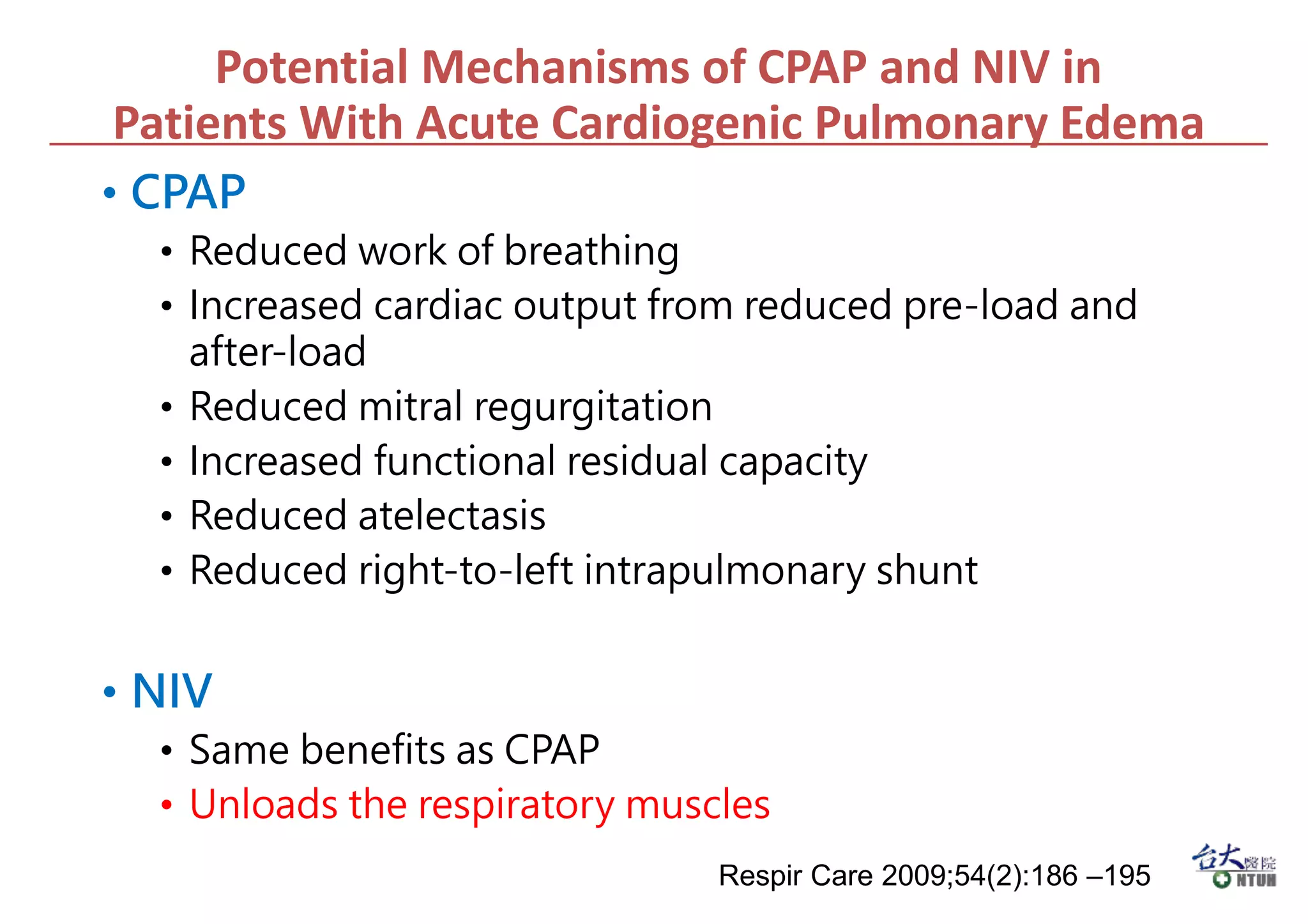
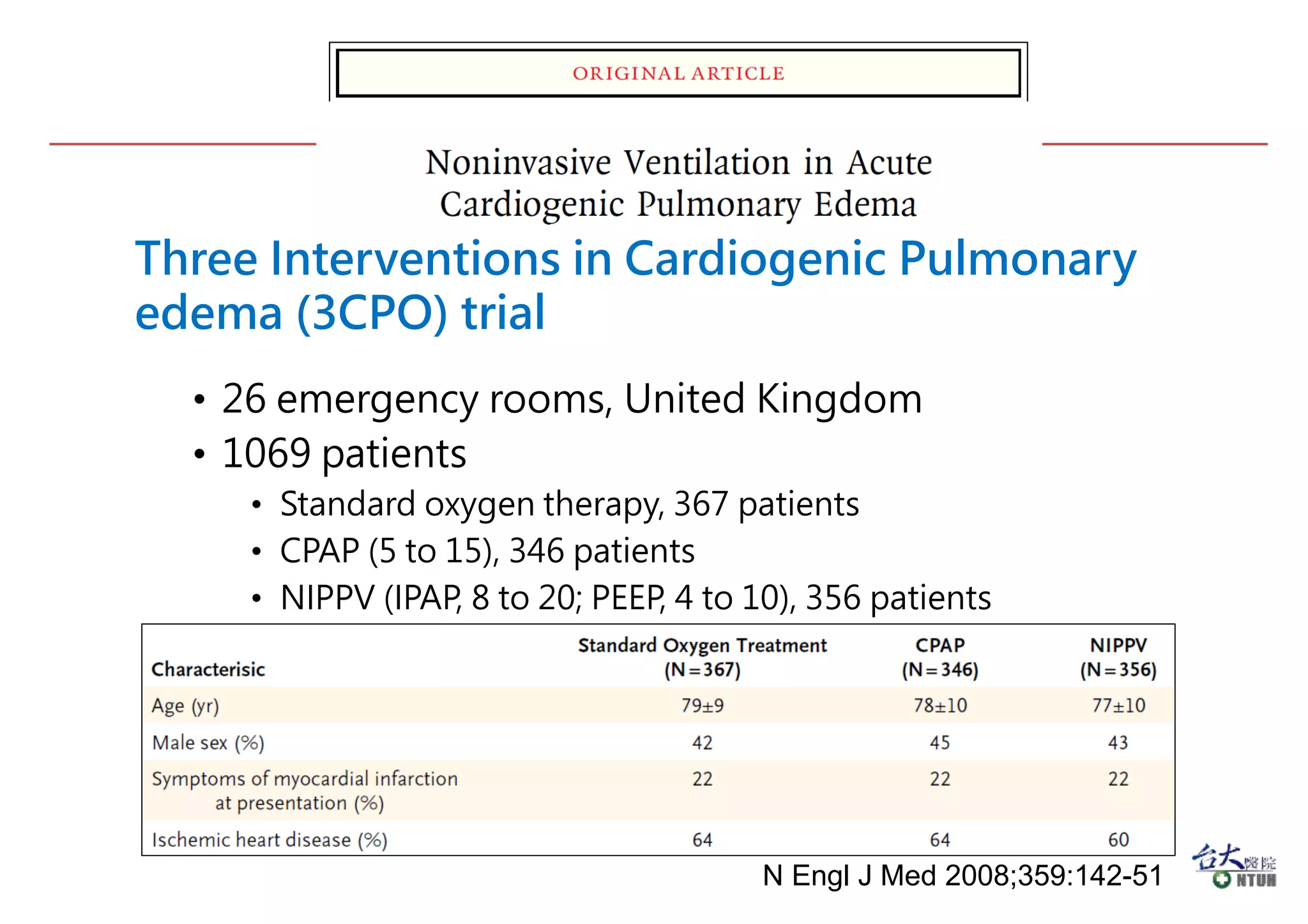
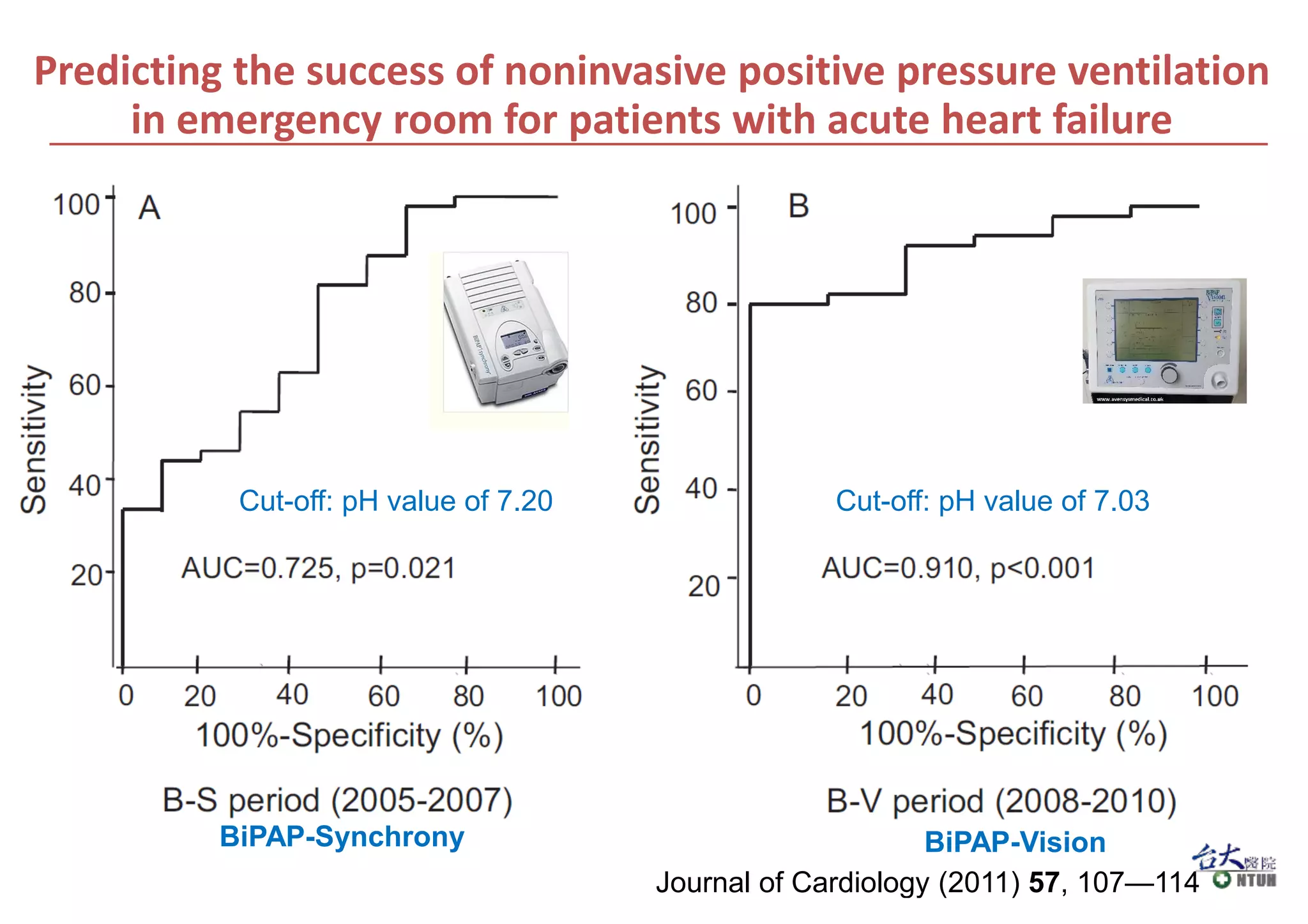
