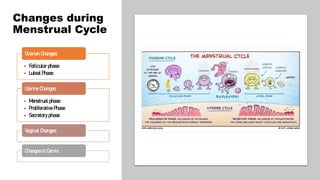
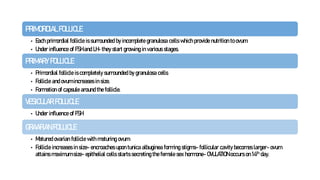
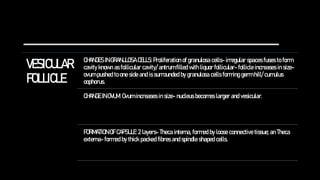
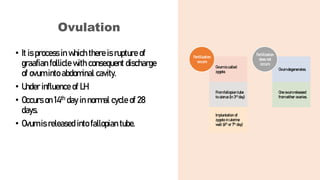
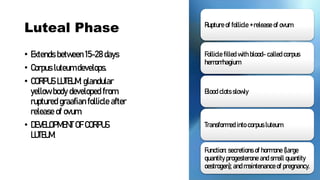
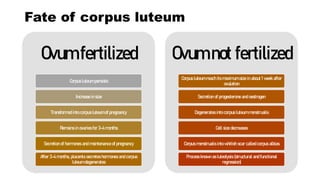
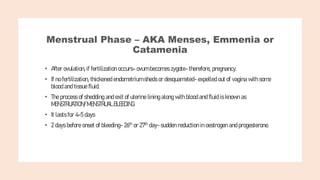
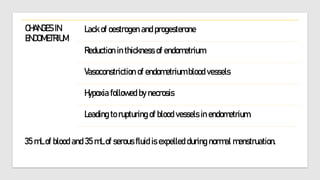
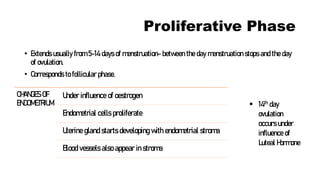
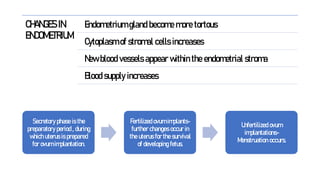
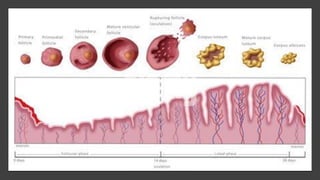
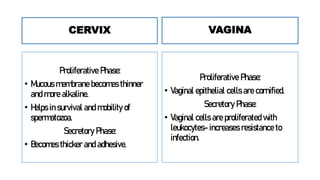
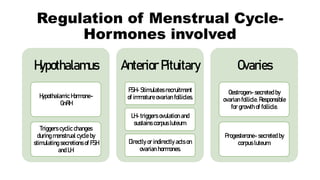
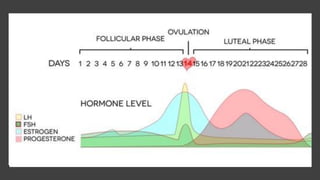
The document provides a detailed overview of the menstrual cycle, which includes phases such as the follicular phase, ovulation, and luteal phase, spanning from menarche at age 12-15 to menopause at 45-50. Key processes like ovum maturation, hormone secretion, and uterine changes during menstruation are discussed, along with the roles of various hormones like FSH, LH, estrogen, and progesterone. The cycle is regulated by hormonal signals from the hypothalamus and pituitary gland, affecting ovarian and uterine functions.