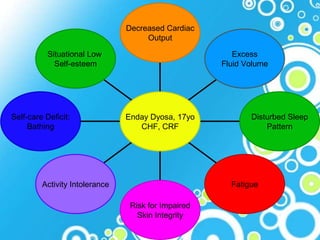
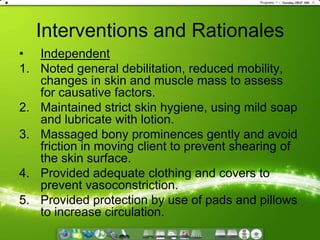
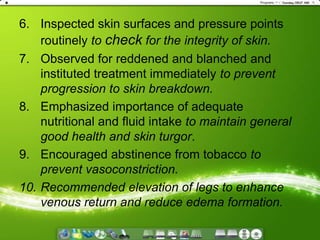
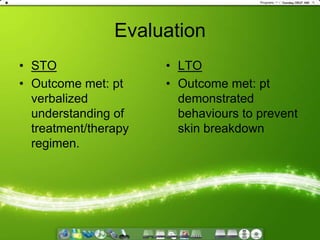
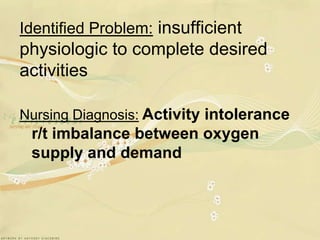
1. The document provides a nursing care plan for a patient with congestive heart failure and chronic renal failure, outlining various identified problems, objectives, interventions, and evaluations.
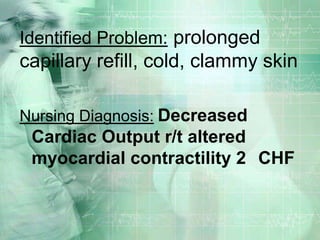
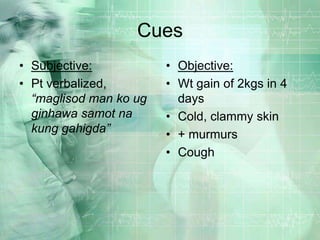
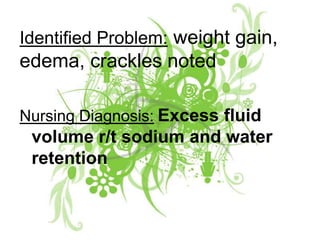
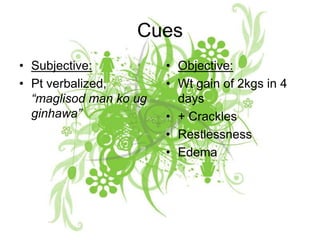
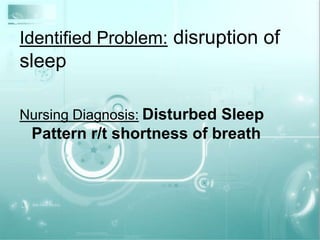
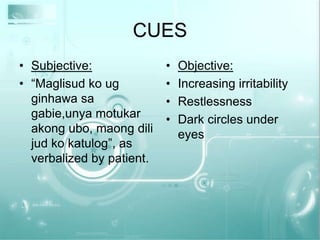
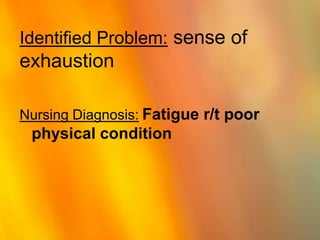
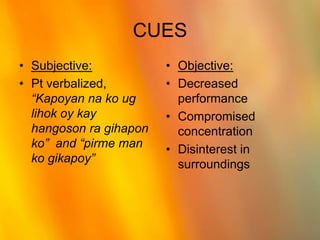
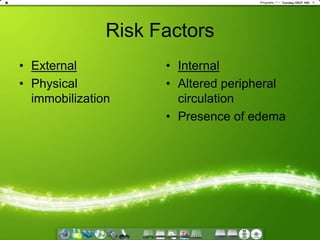
