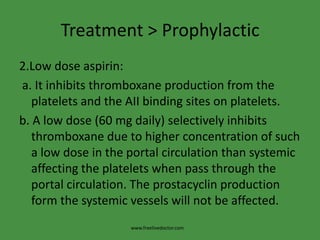
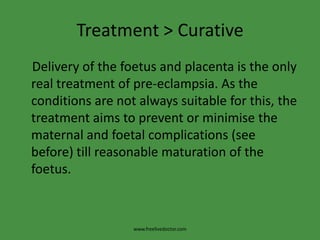
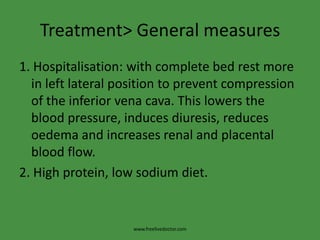
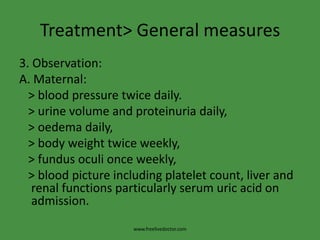
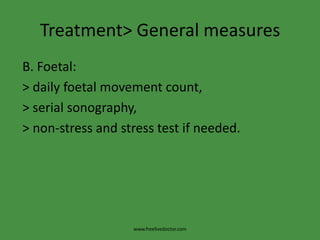
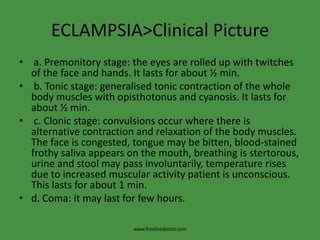
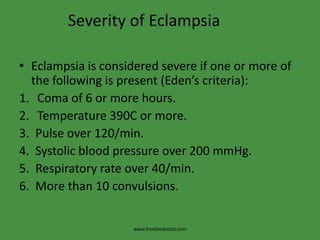
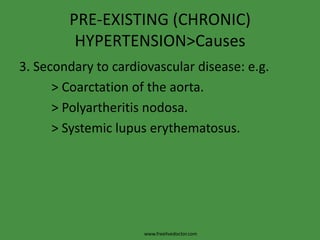
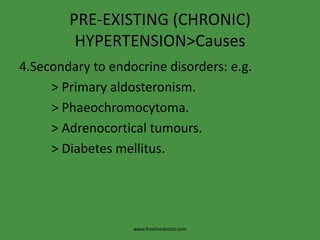
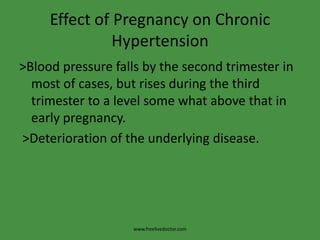
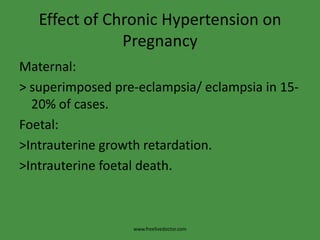
This document discusses hypertensive disorders in pregnancy. It classifies hypertension into pre-existing (chronic) hypertension, pregnancy-induced hypertension (PIH), and superimposed pre-eclampsia/eclampsia. PIH includes transient hypertension, pre-eclampsia, and eclampsia. The document explores various theories of causation and provides details on pathological changes, diagnosis, screening tests, types of pre-eclampsia, complications, and treatment including prophylactic low-dose aspirin.