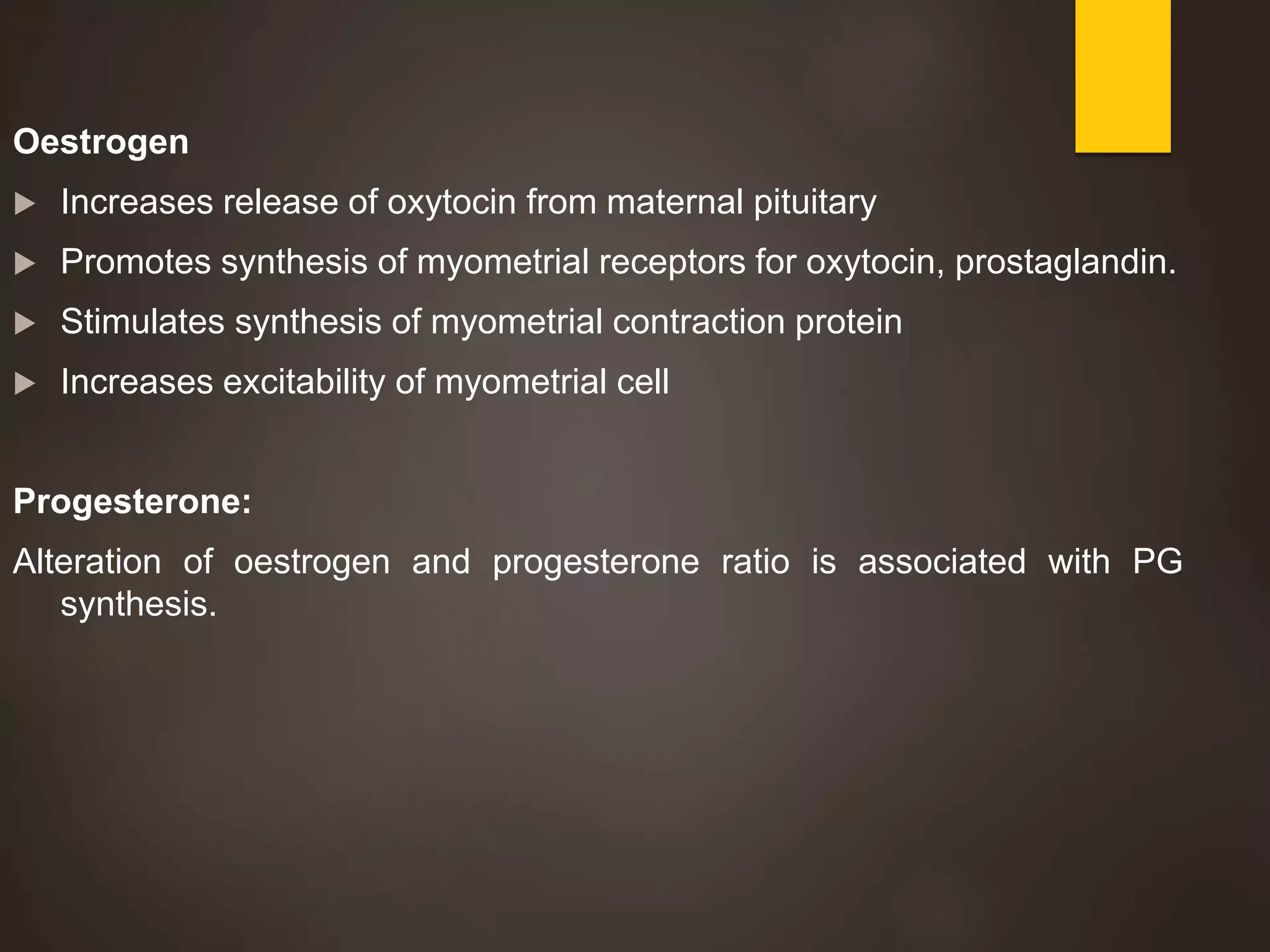
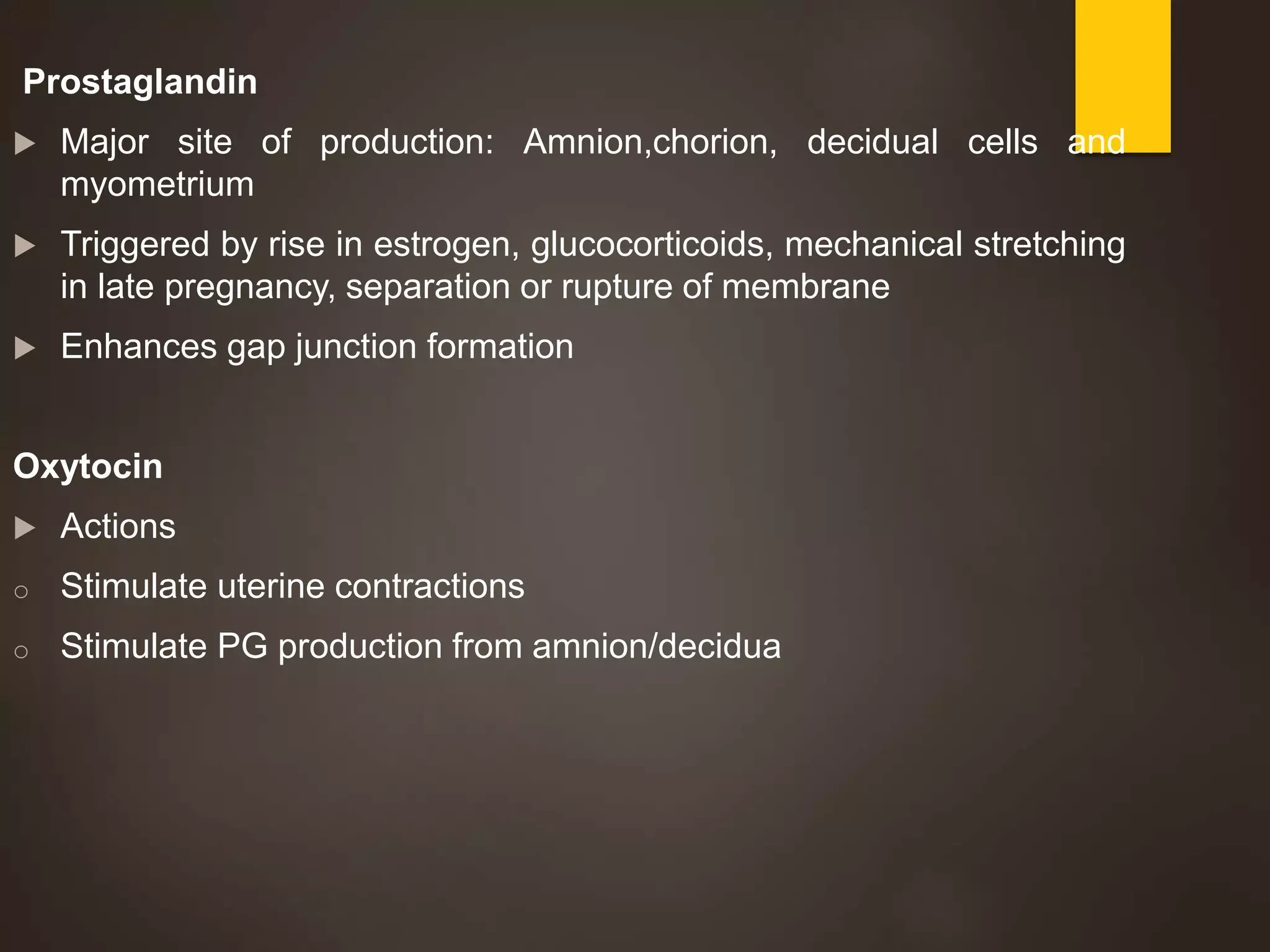
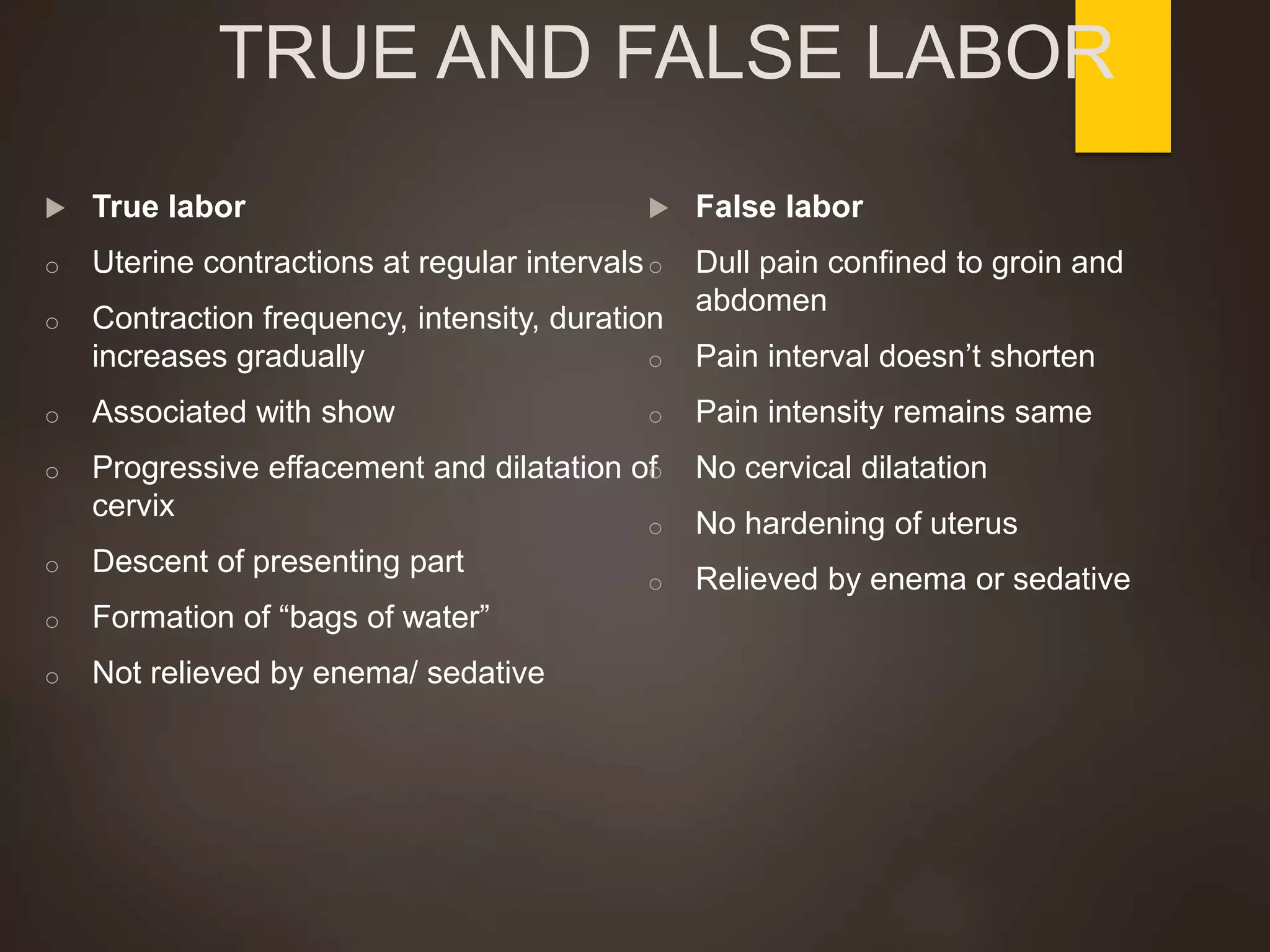
