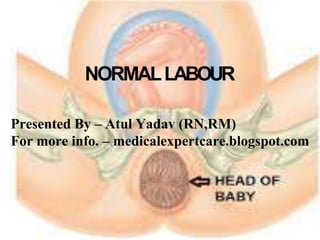
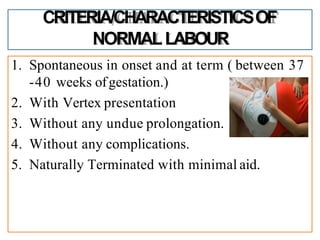
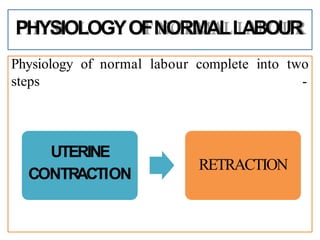
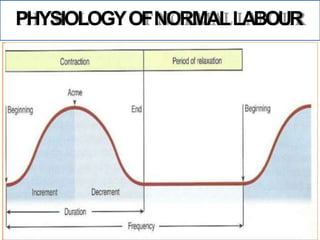
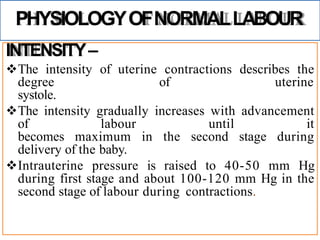
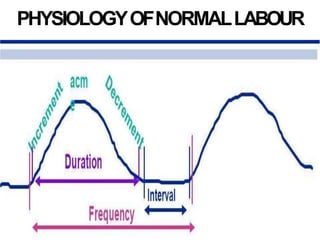
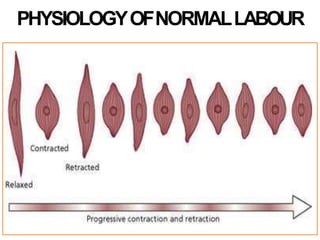
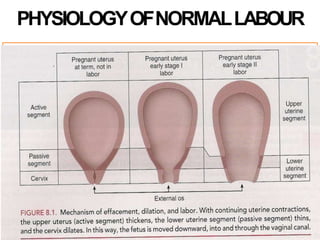
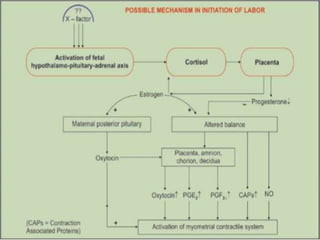
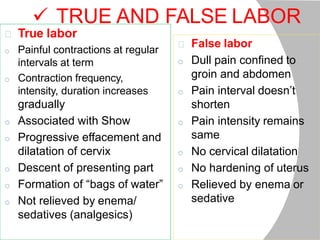
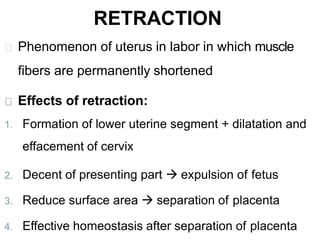
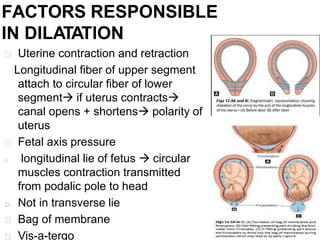
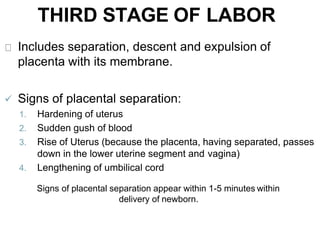
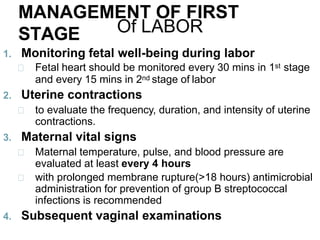
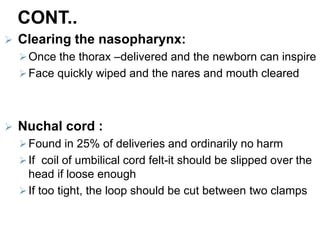
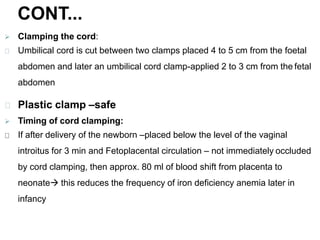
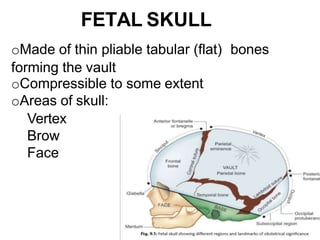
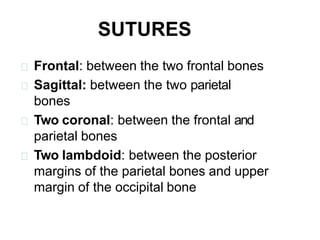
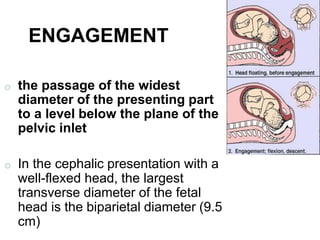
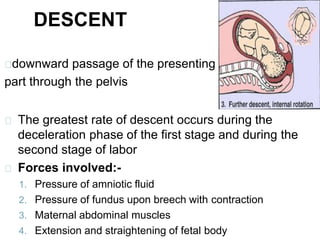
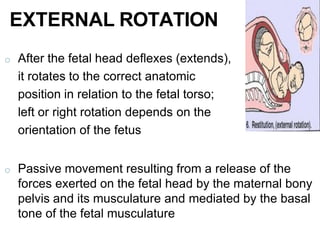
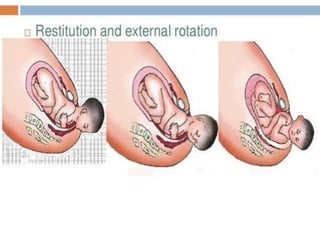
The document provides a comprehensive overview of normal labor, defining it as a physiological process involving spontaneous uterine contractions that lead to the expulsion of viable products of conception. It outlines the phases of labor, characteristics of normal labor, and the physiological mechanisms involved, including uterine contractions and retraction, as well as the roles of hormones in facilitating labor. Additionally, it addresses management during different stages of labor, including monitoring and interventions to ensure maternal and fetal well-being.