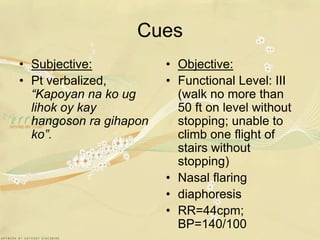
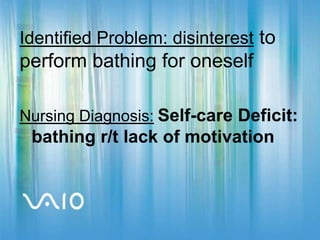
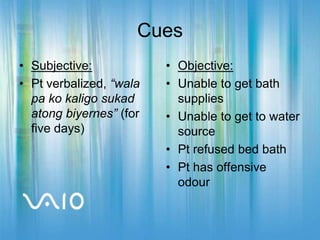
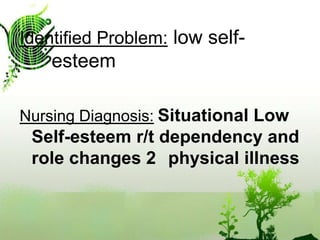
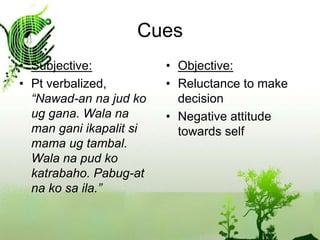
2. It addresses problems related to decreased cardiac output, excess fluid volume, disturbed sleep patterns, fatigue, risk for skin breakdown, activity intolerance, bathing self-care deficits, and situational low self-esteem.
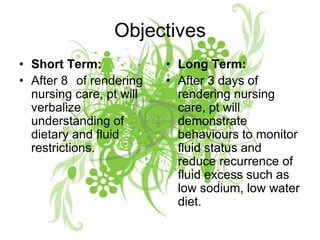
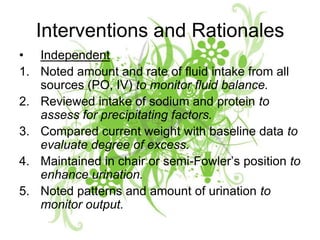
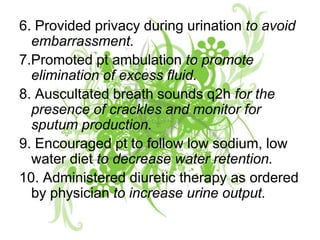
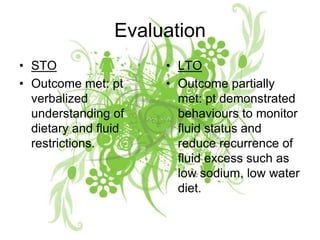
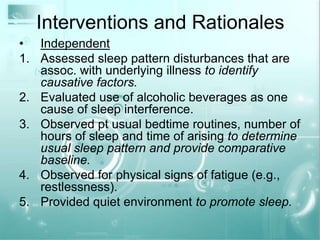
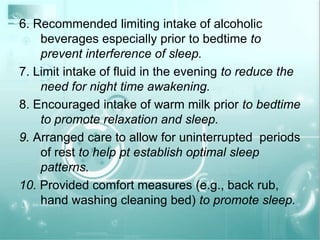
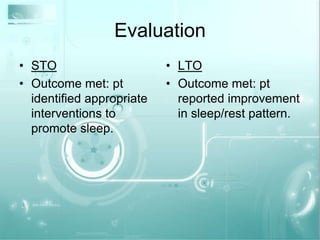