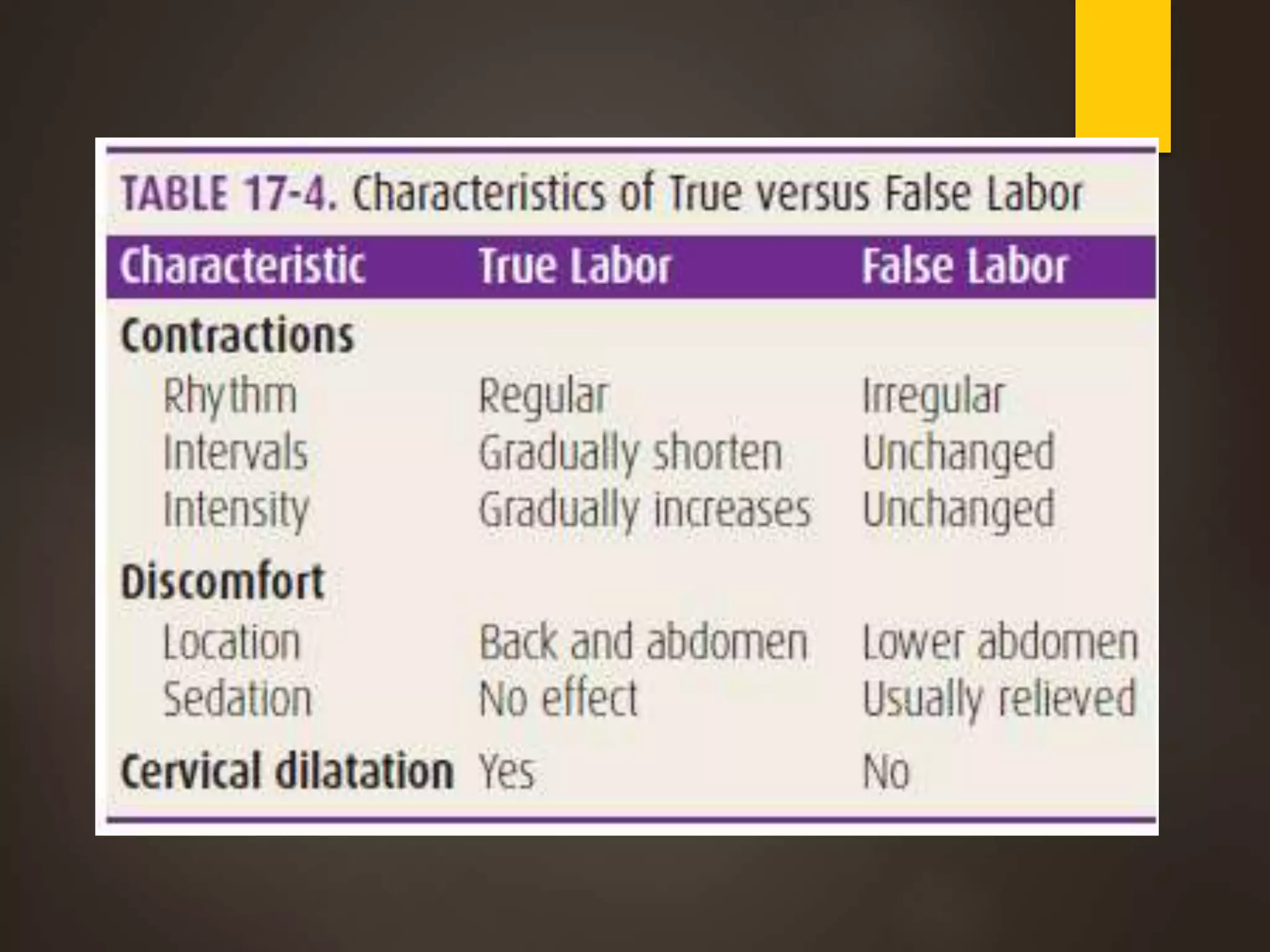
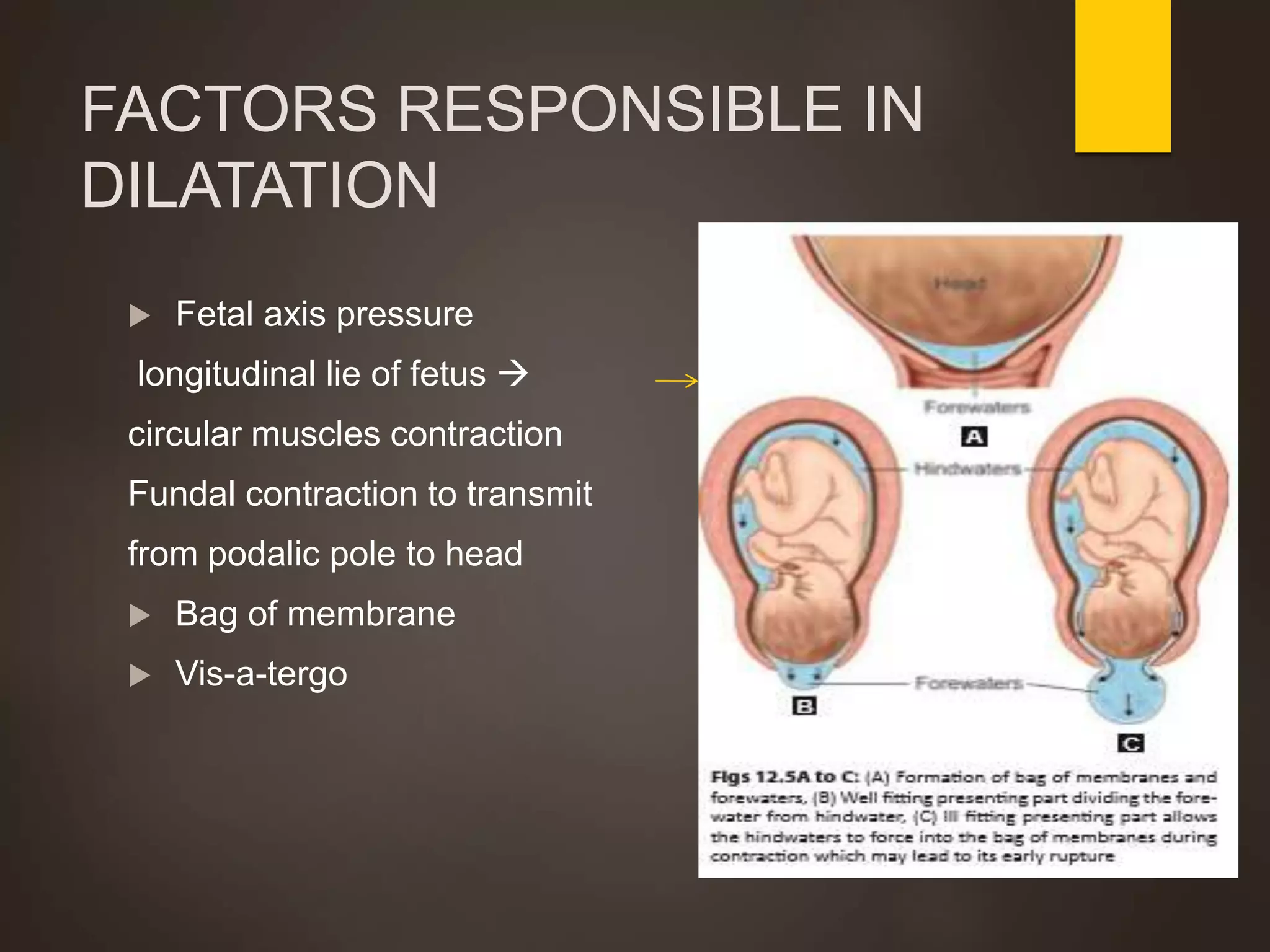
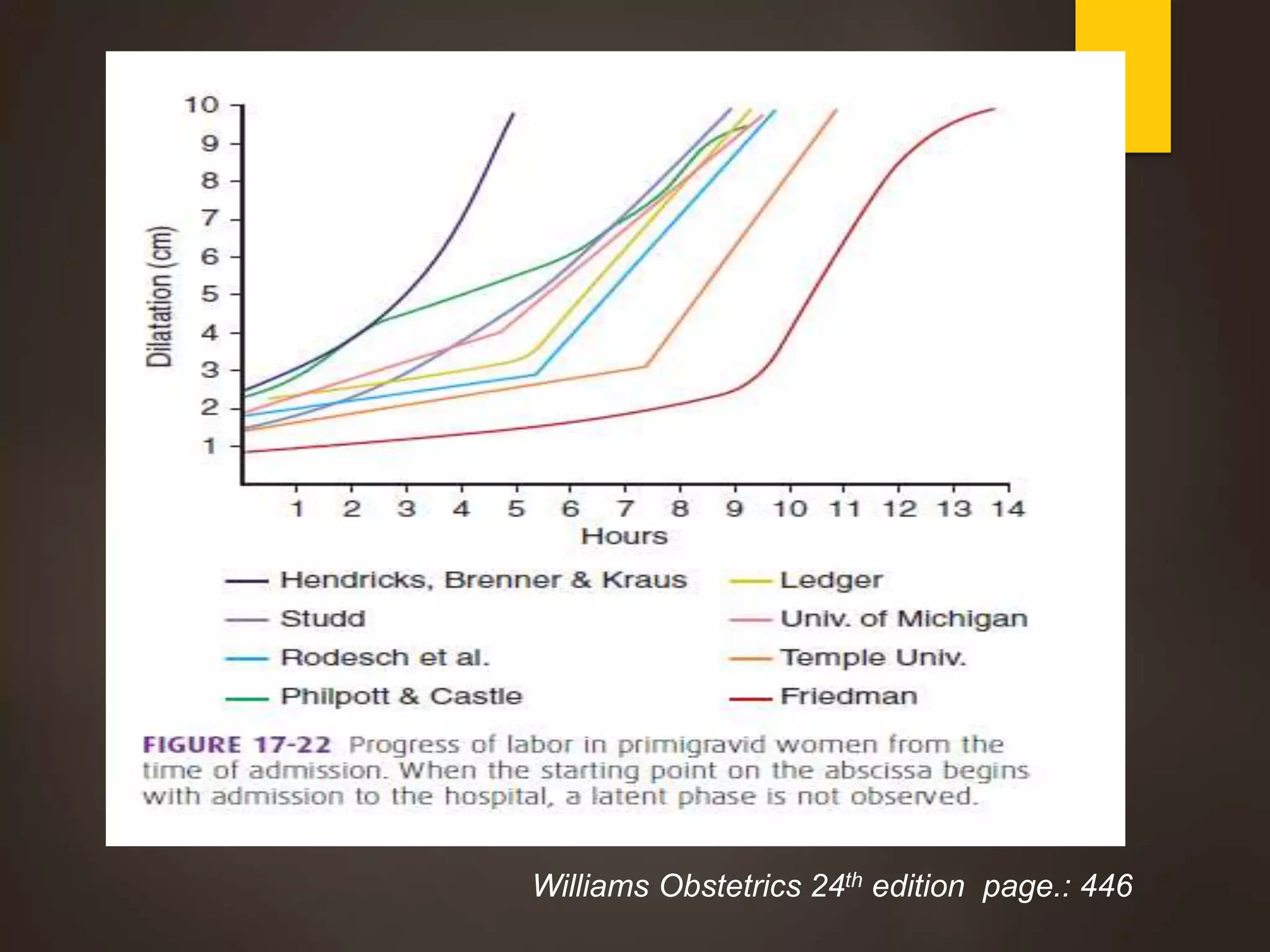
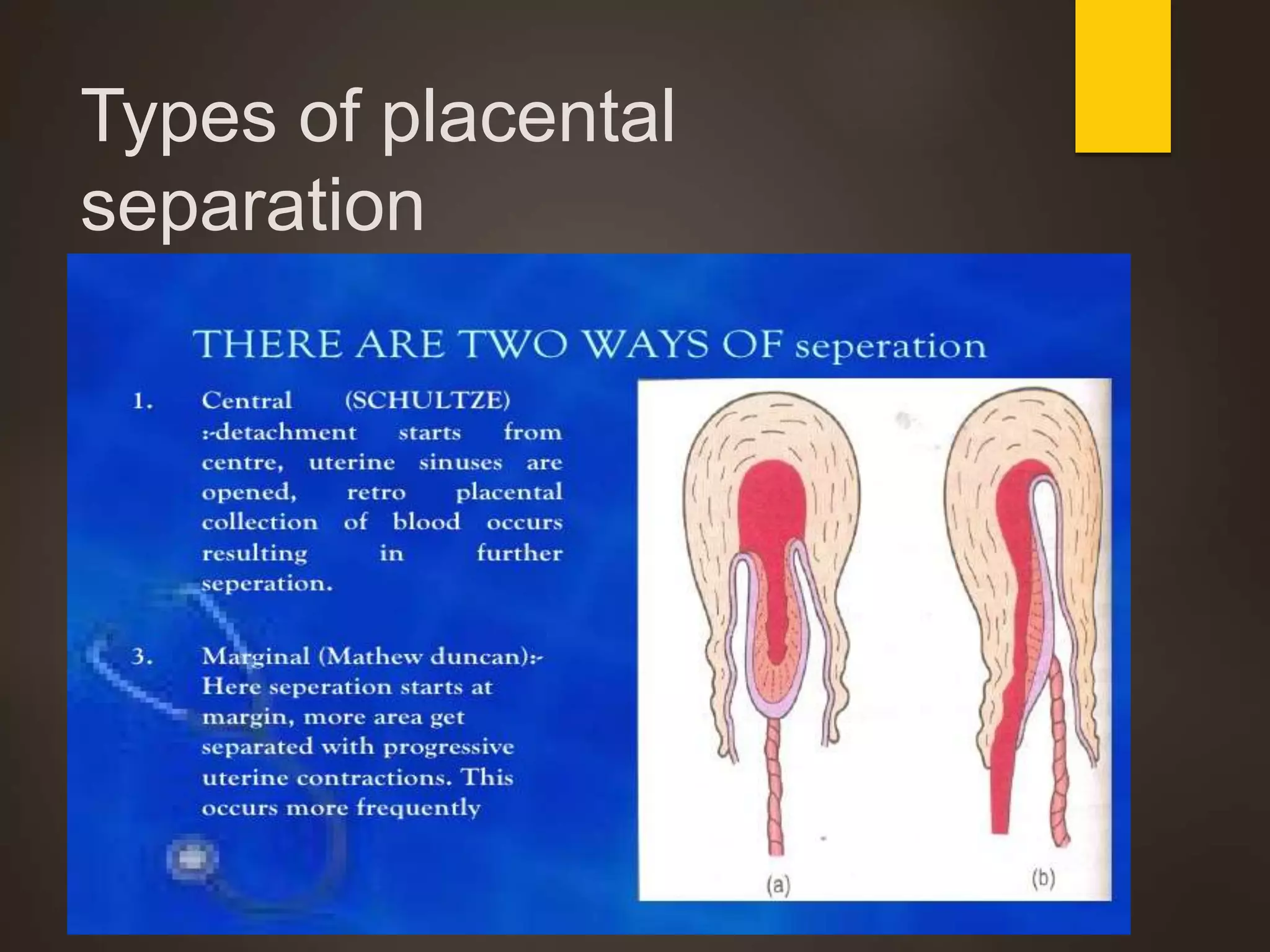