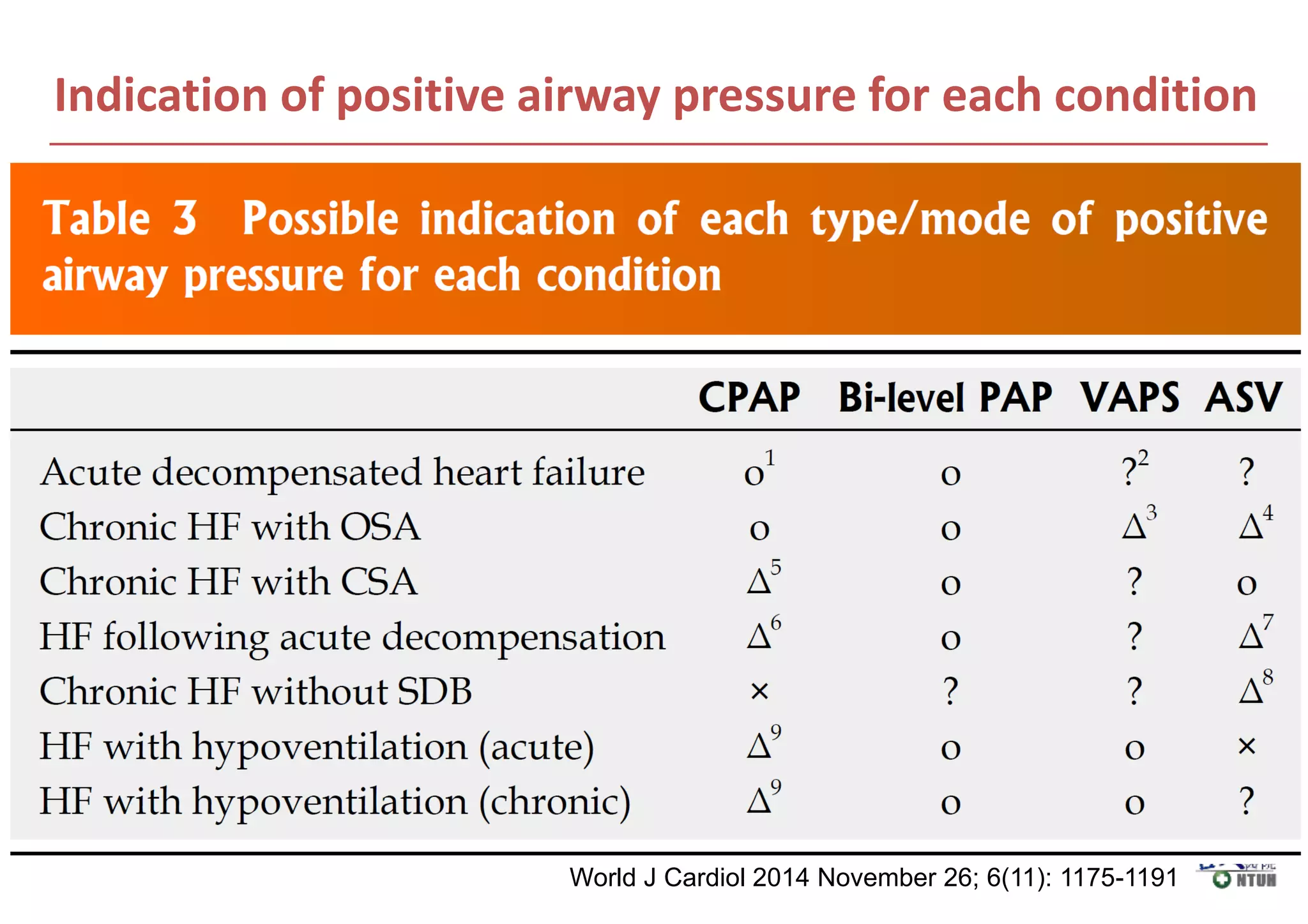
This document discusses the use of non-invasive ventilation (NIV) such as CPAP and BiPAP in