The document proposes the National Urban Health Mission to address health issues of India's growing urban poor population. Key points:
1) India's urban population is growing rapidly and will reach 43.2 crores by 2021, increasing strain on infrastructure. The urban poor have poor access to healthcare due to inadequate public systems and high costs of private care.
2) The NUHM will cover all cities over 1 lakh people and state capitals. It will focus on the urban poor, especially those in slums, as well as other vulnerable groups. The mission aims to facilitate equitable access to available healthcare.
3) Components include strengthening public primary care, engaging private providers, promoting community involvement, organizing women into health









































































![117
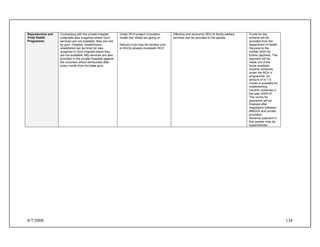
Draft Generic MoU Appendix 2
Draft Memorandum of Understanding (MoU) Between Ministry of Health & Family Welfare,
Government of India And The Government of the State of …………../ Urban Local Body
[NOTE: Explanatory Footnotes and Sample Annexes are for purposes of
clarification and illustration only.]
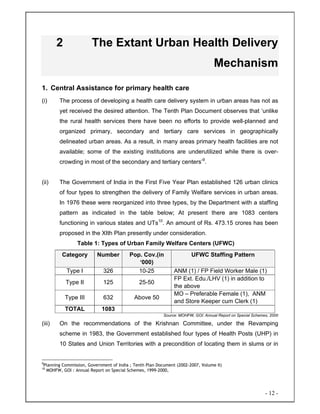
1. Preamble
1.1 WHEREAS the National Urban Health Mission, hereinafter referred to as
NUHM, has been launched for nation-wide implementation with effect from
……..
1.2 WHEREAS the NUHM aims at providing accessible, affordable, effective,
accountable and reliable health care to all citizens and especially urban poor
with focus on urban slums (listed and unlisted) and other vulnerable sections
like destitute, beggars, street children, construction workers, coolies,
rickshaw pullers, sex workers and other such migrant workers category who
do not reside in slums but reside in temporary settlements, or elsewhere in
any part of the city or are homeless.
1.3 AND WHEREAS the NUHM would achieve its objectives through