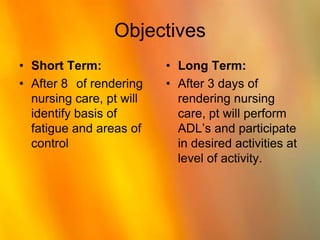
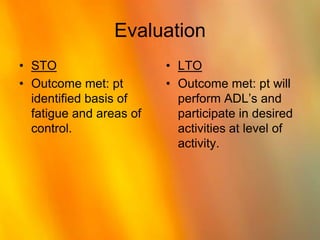
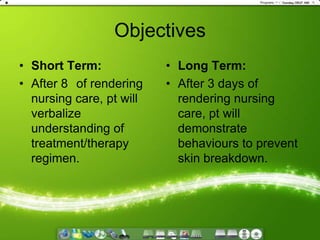
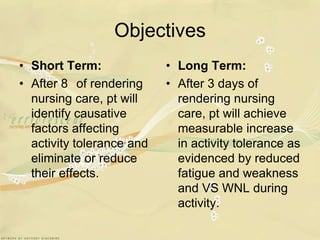
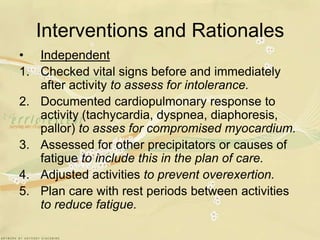
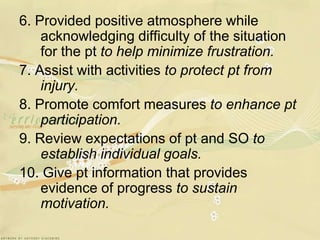
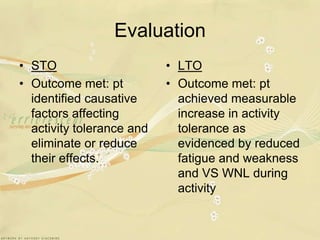
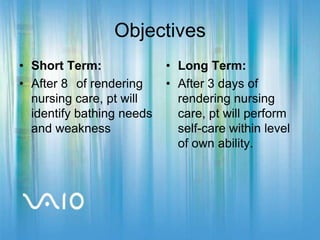
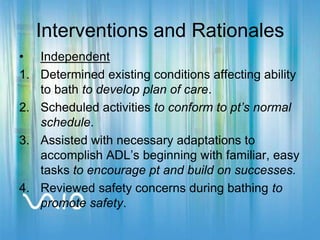
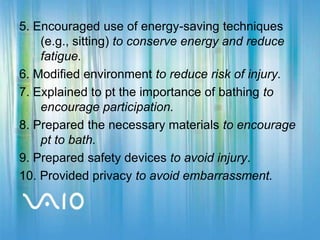
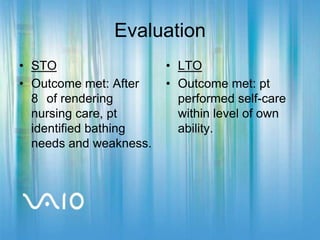
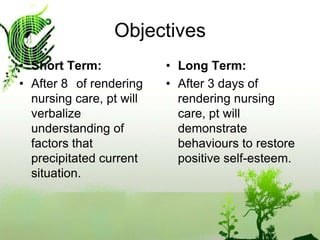
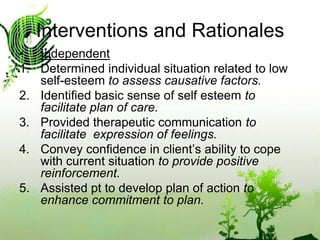
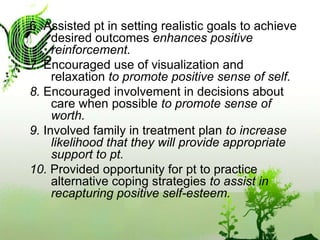
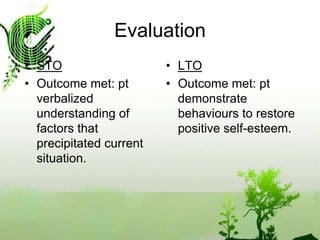
3. For each problem, the care plan proposes short-term and long-term objectives, lists nursing interventions and rationales, and evaluates the outcomes.