the treatment of acute and chronic heart failure. For acute heart failure with pulmonary edema:
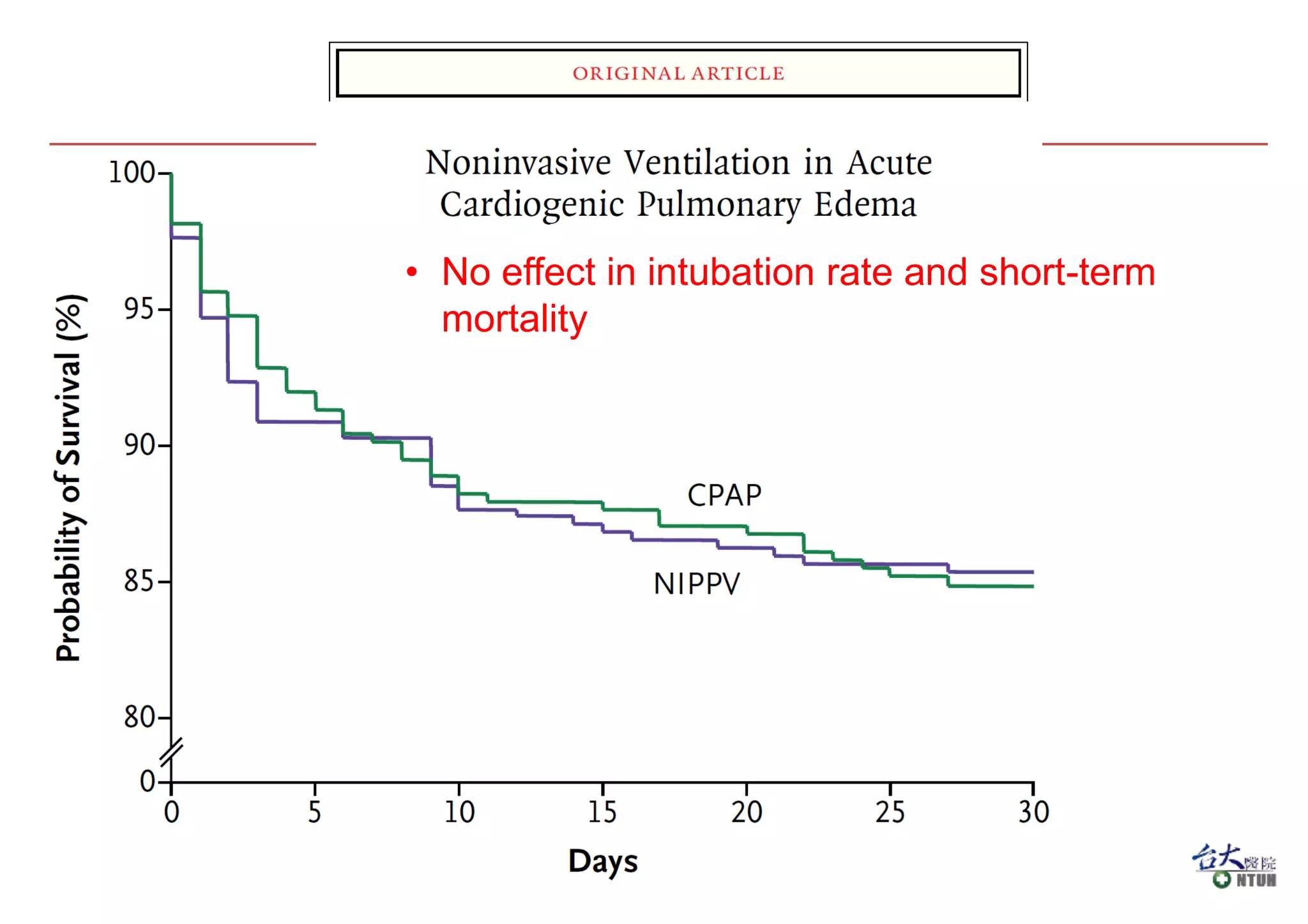
