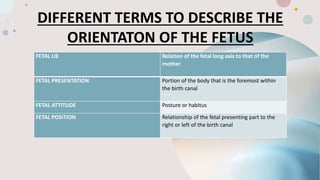
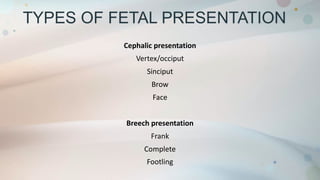
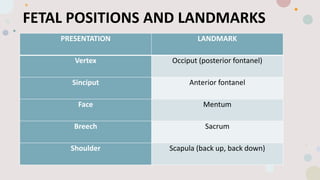
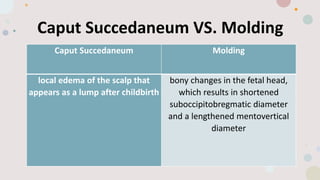
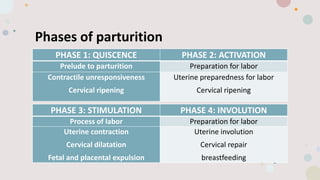
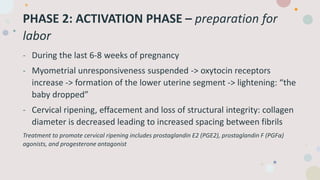
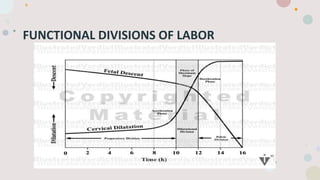
This document discusses normal labor and delivery. It begins by defining various terms used to describe the fetal position and presentation. It then describes the different types of fetal presentations including cephalic and breech. It discusses the phases of labor including quiescence, activation, stimulation and involution. It explains the three stages of labor and the cardinal movements. It also describes cervical dilatation phases including latent, active and deceleration. Finally, it discusses placental delivery and mechanisms.