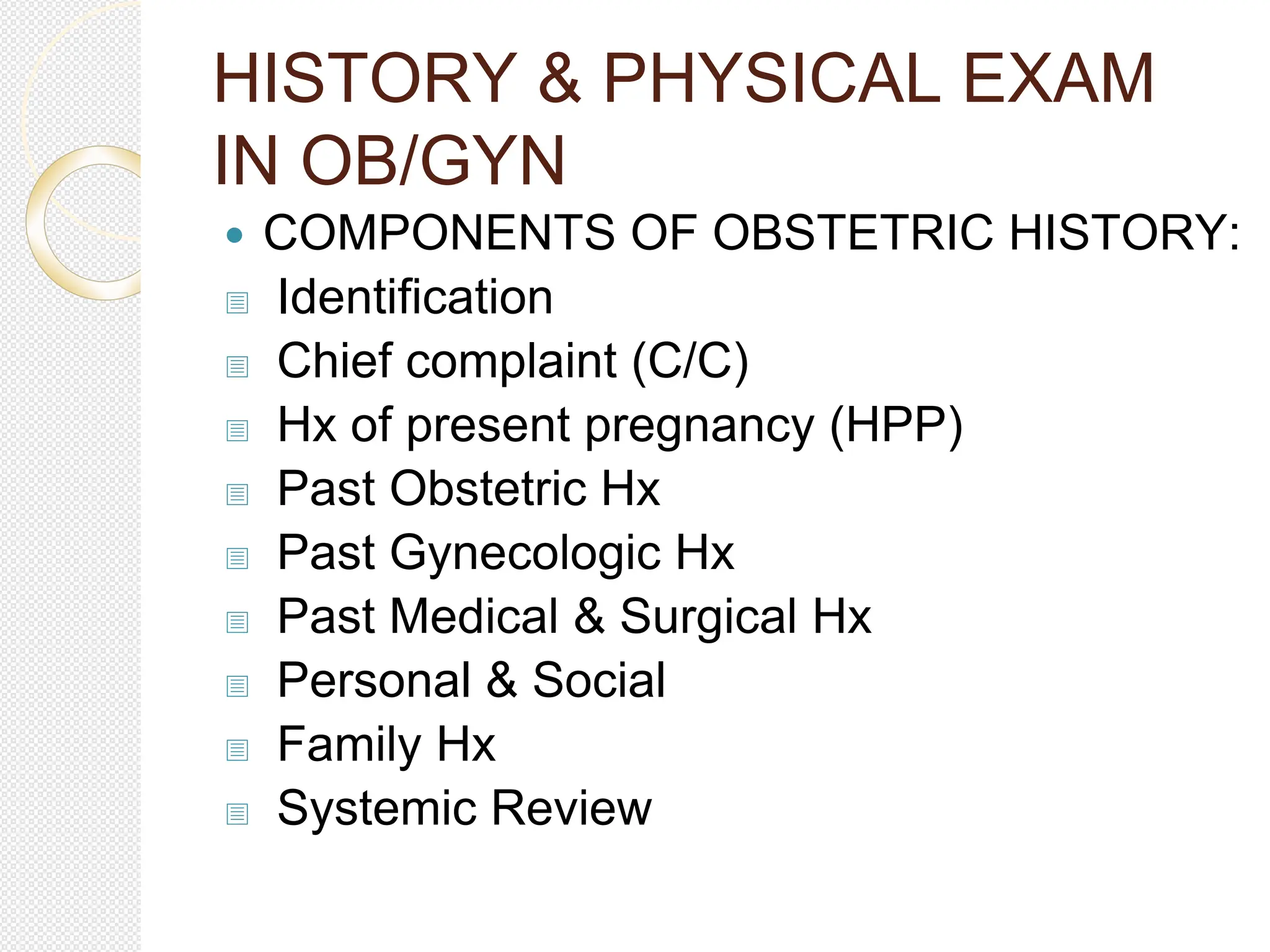
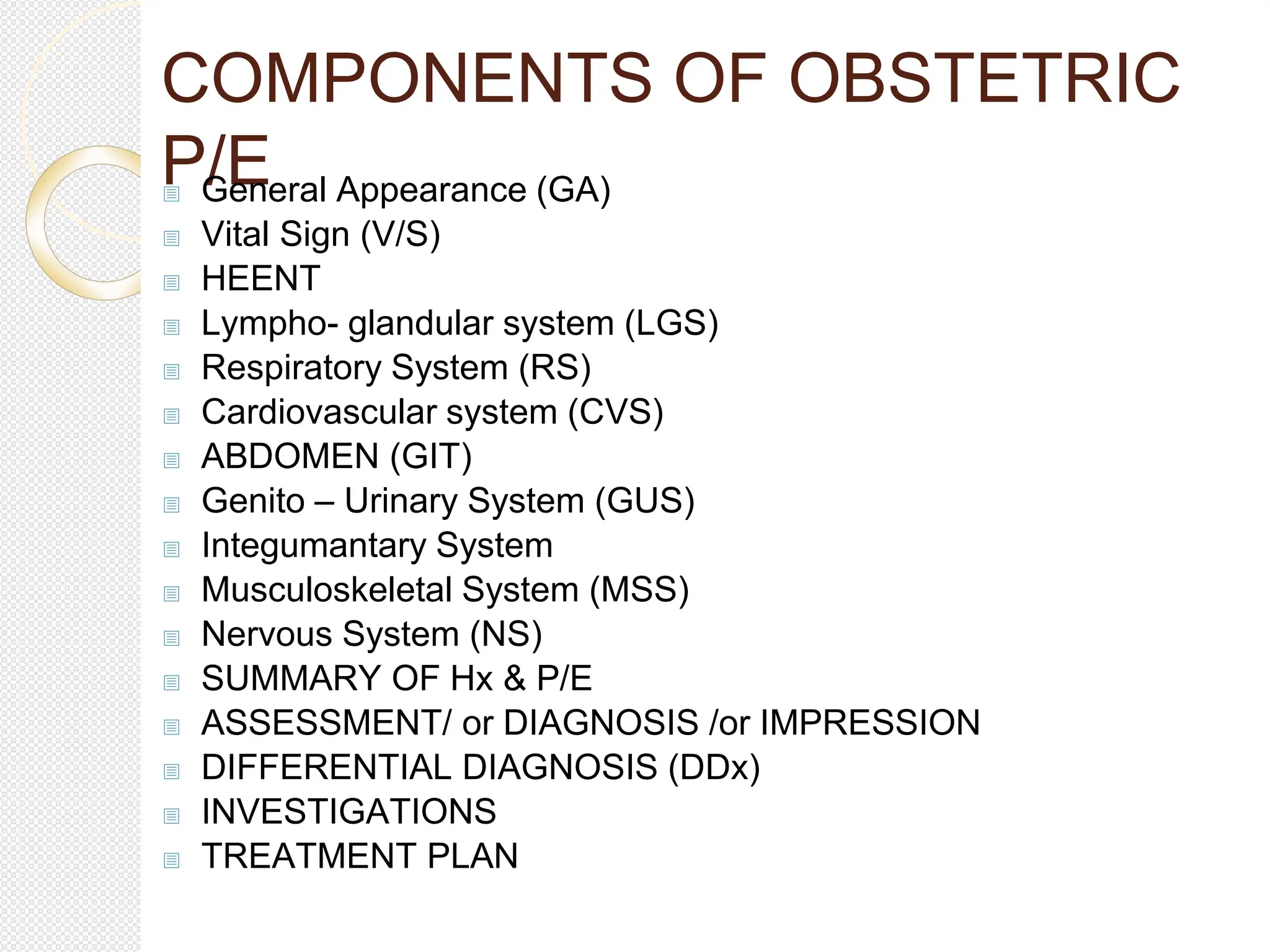
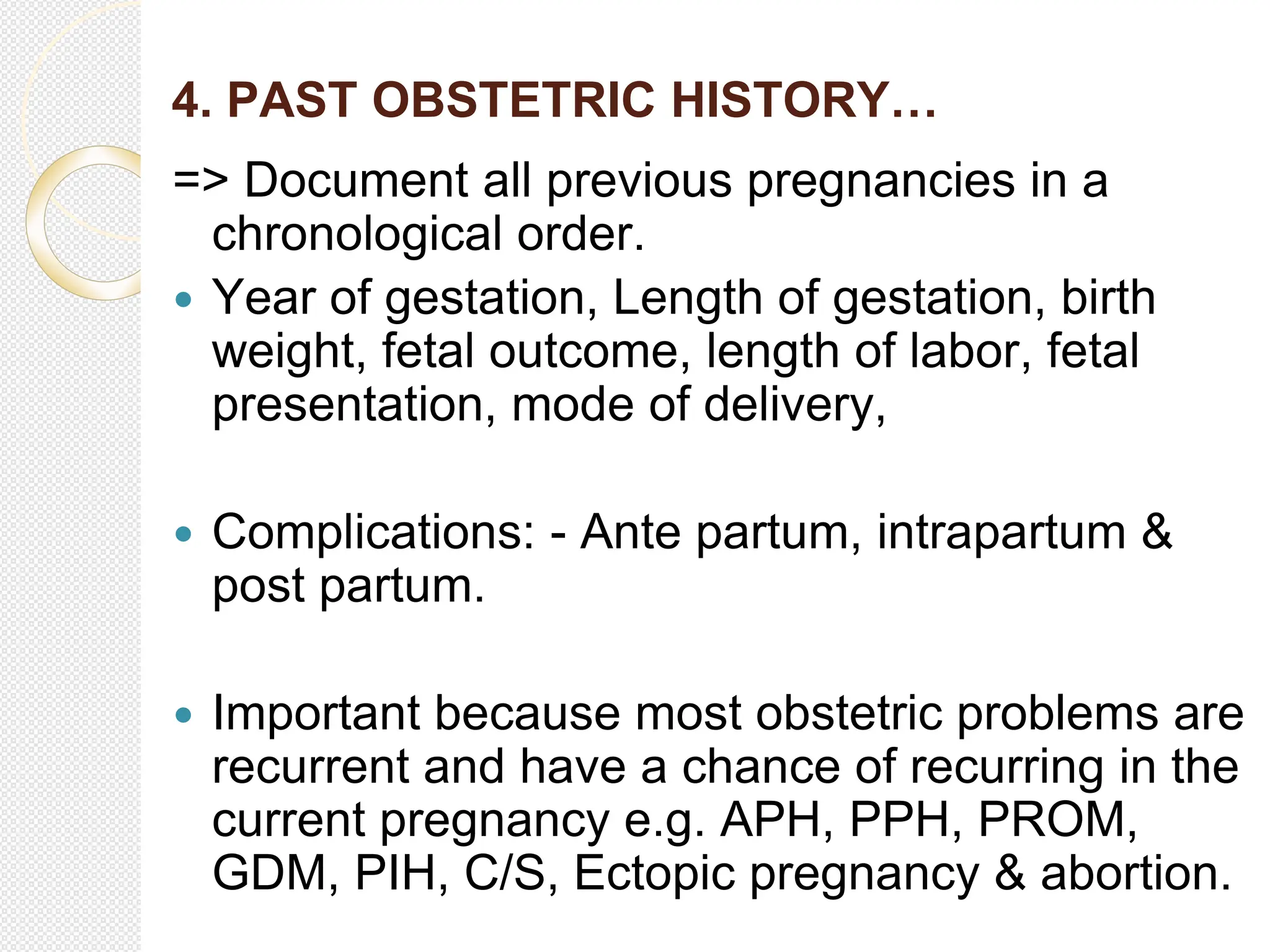