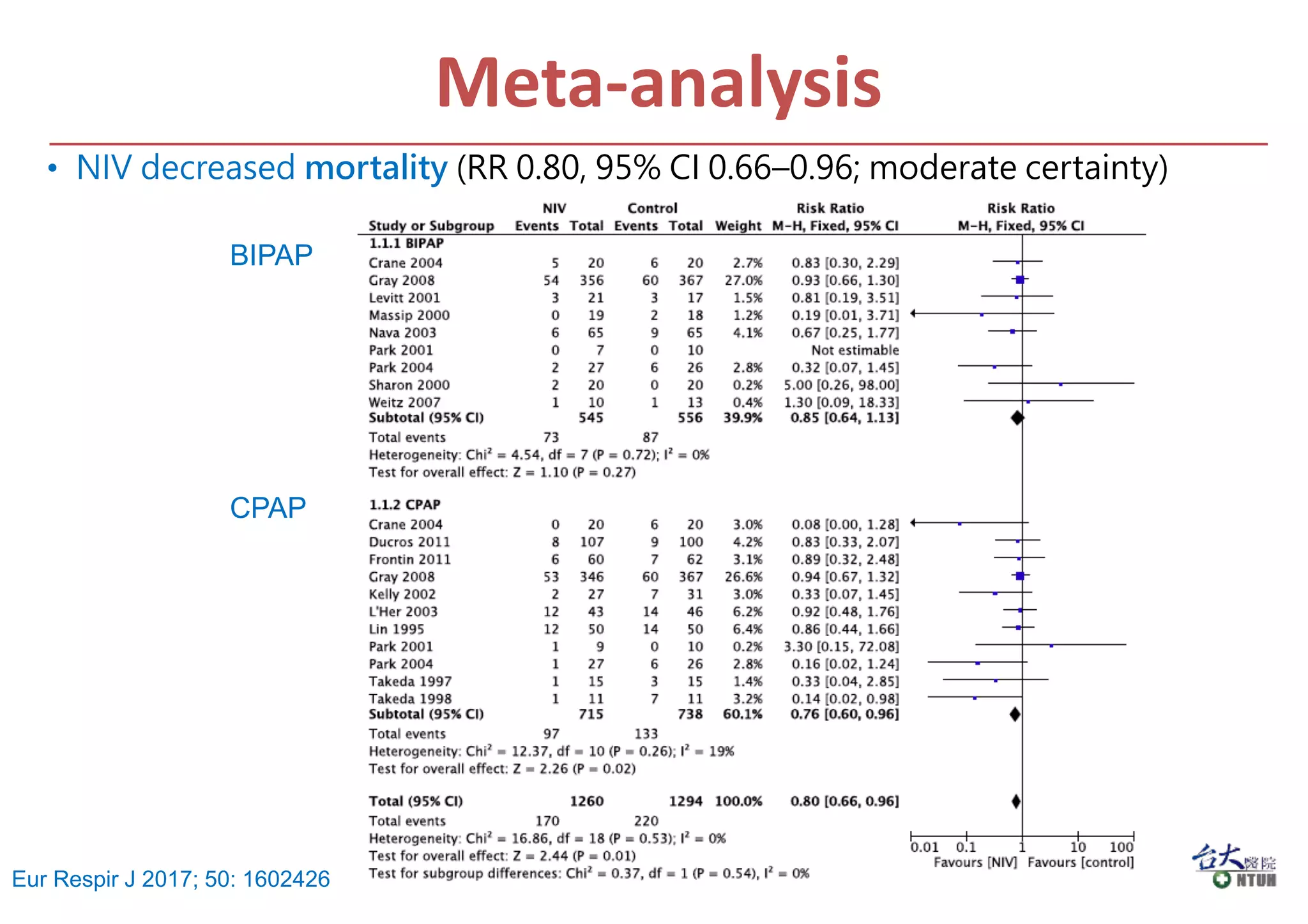
1) Meta-analyses found that NIV decreases the need for intubation and reduces hospital mortality compared to standard oxygen therapy alone.
2) NIV is not associated with increased risk of myocardial infarction.
