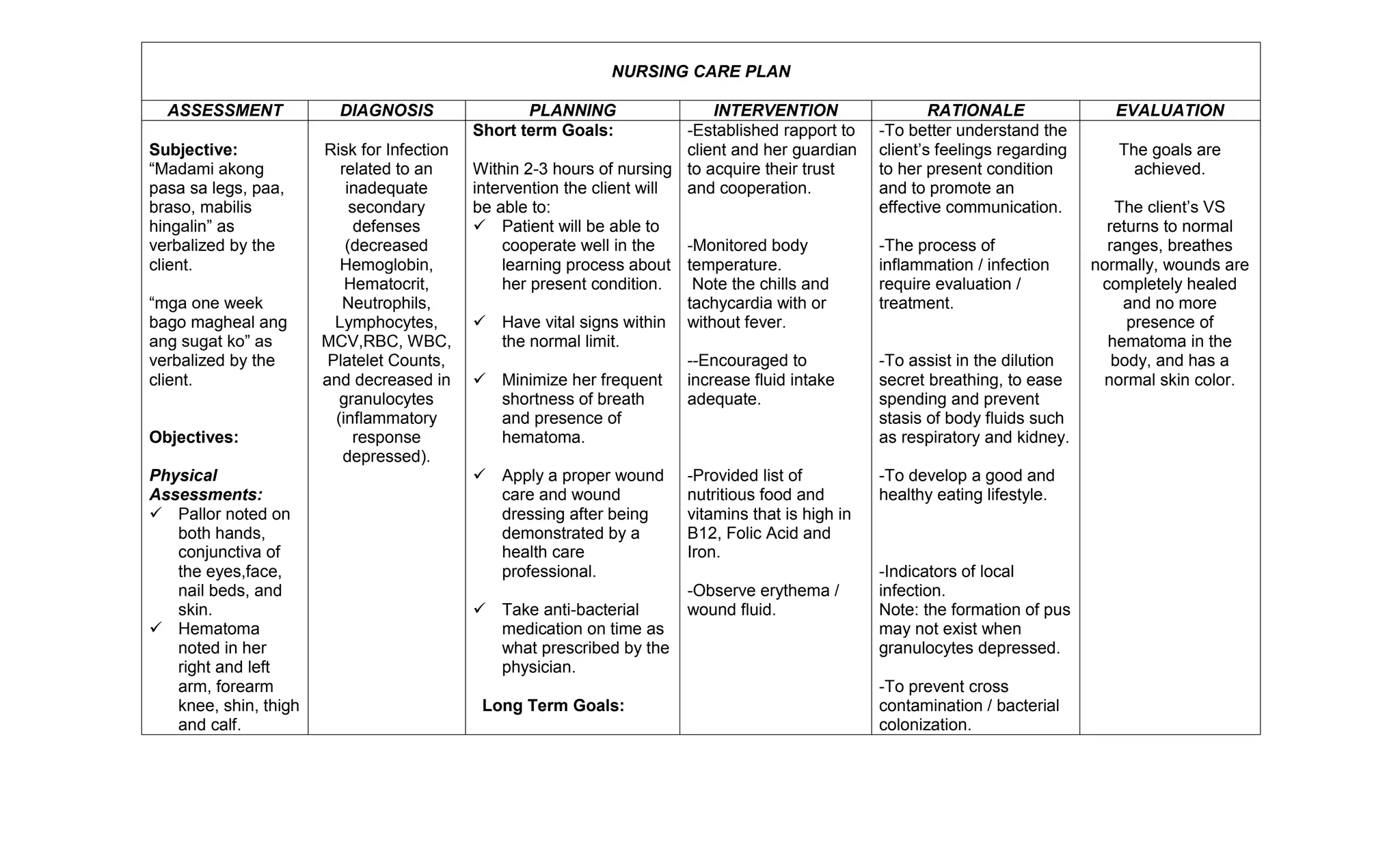
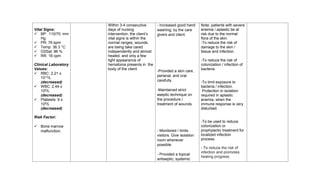
The nursing care plan assessed a client with easy bruising and weakness, diagnosed a risk for infection due to low blood counts, and planned short-term goals of stabilizing vital signs and long-term goals of healing wounds and increasing nutrition through dietary changes and medication.