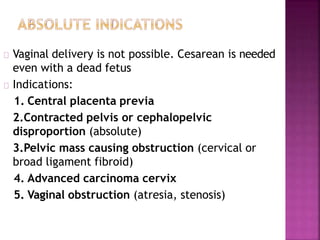
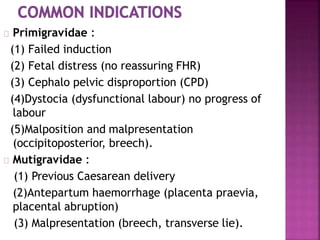
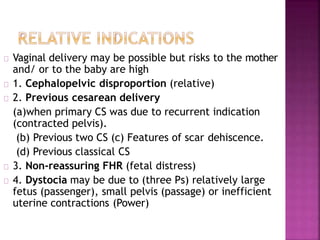
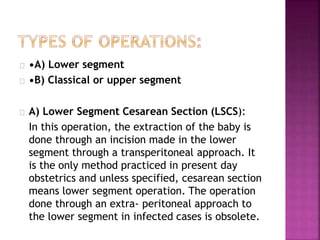
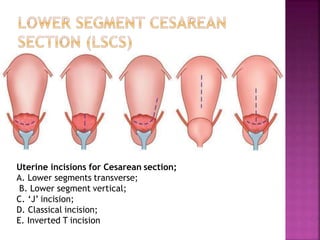
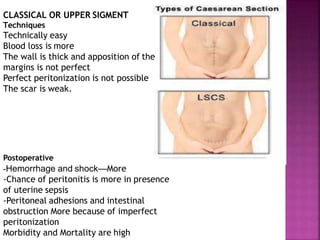
Cesarean section is a surgical procedure to deliver babies through incisions in the abdominal wall and uterus. It is indicated when vaginal delivery poses risks to the mother or baby. The incidence of cesarean sections has risen in recent decades. There are two main types - lower segment and classical. Lower segment cesarean section through a transverse lower uterine incision is now the standard procedure. Complications can include hemorrhage, infection, and injury to other organs. Proper preoperative preparation and postoperative care and monitoring can help prevent complications.