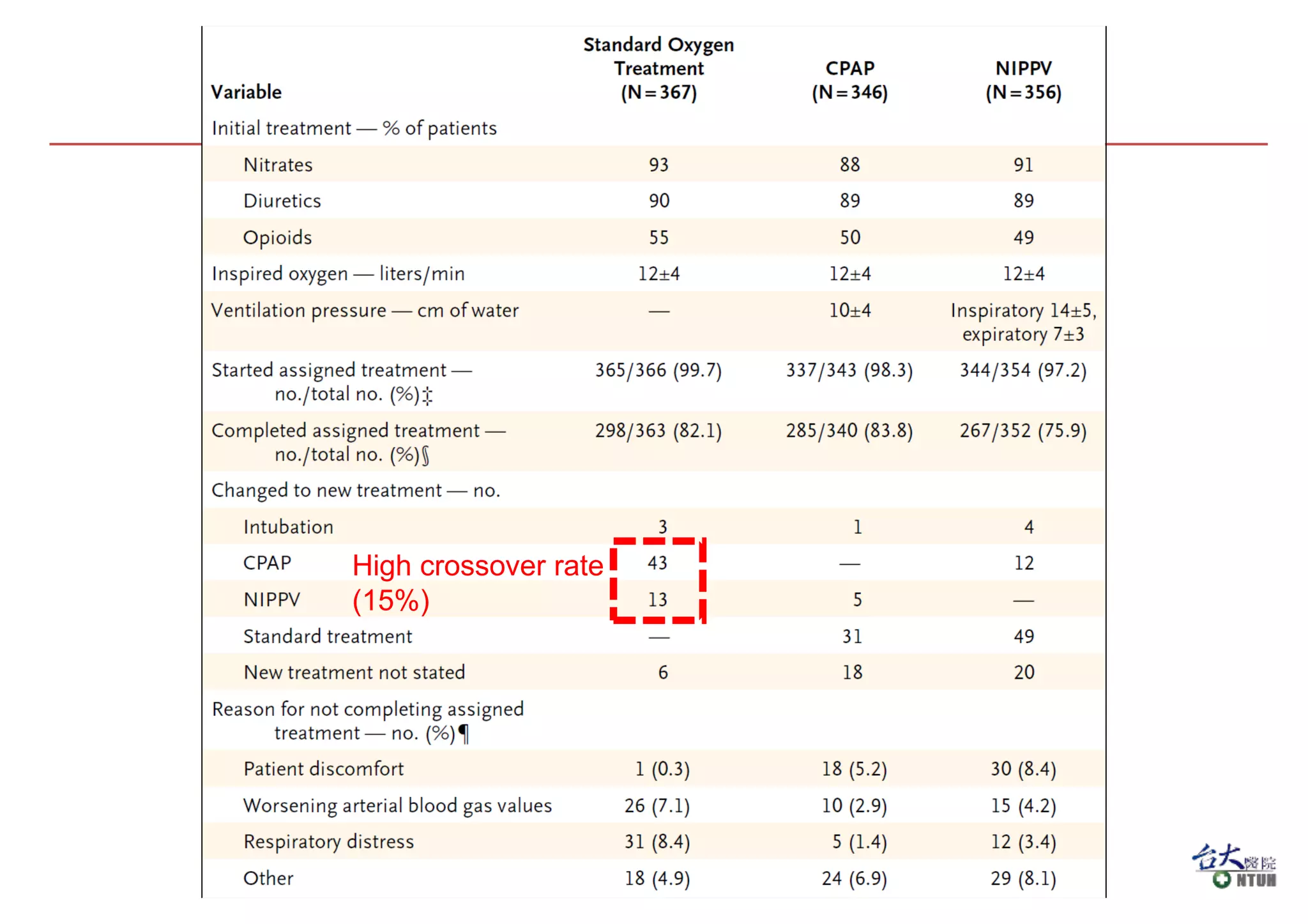
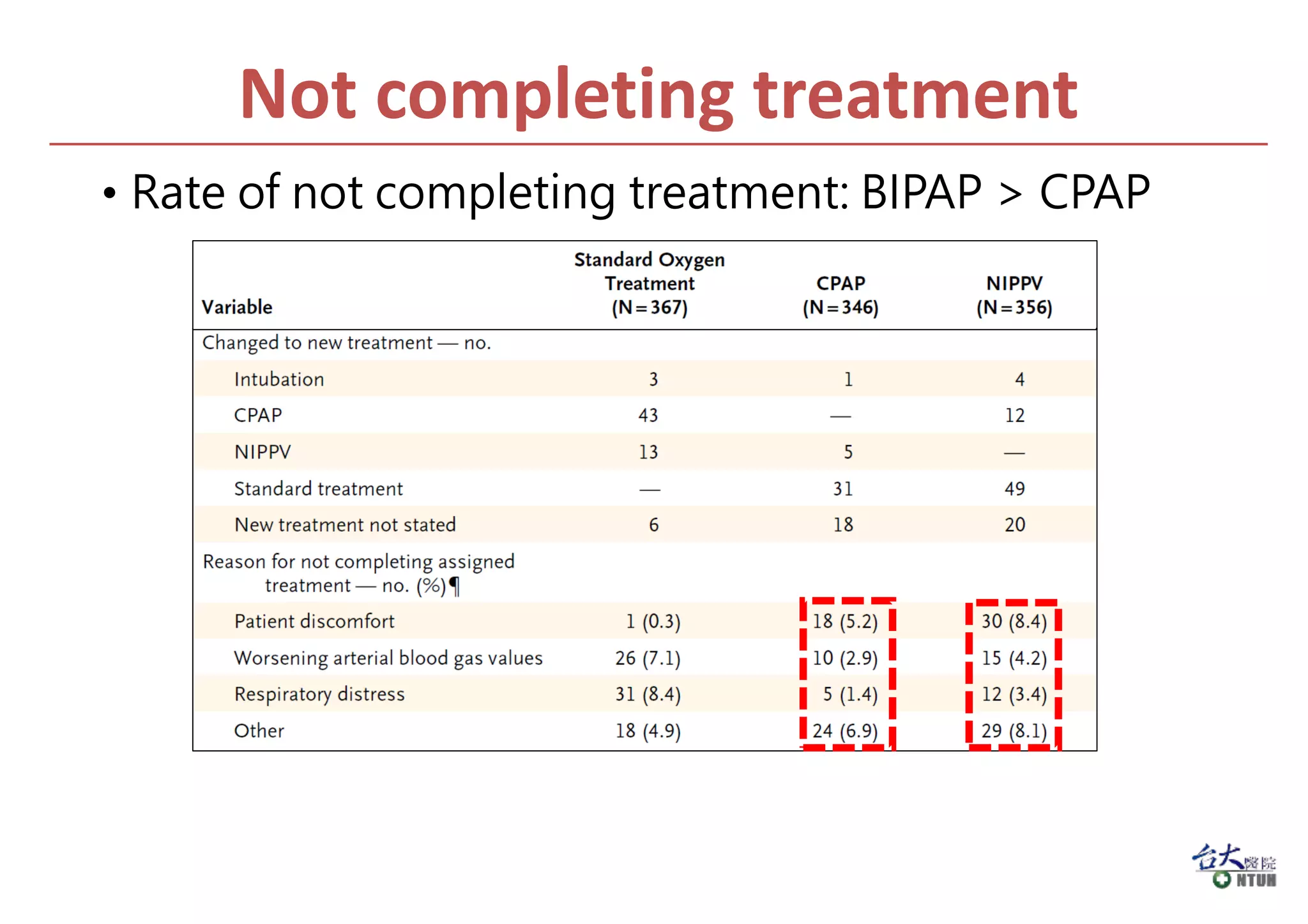
3) CPAP and BiPAP provide similar benefits but CPAP has some advantages