rationalisation and strengthening of the existing primary health care services,
provisioning of a platform for integration of vertical programs and structures;
delegation and decentralization of authority; involvement of Urban Local
Bodies, strengthening the management system with adequate scope for
community involvement in planning and management and other supportive
policy reform measures in the areas of medical education, public health
management, incorporation of Indian Systems of Medicine, regulation of
health care providers and new health financing mechanisms;
1.4 NOW THEREFORE the signatories to this Memorandum of Understanding
(hereinafter referred to as MoU) have agreed as set out herein below.
2. Duration of the MoU
2.1 This MoU will be operative with effect from the date of its signing by the
parties concerned and will remain in force till March, 2012 or till its renewal
through mutual agreement whichever is earlier.](https://image.slidesharecdn.com/nuhm-draft-140419143022-phpapp02/85/Nuhm-draft-117-320.jpg)


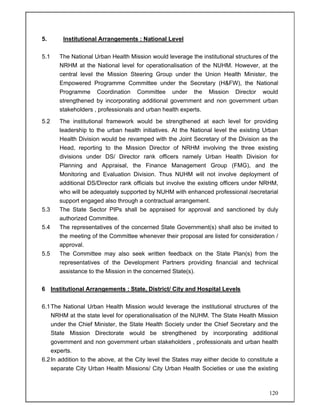

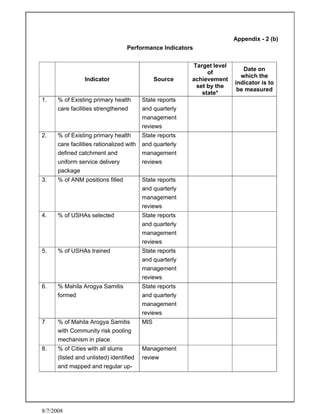

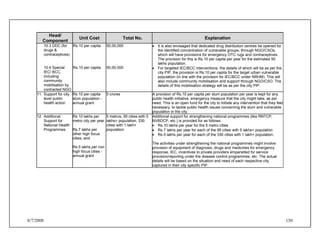
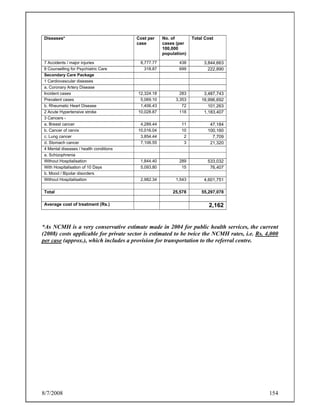
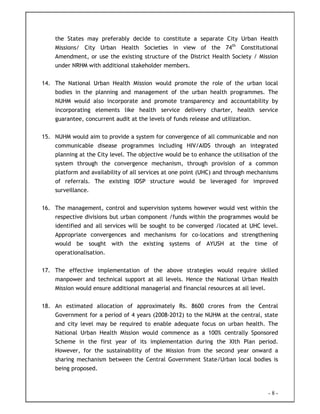
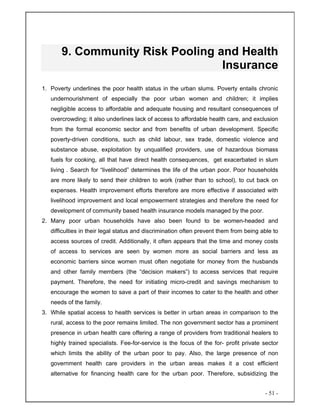
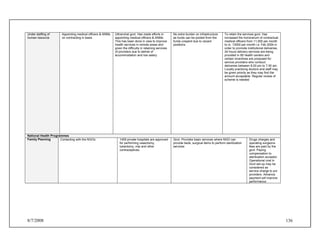
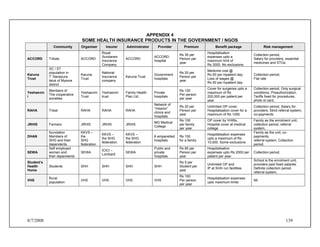
![8/7/2008 131
APPENDIX 2(c)
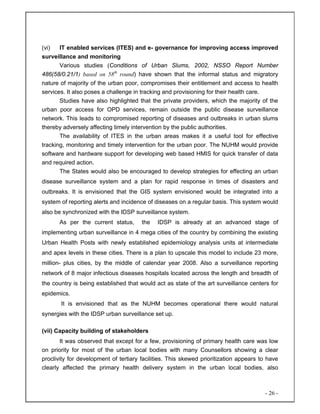
Agreed Performance Indicators
A: Mandatory Performance Indicators
A-1: Share of State Budget for health sector [ Benchmark: minimum 10% (nominal)
increase every year]
Item /category
Last Financial
Year
Current
Financial Year
%age Increase
over previous
year
State Budget-Total
Outlay for health sector
B Indicators to assess progress of Institutional Reforms
Domain
Milestones to be
achieved
Agreed month for
achievement
Agreed source for
verifying
achievement
Empowerment