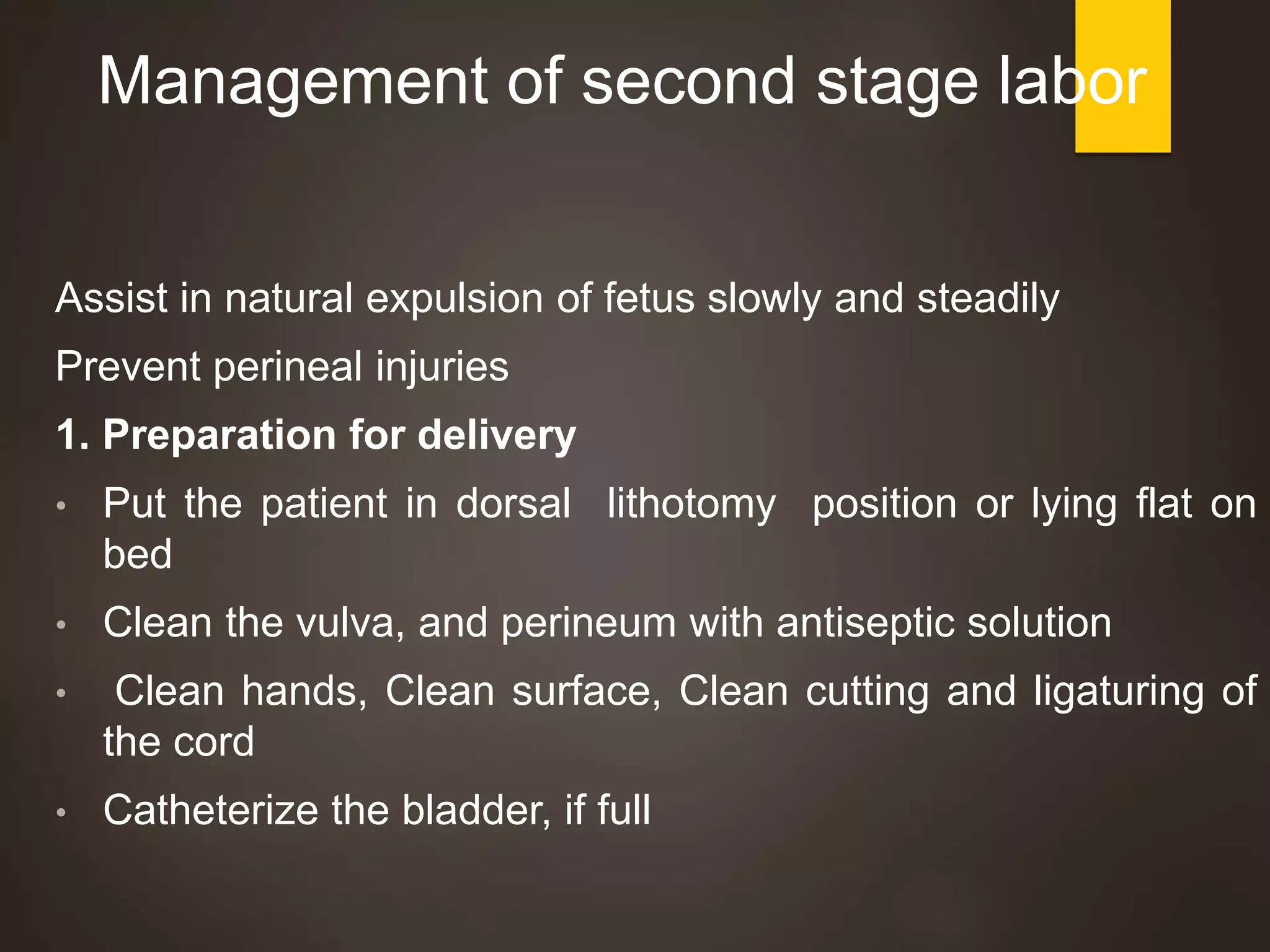
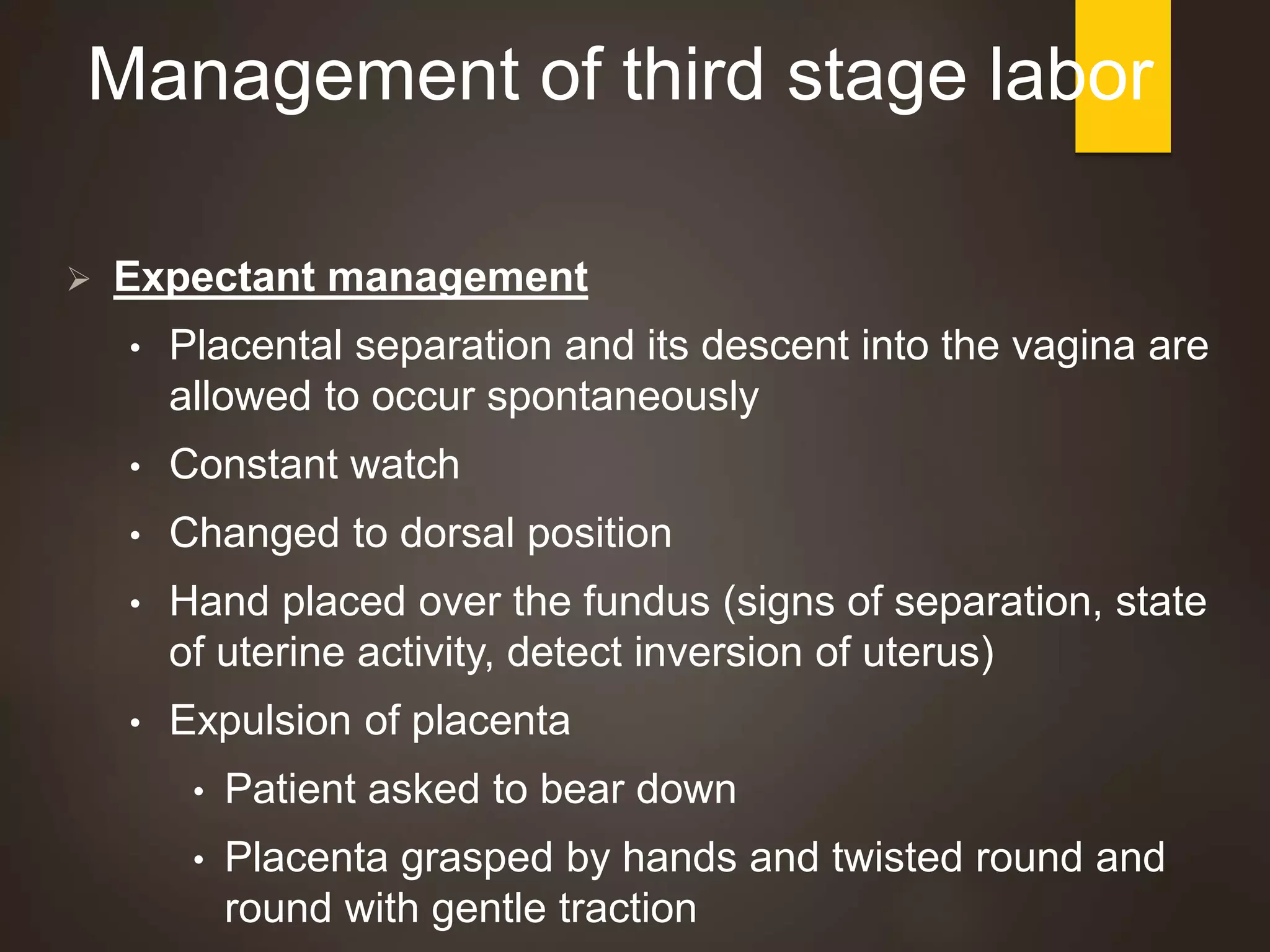
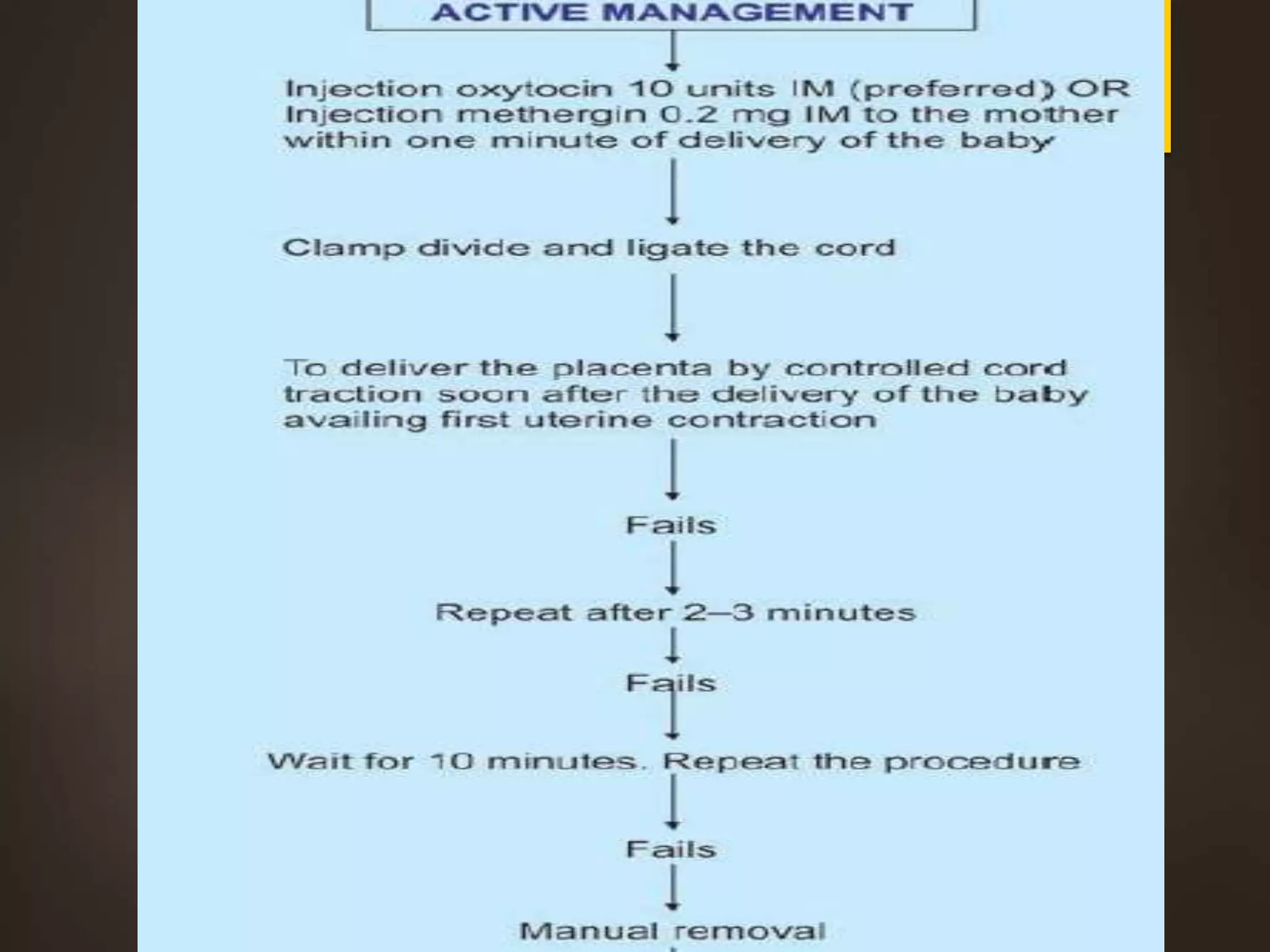
