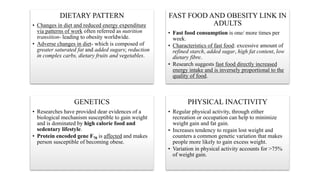
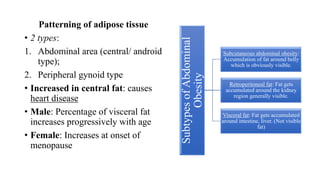
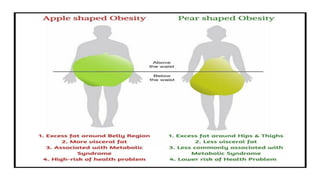
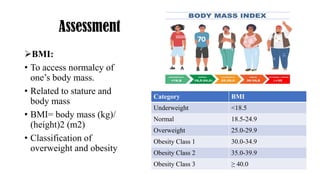
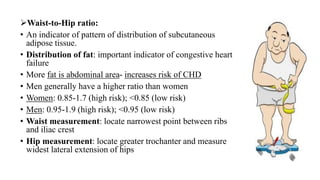
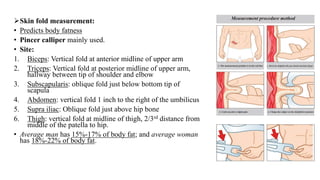
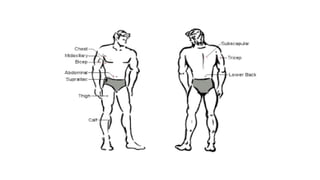
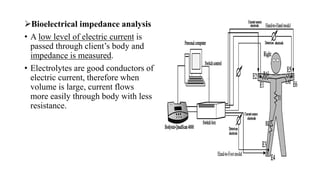
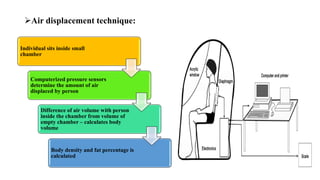
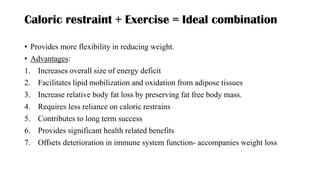
The document discusses obesity as a complex global epidemic affecting 1.9 billion overweight individuals, with 600 million classified as obese. It examines contributing factors such as dietary patterns, genetics, and physical inactivity, along with the serious comorbidities linked to obesity like cardiovascular disease and diabetes. The document also outlines assessment techniques, medical and surgical management options, and the importance of education, dietary changes, and exercise in obesity treatment.