and involvement
of ULBs
Strengthening
and capacity
building of
district/ City
societies
Streamlining /
strengthening of
MIS(including
disease
surveillance)
Streamlining,
strengthening
and re-](https://image.slidesharecdn.com/nuhm-draft-140419143022-phpapp02/85/Nuhm-draft-131-320.jpg)

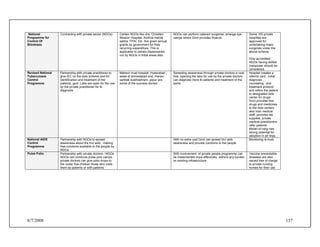



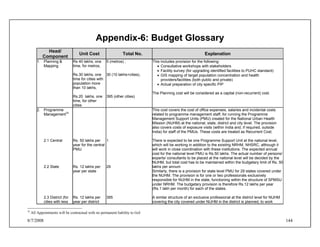
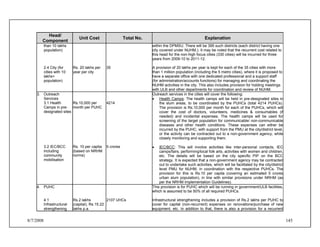
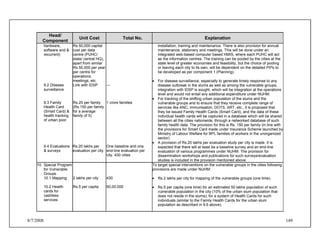
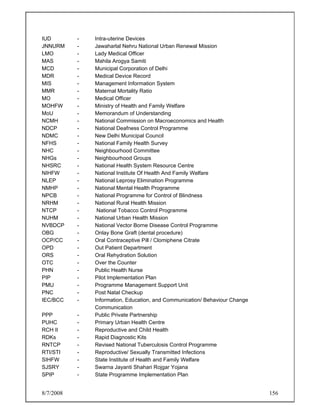
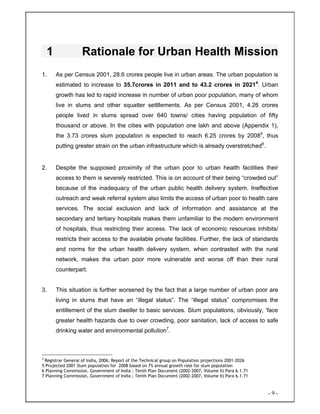
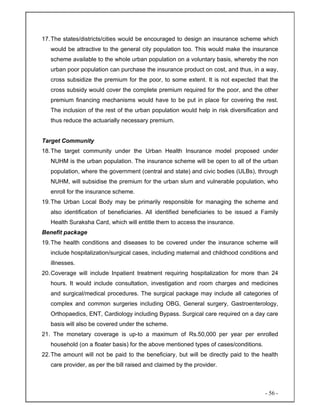
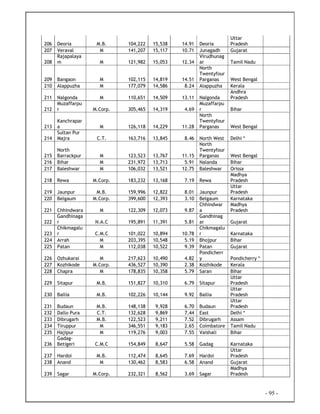
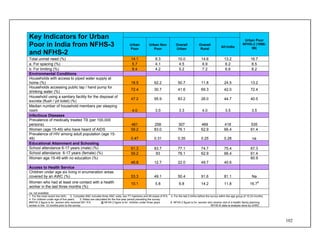
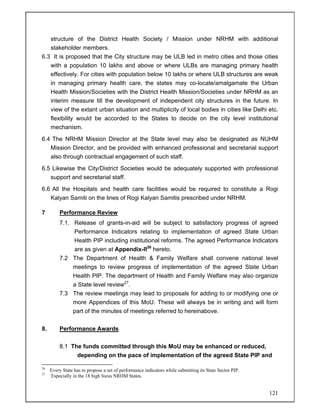
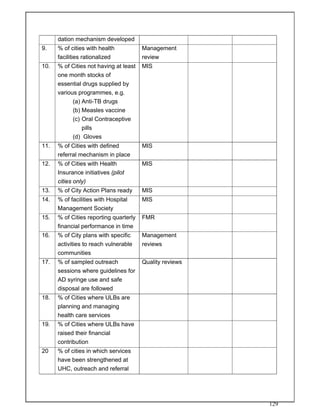
![8/7/2008 146
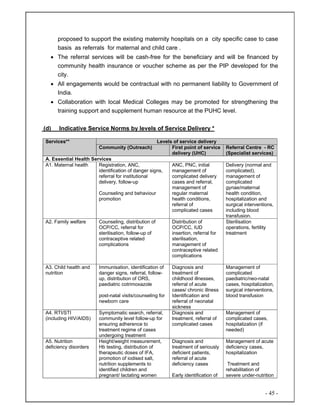
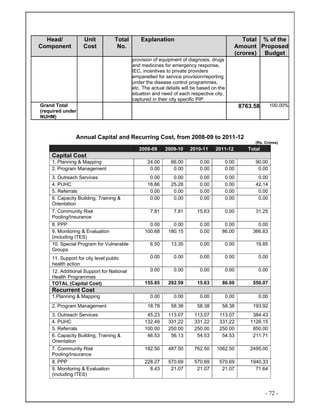
Head/
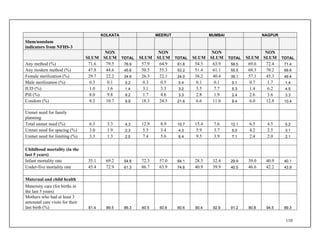
Component
Unit Cost Total No. Explanation
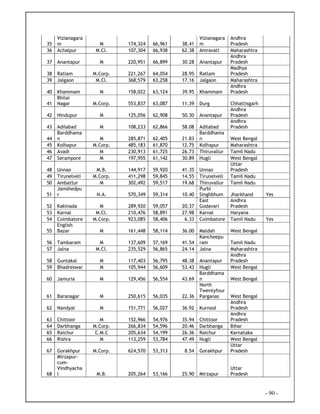
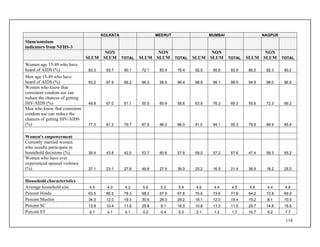
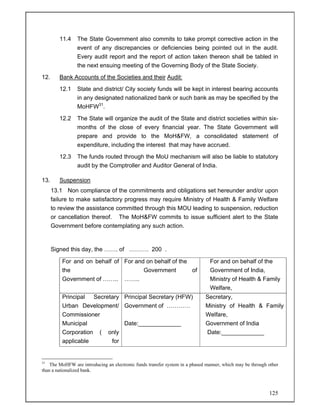
4.2 RKS funds
(recurring including
salaries, OE, etc.)
[estimates, based
on NCMH costs
and prevailing
govt. rates for
contractual
positions]
Rs.50,000 p.a. (as
per NRHM norms
for PHCs)
2107 UHCs
cost of Rs.15.22 lakhs per year per PUHC is provided for to cover costs of
salary, incidental expenses, operations & maintenance, etc. The staffing
suggested for the PUHC includes a doctor, 2 multi-skilled paramedics
(including pharmacist, lab technician etc.), 2 multi-skilled nurses, 4 ANMs,
apart from clerical and support staff (peons, sweepers). This is in addition to
the existing salaries borne by state/municipal bodies for the existing staff.
Apart from that, this also includes provision for additional staff provided under
NUHM like one Public Health Manager at the PUHC, managing and
coordinating the NUHM activities in the area, including activities in
