The document provides an overview of the history and fundamentals of nursing. It discusses:
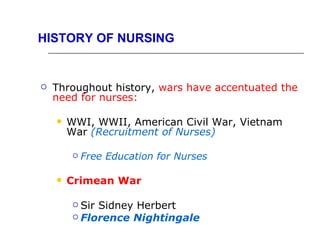
1) The early origins and evolution of nursing from ancient civilizations through major historical events like wars and the establishment of hospitals and codes of sanitation.
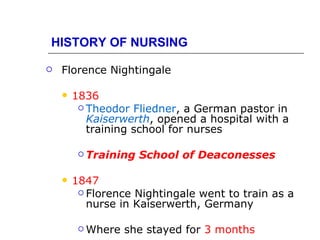
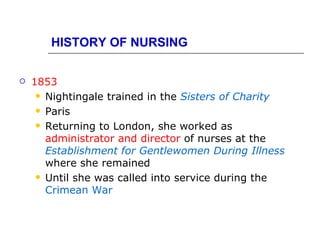
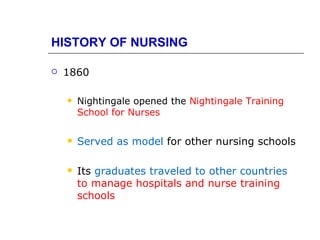
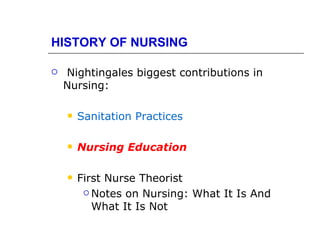
2) The contributions of Florence Nightingale including establishing nursing education standards and emphasizing sanitation practices.
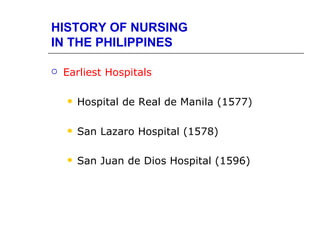
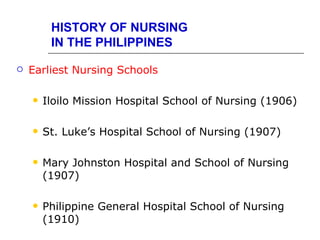
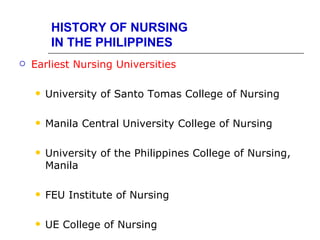
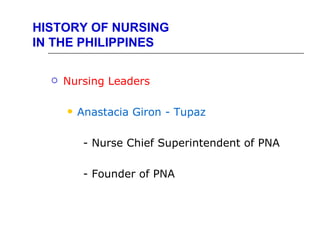
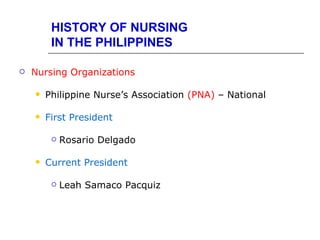
3) The development of nursing in the Philippines including the earliest hospitals and nursing schools.
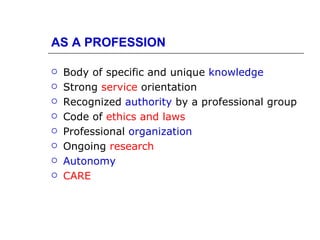
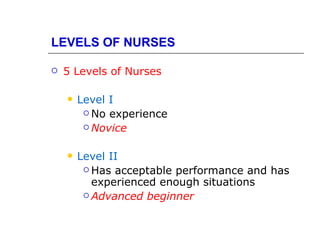
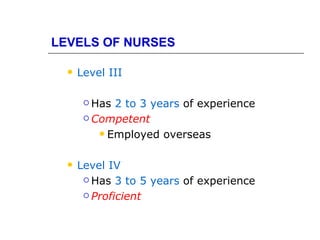
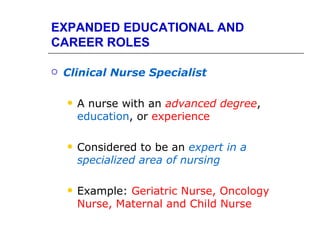
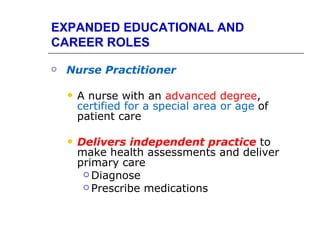
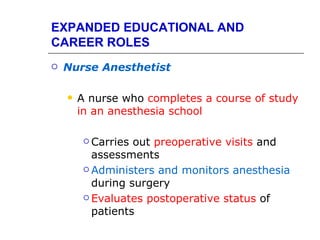
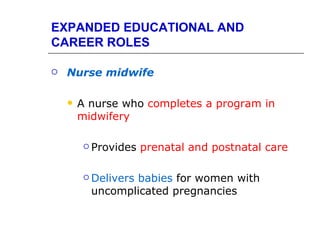
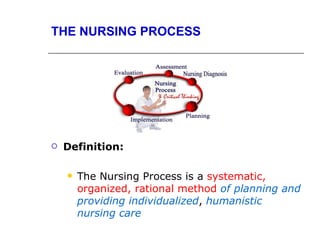
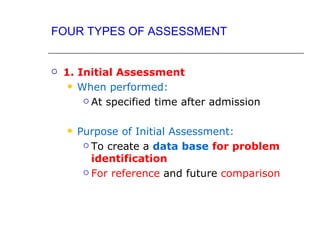
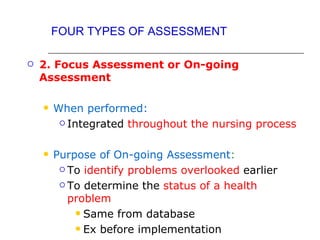
4) Key nursing concepts like the definition of a nurse, levels of nursing practice, fields of nursing practice, and expanded educational and career roles for nurses.