of being simpler technology.
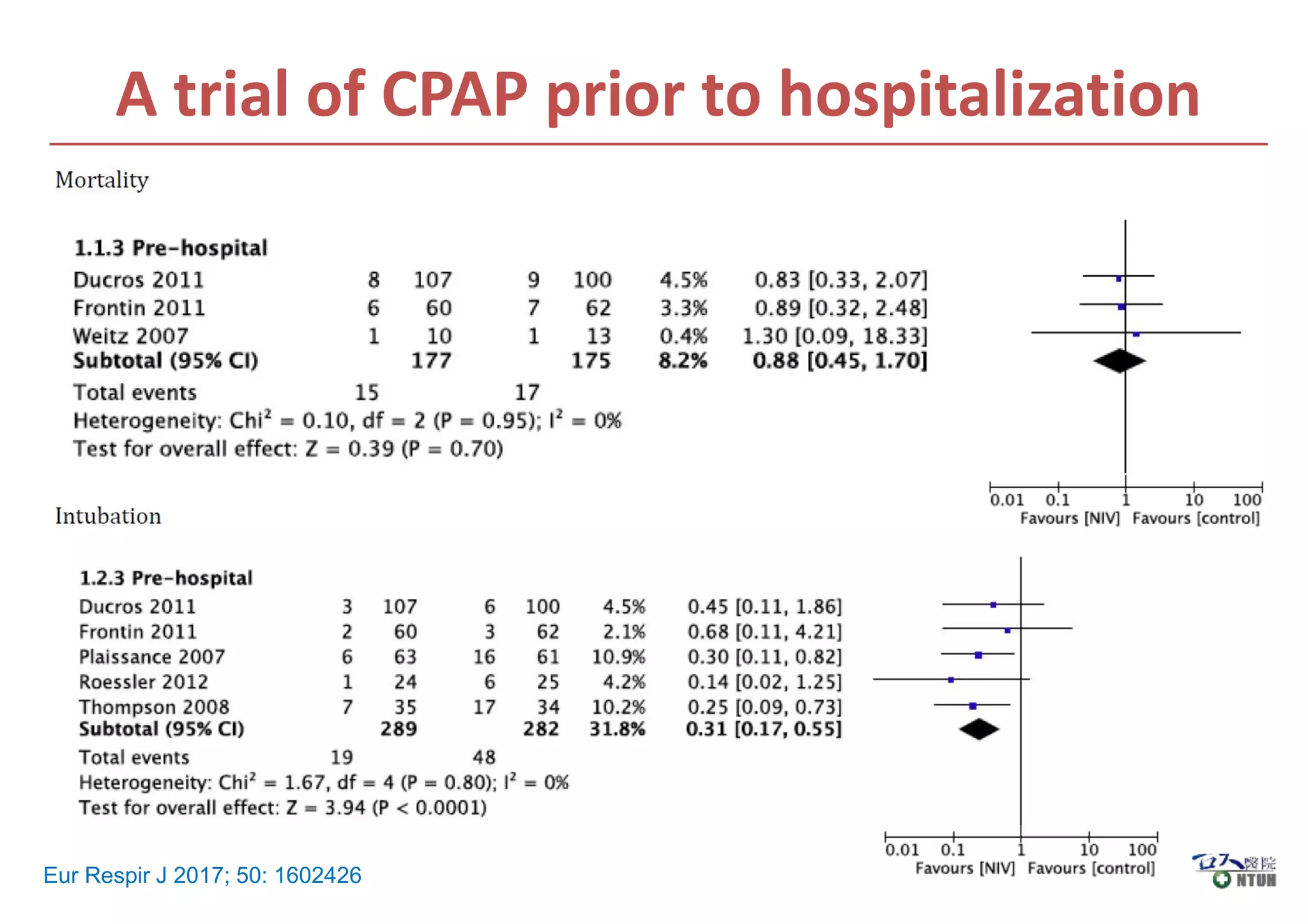
4) NIV can be used in the pre-hospital setting for cardiogenic pulmonary edema.