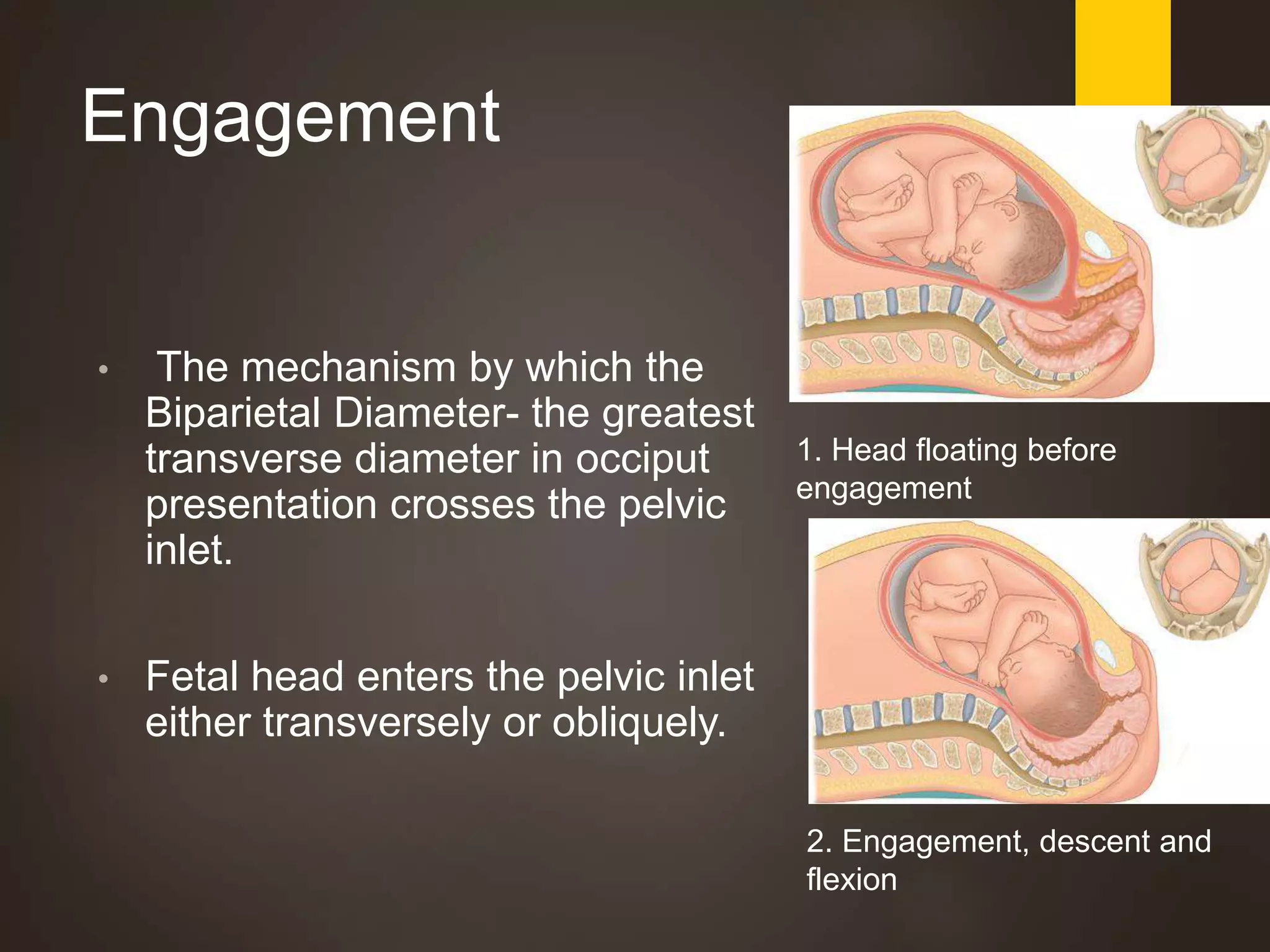
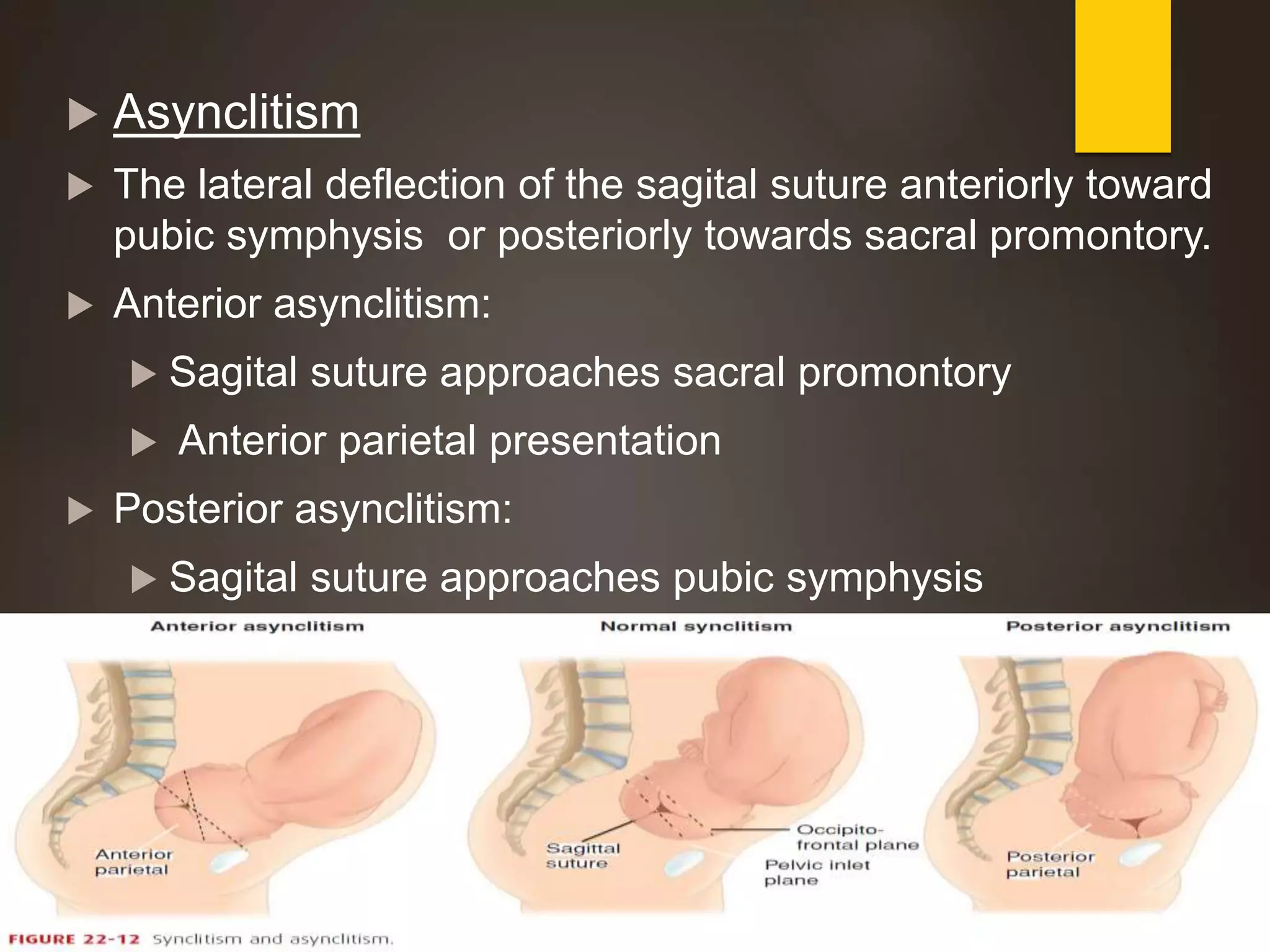
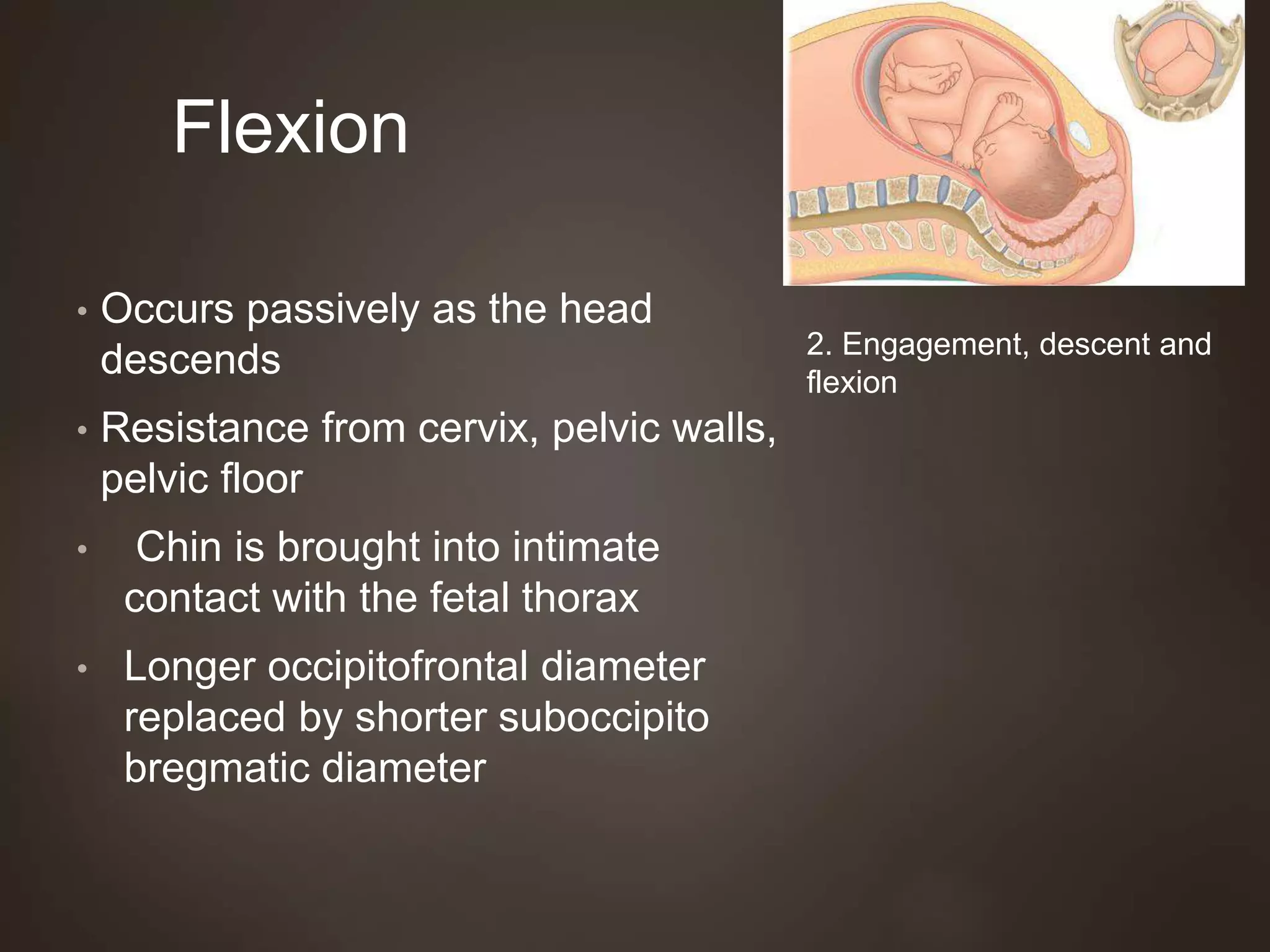
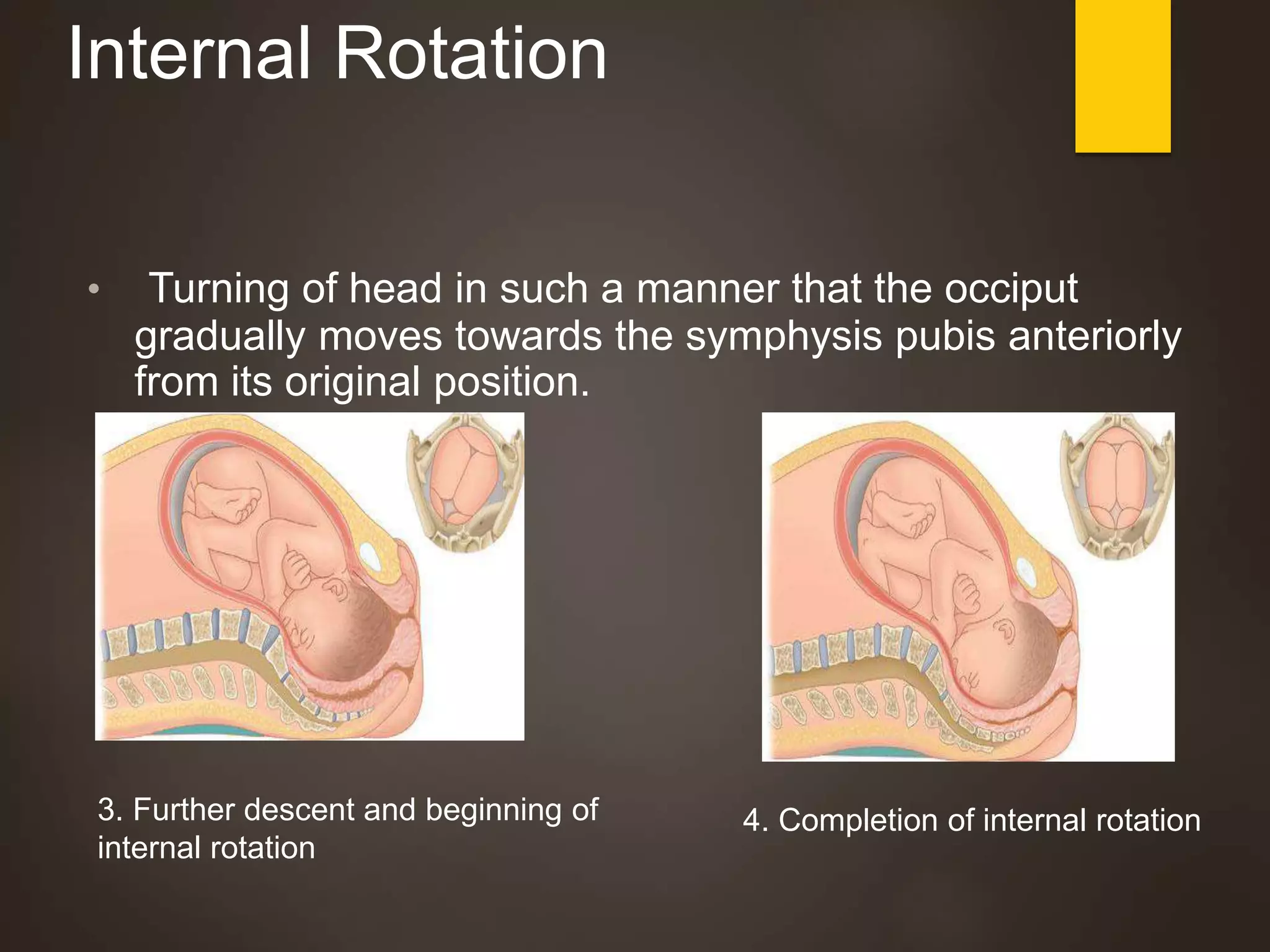