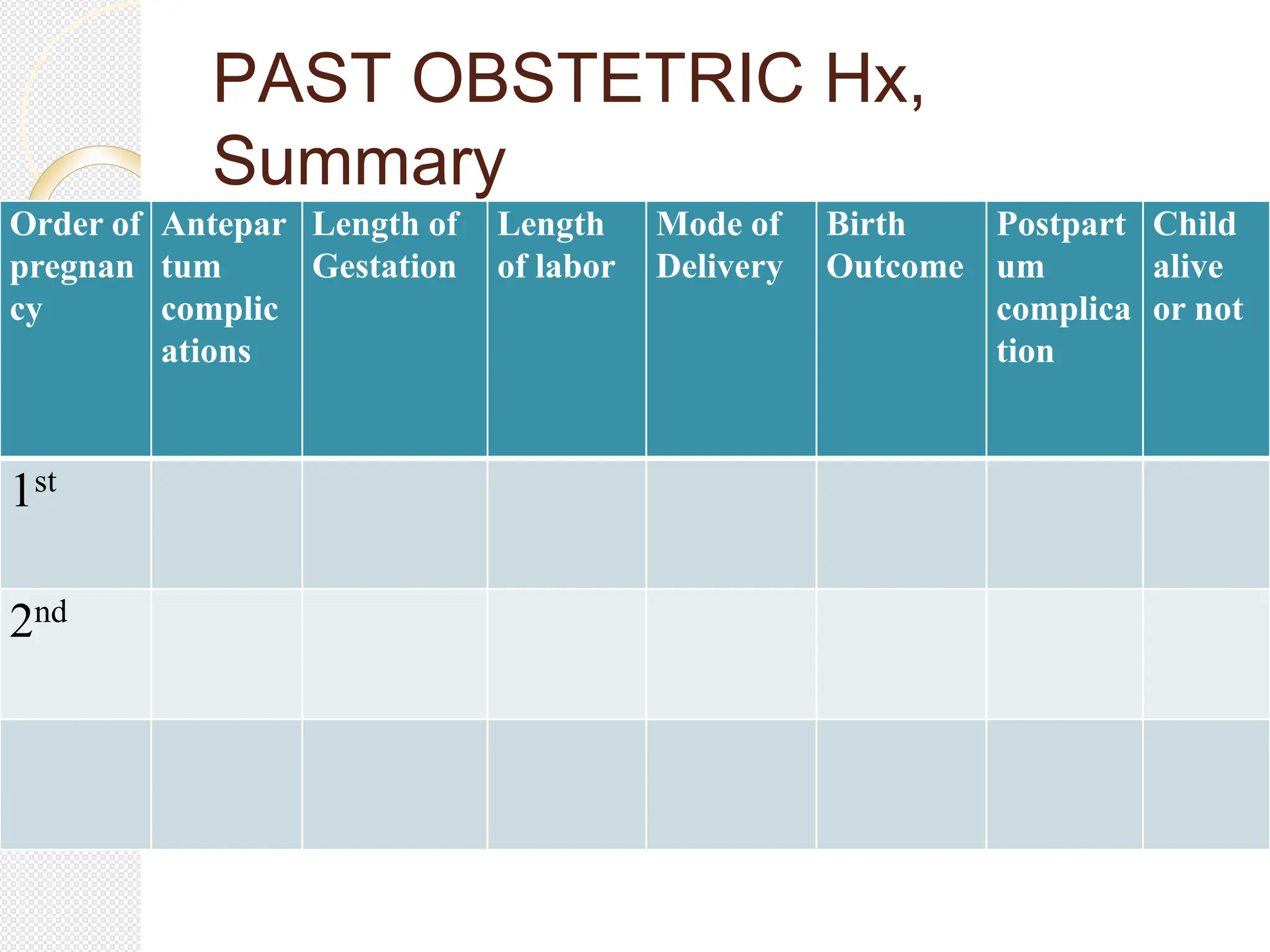
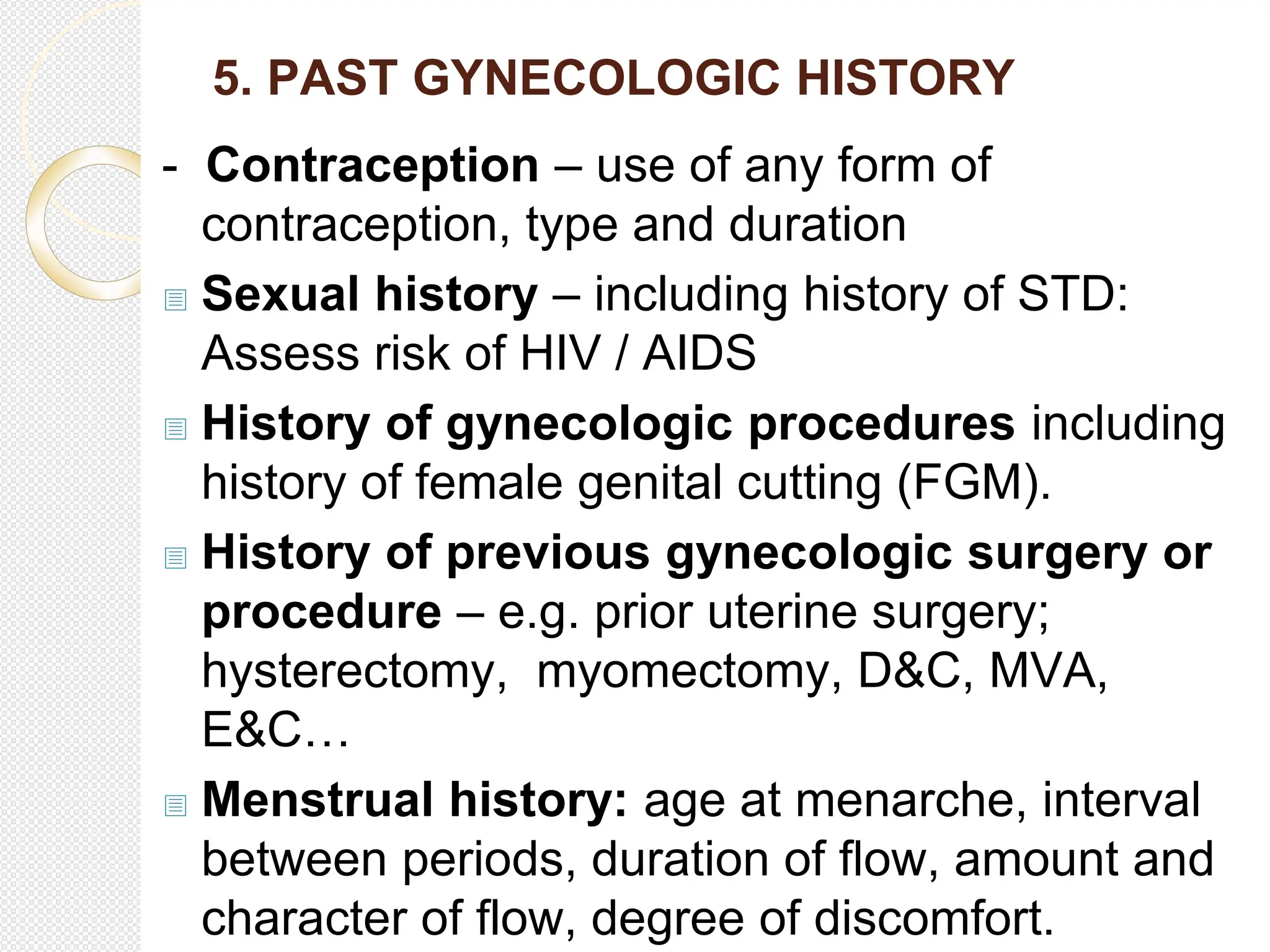
