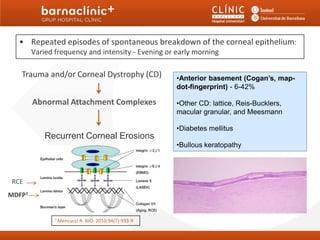
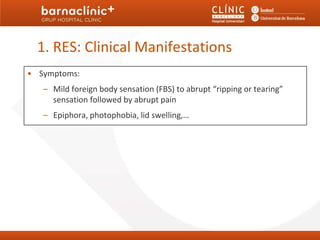
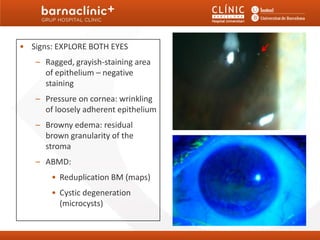
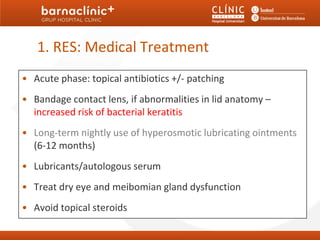
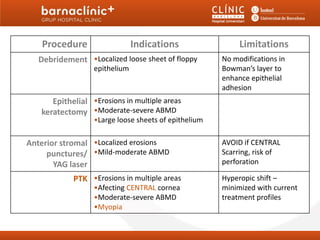
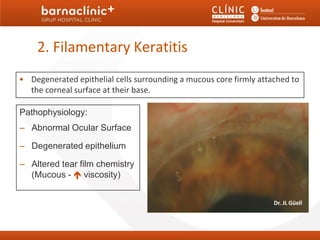
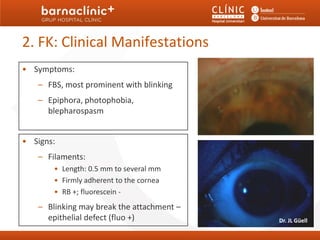
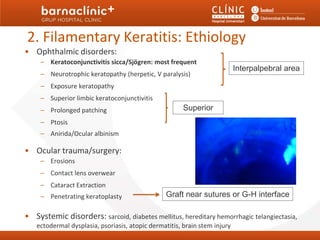
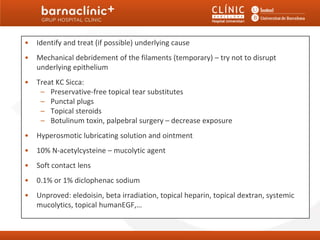
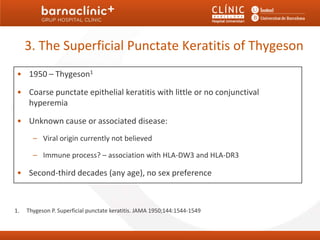
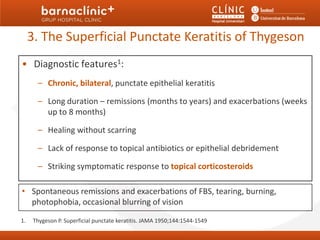
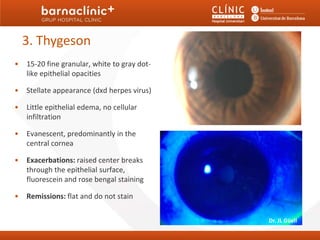
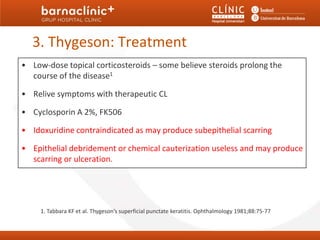
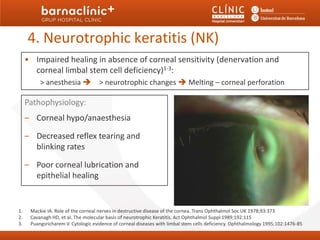
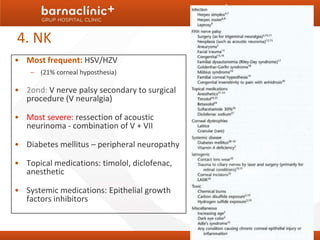
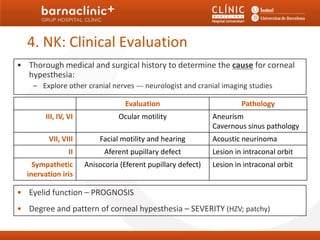
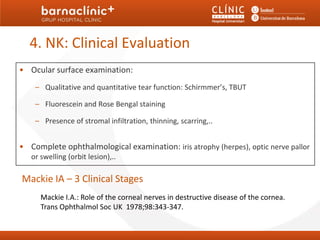
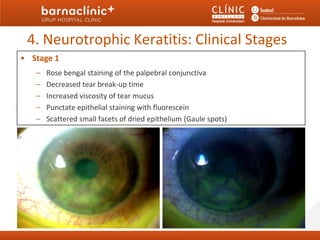
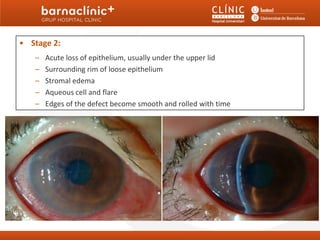
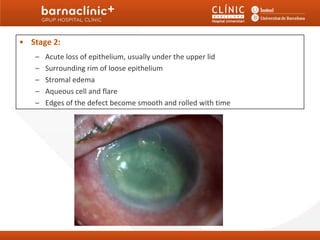
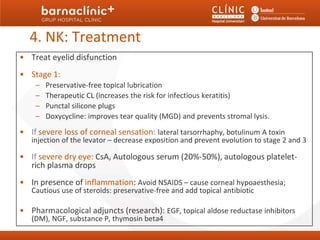
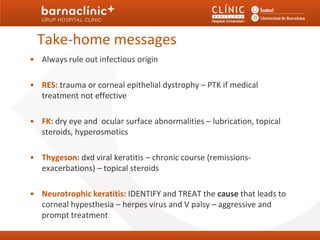
This document discusses different types of noninfectious keratitis, including recurrent erosion syndrome, filamentary keratitis, Thygeson's superficial punctate keratitis, and neurotrophic keratitis. Recurrent erosion syndrome involves repeated breakdown of the corneal epithelium and is associated with trauma, corneal dystrophy, or abnormal attachment complexes. Filamentary keratitis features filaments of degenerated epithelial cells firmly attached to the cornea. Thygeson's keratitis presents as chronic, bilateral punctate epithelial keratitis of unknown cause. Neurotrophic keratitis results from impaired corneal healing due to denervation and involves decreased tearing and blinking. Treatment focuses on managing underlying causes and symptoms for each condition.