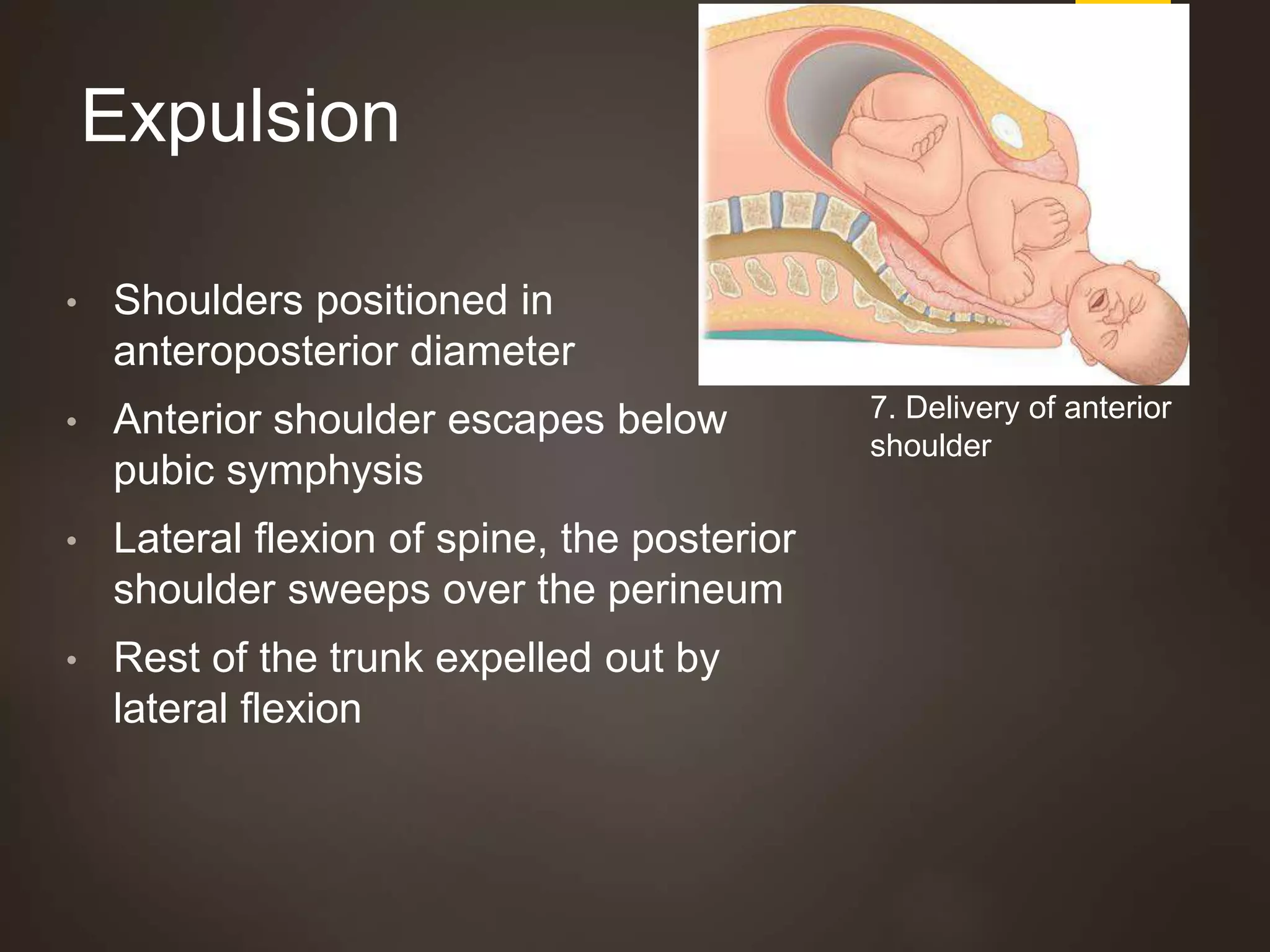
The document outlines the pathophysiology of normal labor, defined as a series of events leading to the expulsion of the fetus and placenta from the womb. It details the criteria for the onset of labor, stages of labor, and the physiological processes involved, along with types of contractions and management strategies for each phase of labor. Key concepts include the hormonal influences, stages of labor, cardinal movements during delivery, and complications associated with different degrees of laceration.