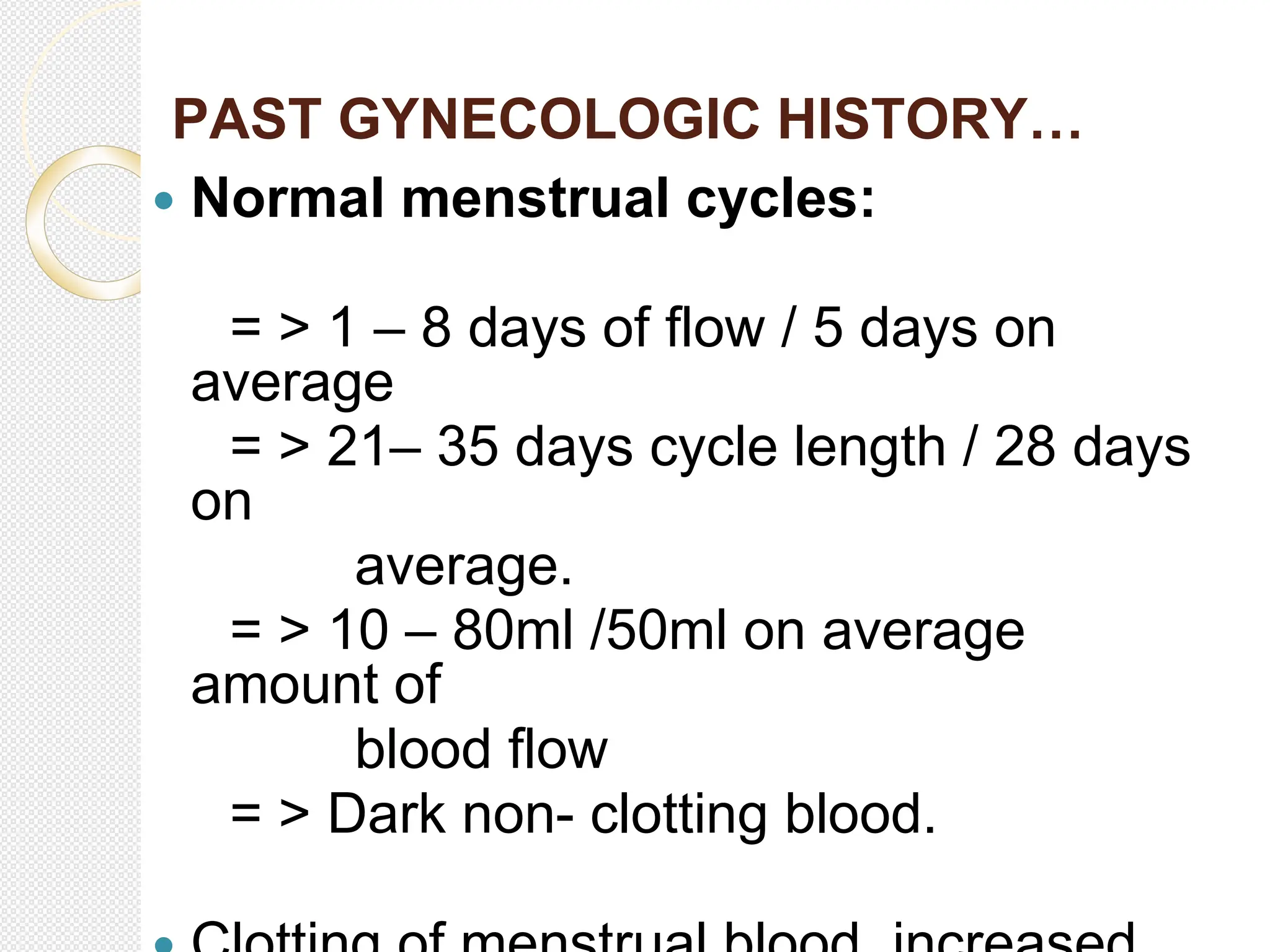
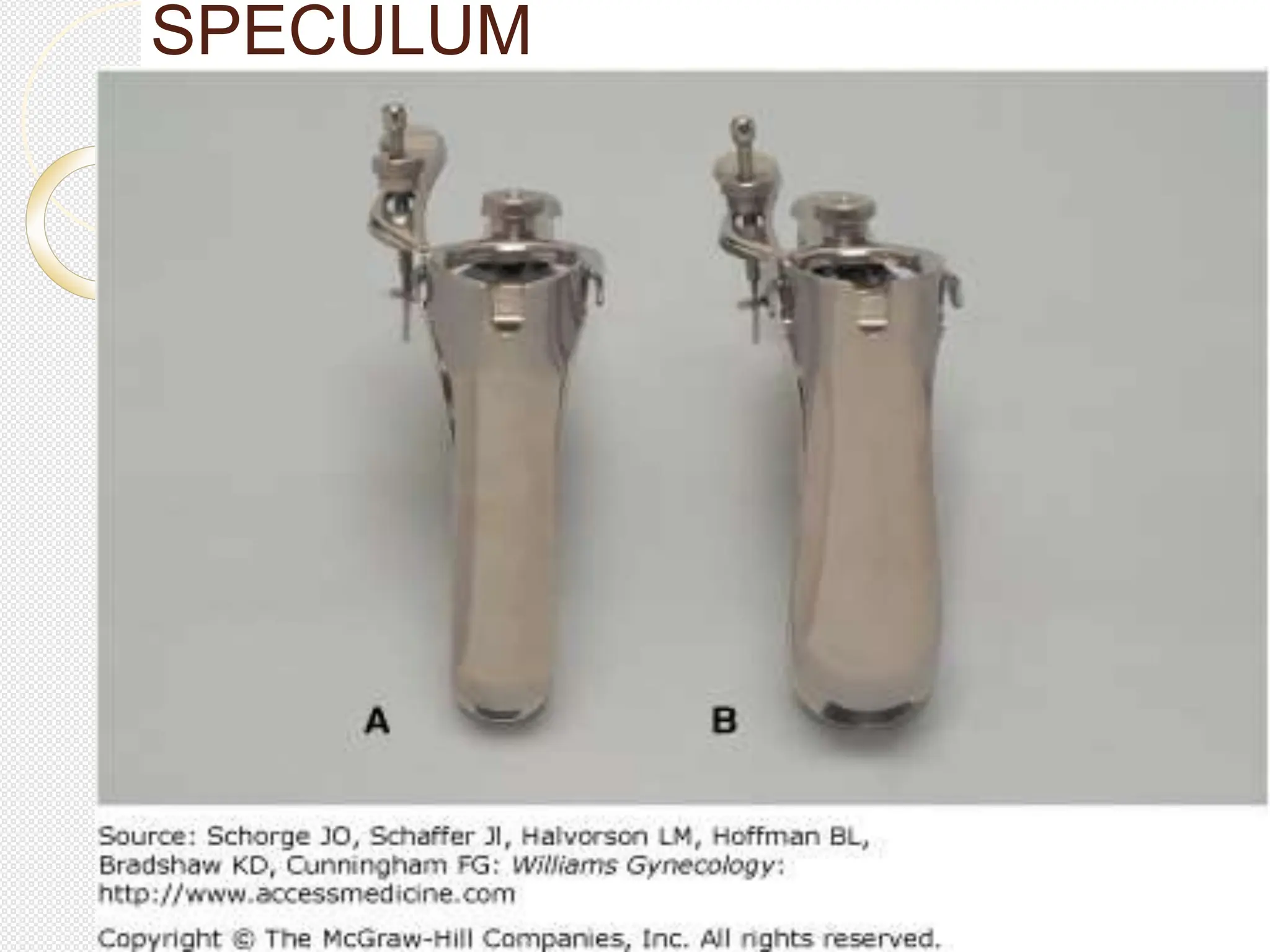
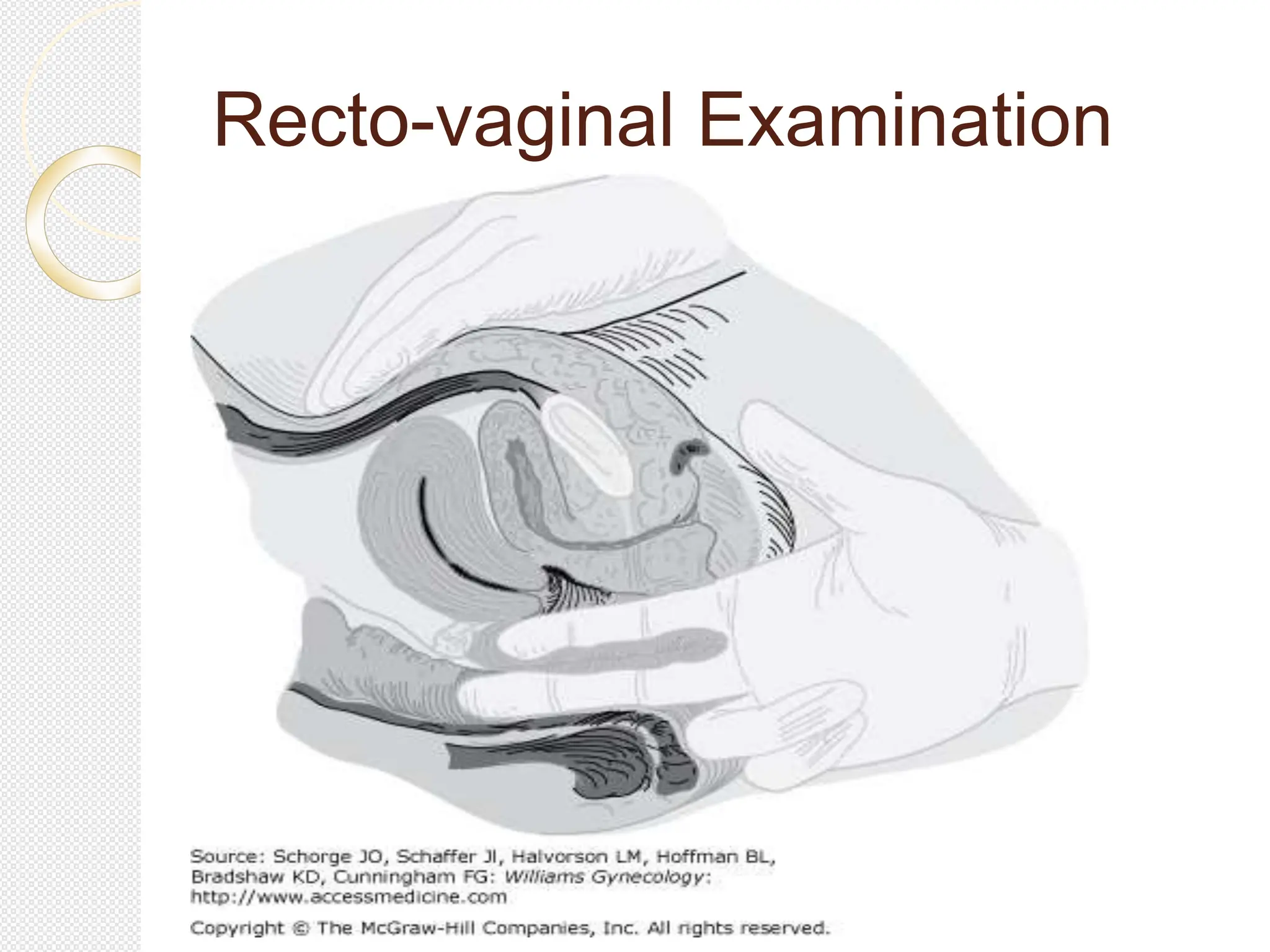