coordination with the Referral Units and revolving fund for 12 USHA/Link
Workers. The provision of Rs. 10 lakhs per year includes provision salaries
for these staffs.
Apart from the above, there is a provision of Rs.50,000 per PUHC per year as
untied fund for annual maintenance and miscellaneous expenses, similar to
the funds for PHCs under NRHM.
5. Referrals
5.1 Support for
RKS in
government
referral units
Rs.4000 per
patient
(Rs.3393as per
NCMH, rounded off
to include referral
transportation)
5 lakhs (1% of target
population)
There is provision for the government health facilities designated as referral
centres in the cities is in the form of Rs.4000 per case, which also includes
provision for referral transportation. Rs. 4000 per case is the average cost of
delivering secondary level healthcare, as per NCMH estimates (Rs.3393)
rounded off to accommodate provision for referral transportation also. For
calculations, it is estimated that 2% of the target population of 5 crores will
need referral transportation, of which 50% will go to public referral units.
6. Capacity
Building,
Training &
Orientation
6.1 Community
level
6.2 Link workers
6.3 ANMs
6.4 Multi-skilled
Nurses
Rs 1000
Rs 10,000
Rs. 5000
Rs. 5000
Rs. 5000
1, 02,000 MAS
25,00033
16,856
500034
5000
For capacity building the target is as follows:
• Mahila Arogya Samittee – orientation training of all 1,02,000 MAS (one
time) @ Rs. 1000 per MAS
• Orientation-cum-induction training of all Link workers (estimated 25,000)
@ Rs. 10,000 per worker
• One-time skill upgradation training of PUHC and other enlisted
government hospital staff including ANM (estimated 16,856), all Nurses,
Pharmacists, lab Technician (estimated number, 5000 each); with a
33
One link worker for every 2000 slum population
34
One per UHC, the rest from other enlisted/accredited health facilities](https://image.slidesharecdn.com/nuhm-draft-140419143022-phpapp02/85/Nuhm-draft-146-320.jpg)