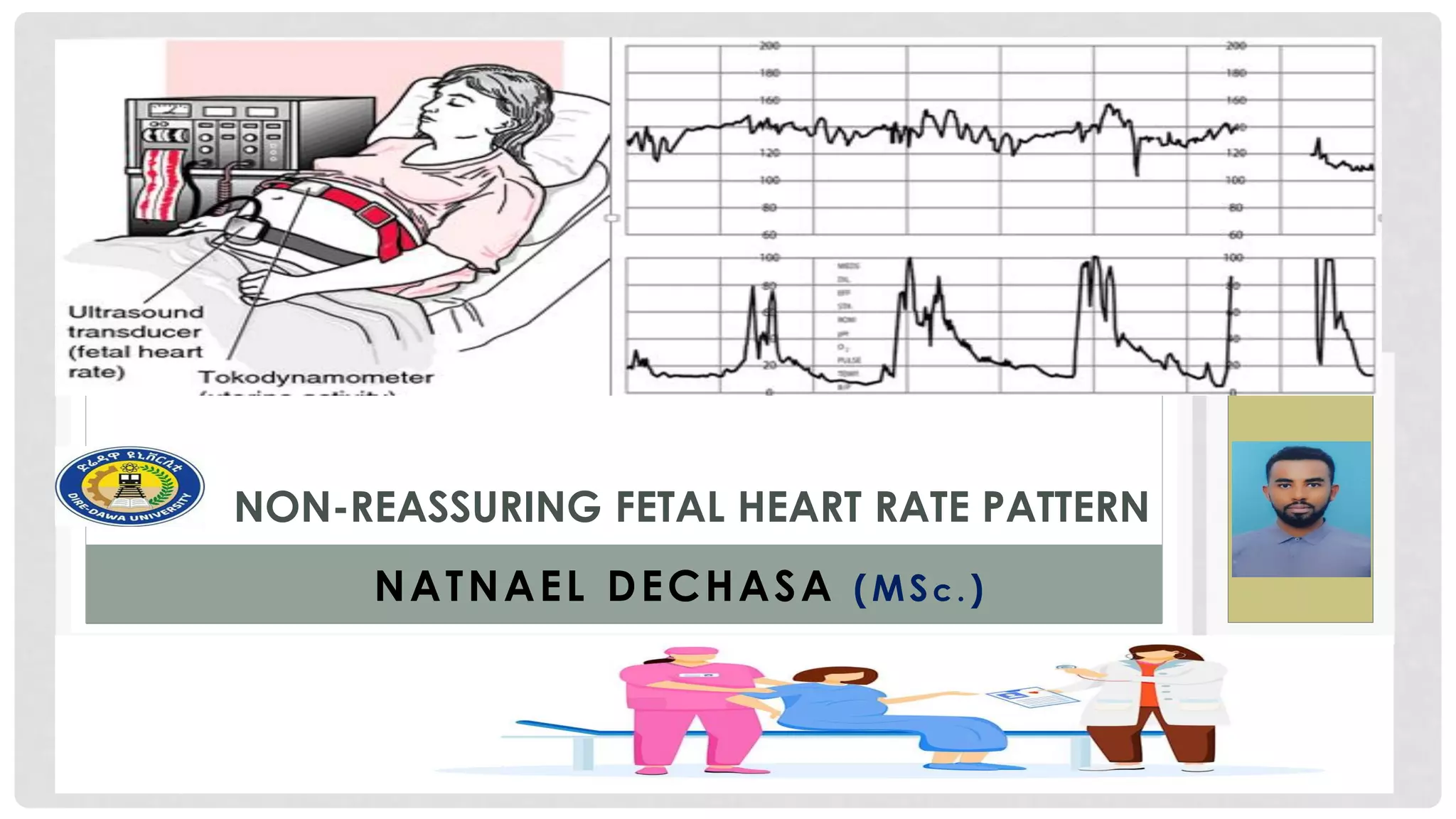
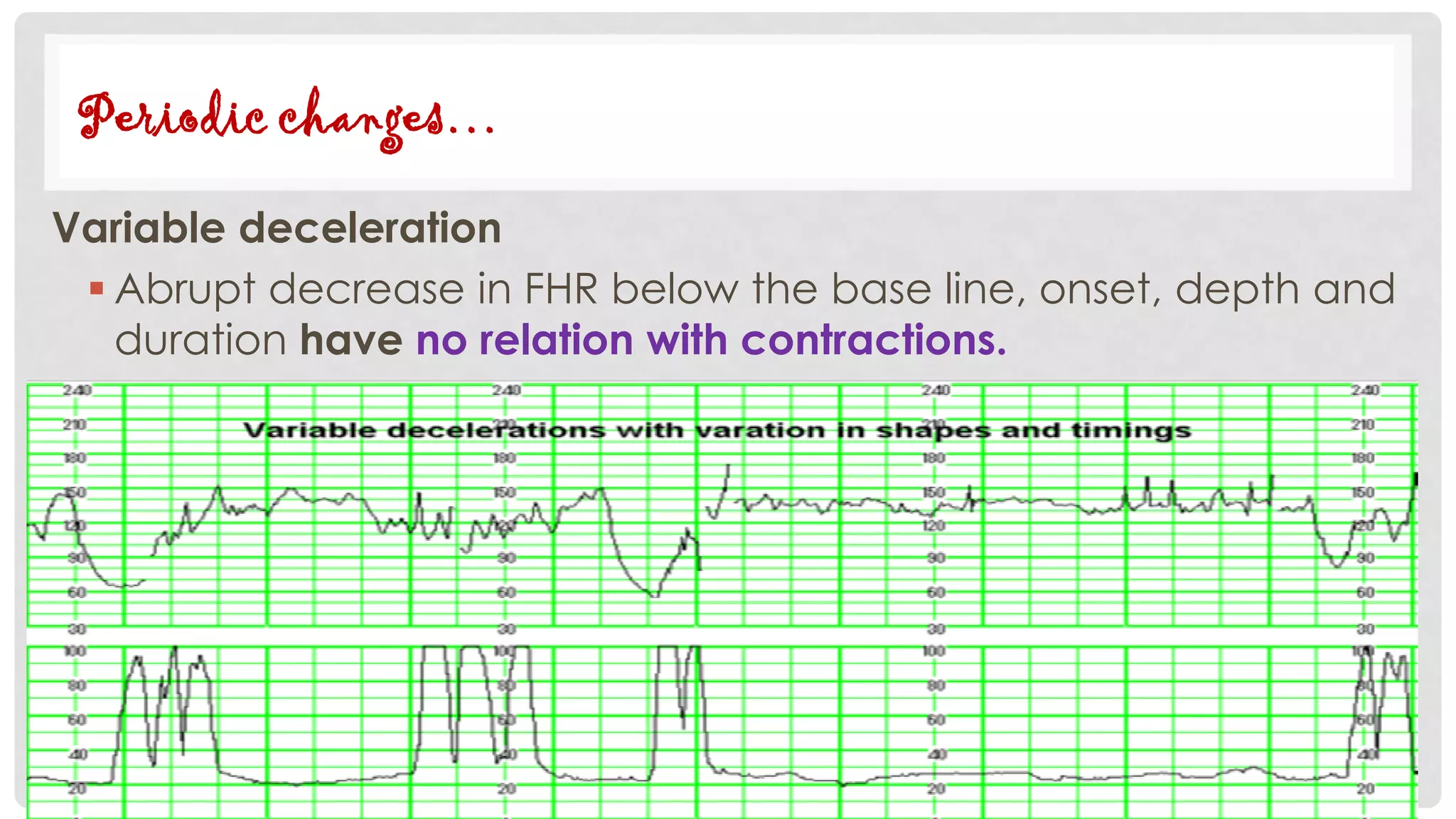
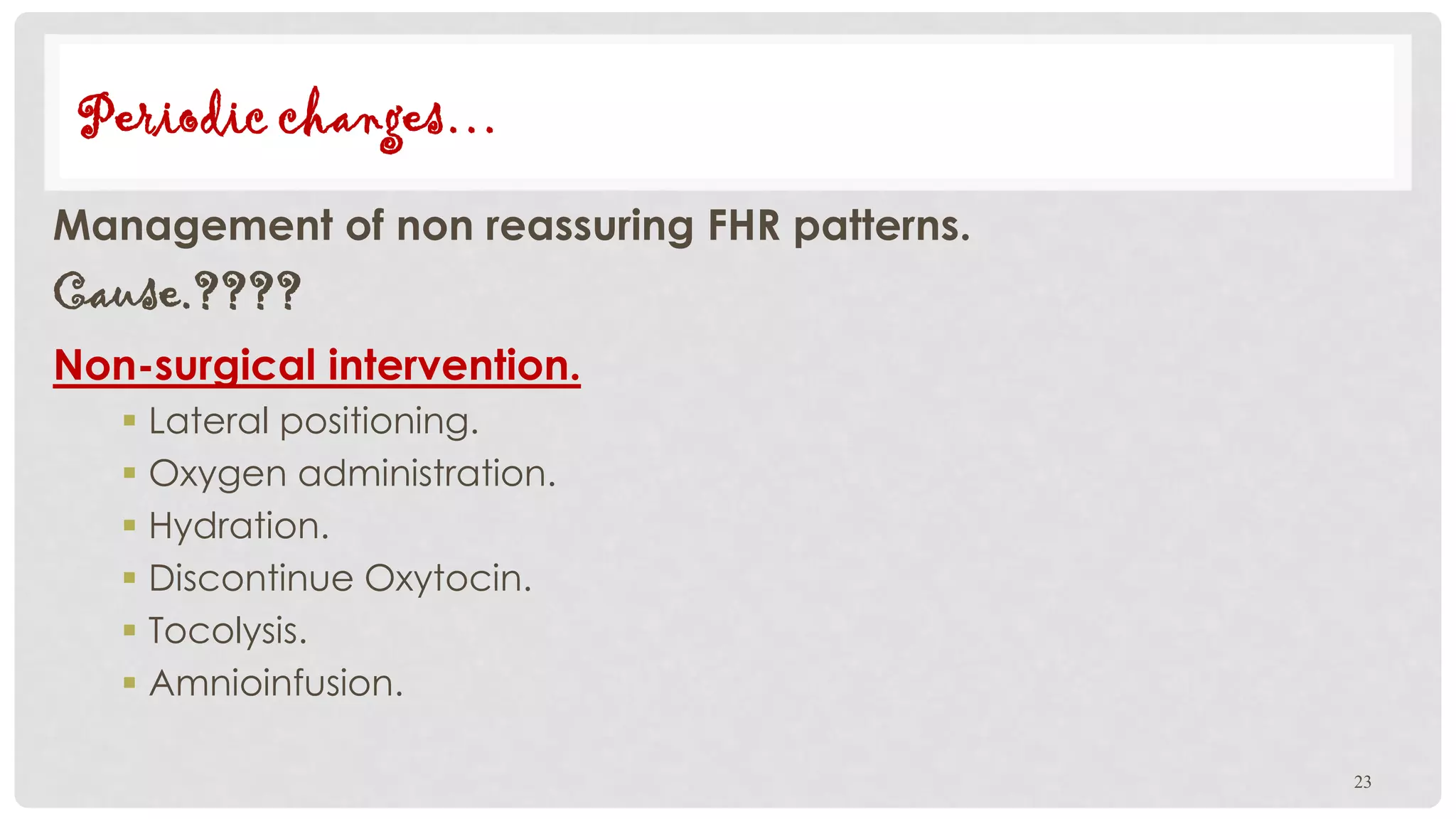
This document discusses fetal heart rate monitoring techniques and patterns. It describes intermittent auscultation using a fetoscope or Doppler ultrasound, and continuous electronic fetal monitoring using cardiotocography. Normal fetal heart rate is between 120-160 bpm; patterns like late decelerations, variable decelerations, or a sinusoidal pattern are non-reassuring. The document outlines how to interpret and manage different fetal heart rate patterns.