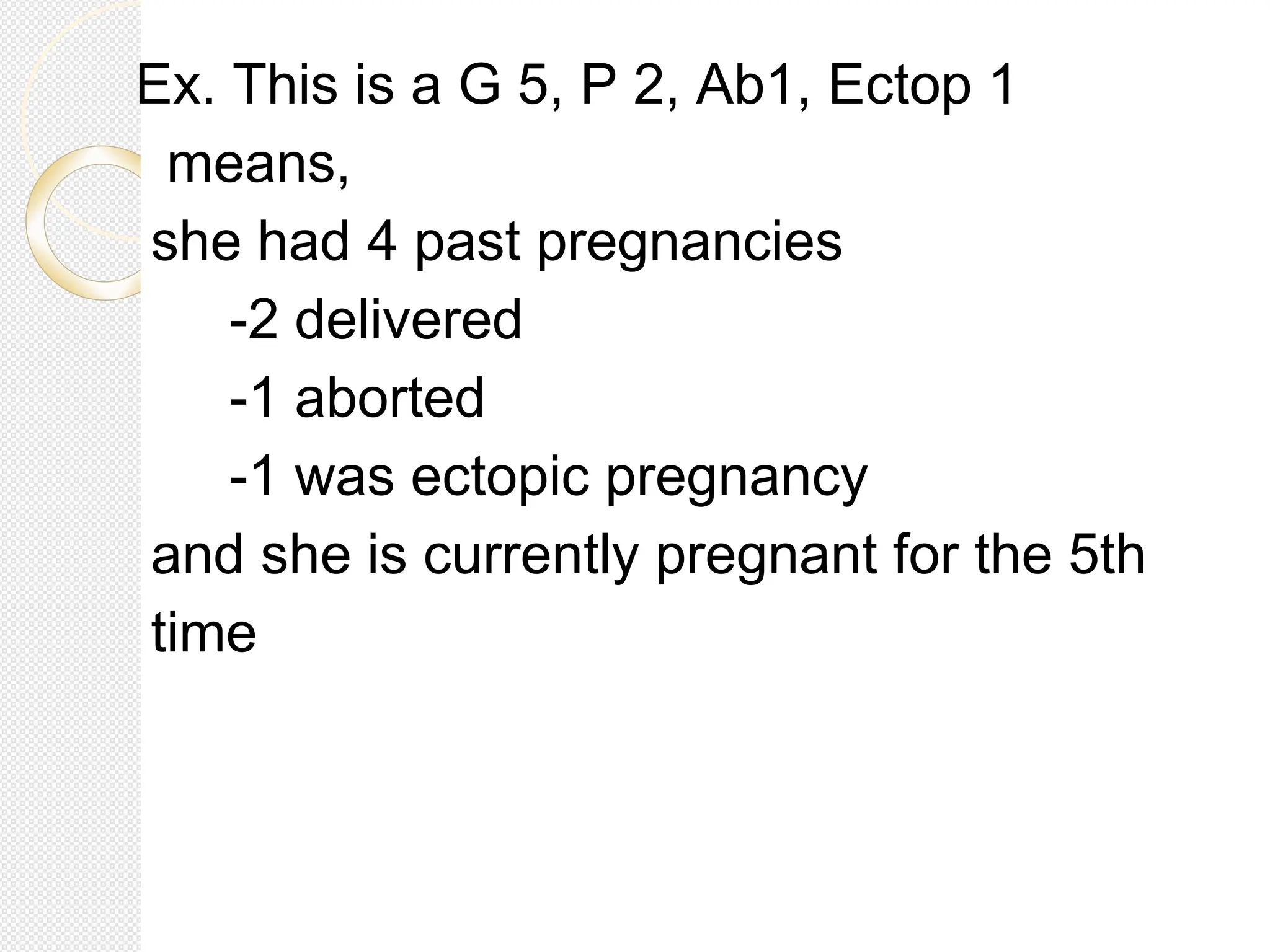
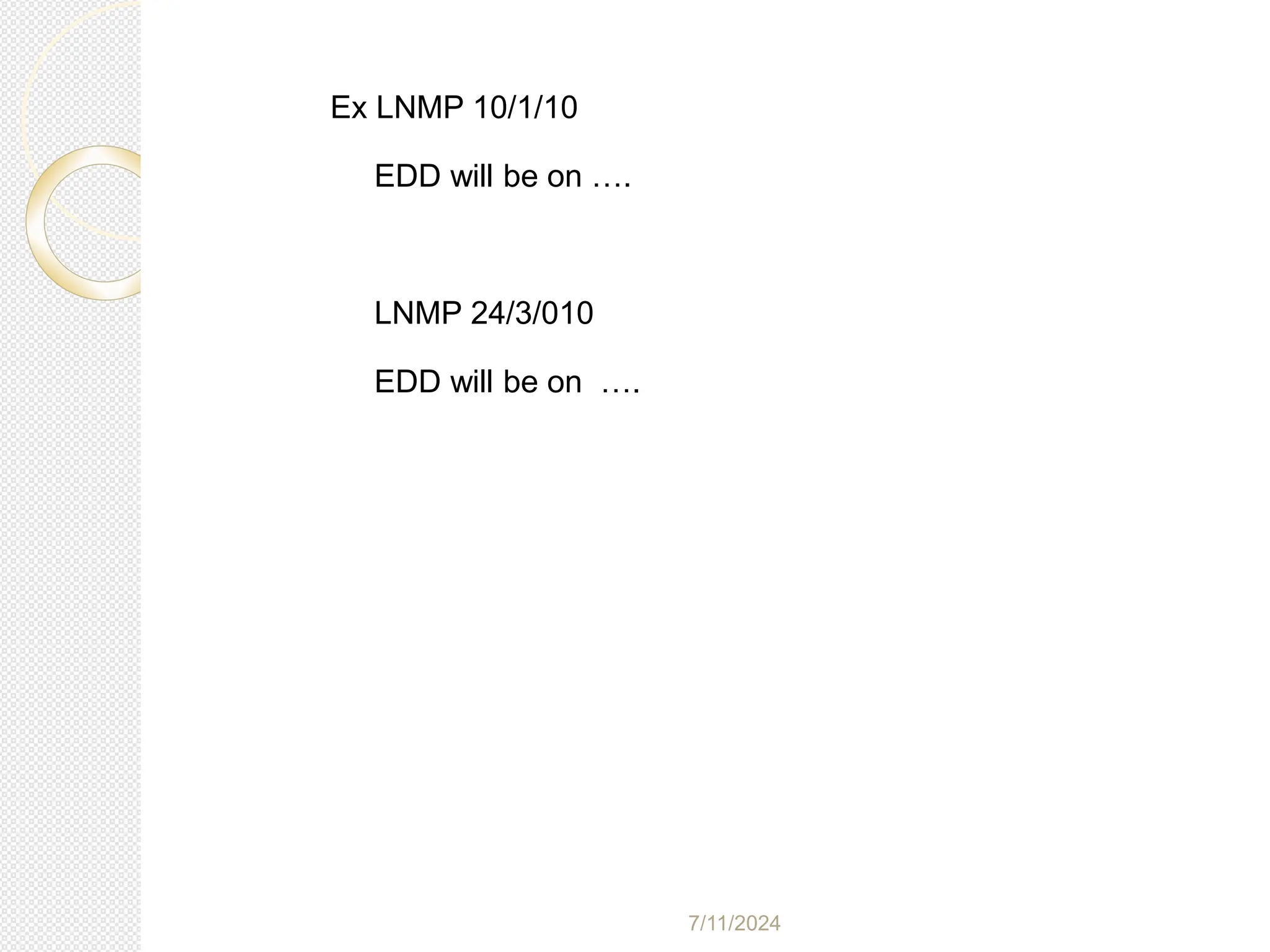
The document outlines the importance of history and physical examination in obstetrics and gynecology, emphasizing components such as obstetric history, general physical examination, and gynecologic history. It details how to gather patient information, assess risk factors, and conduct examinations systematically across various body systems. Additionally, it provides guidelines for identifying complications and making treatment plans based on the gathered information.