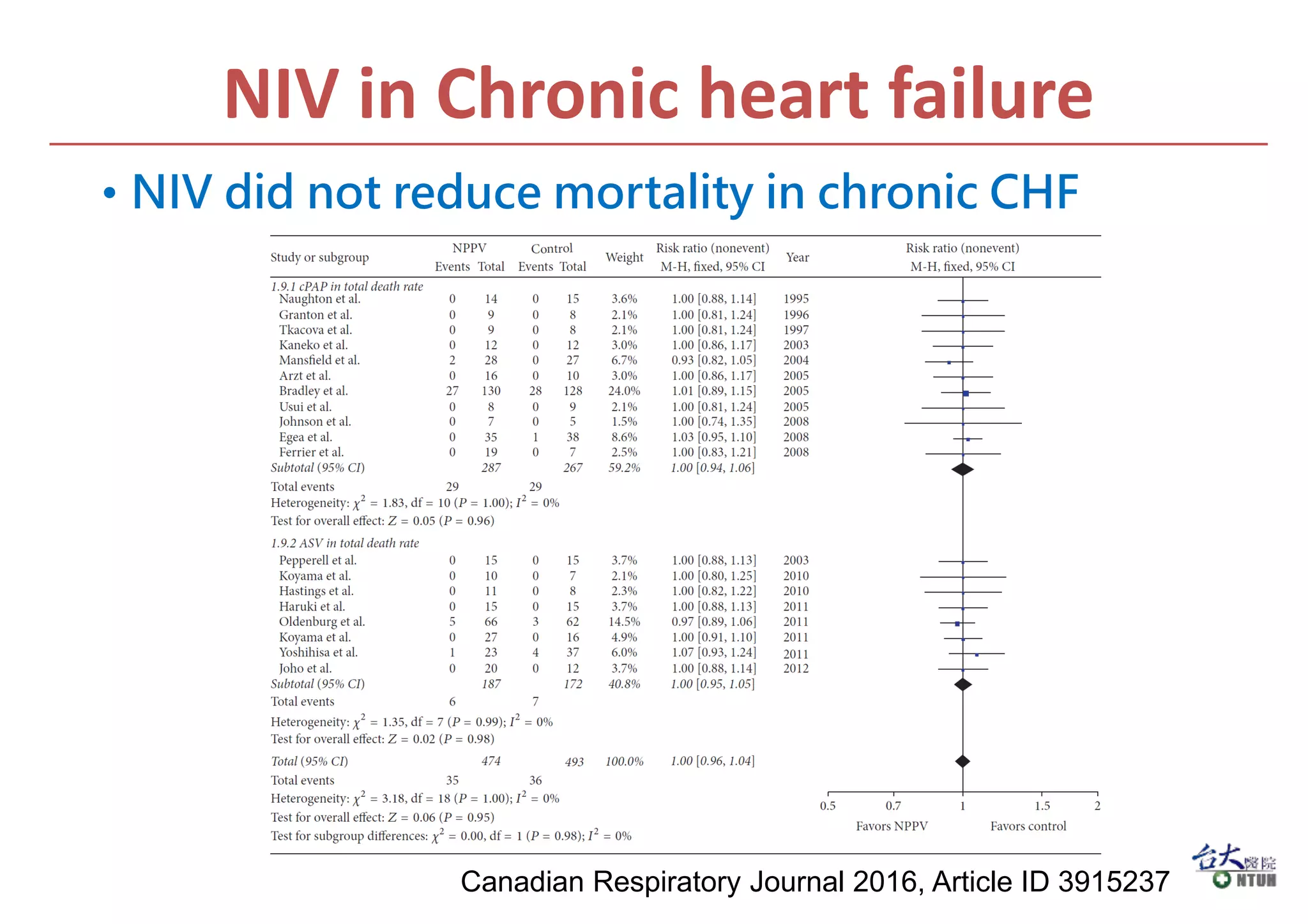
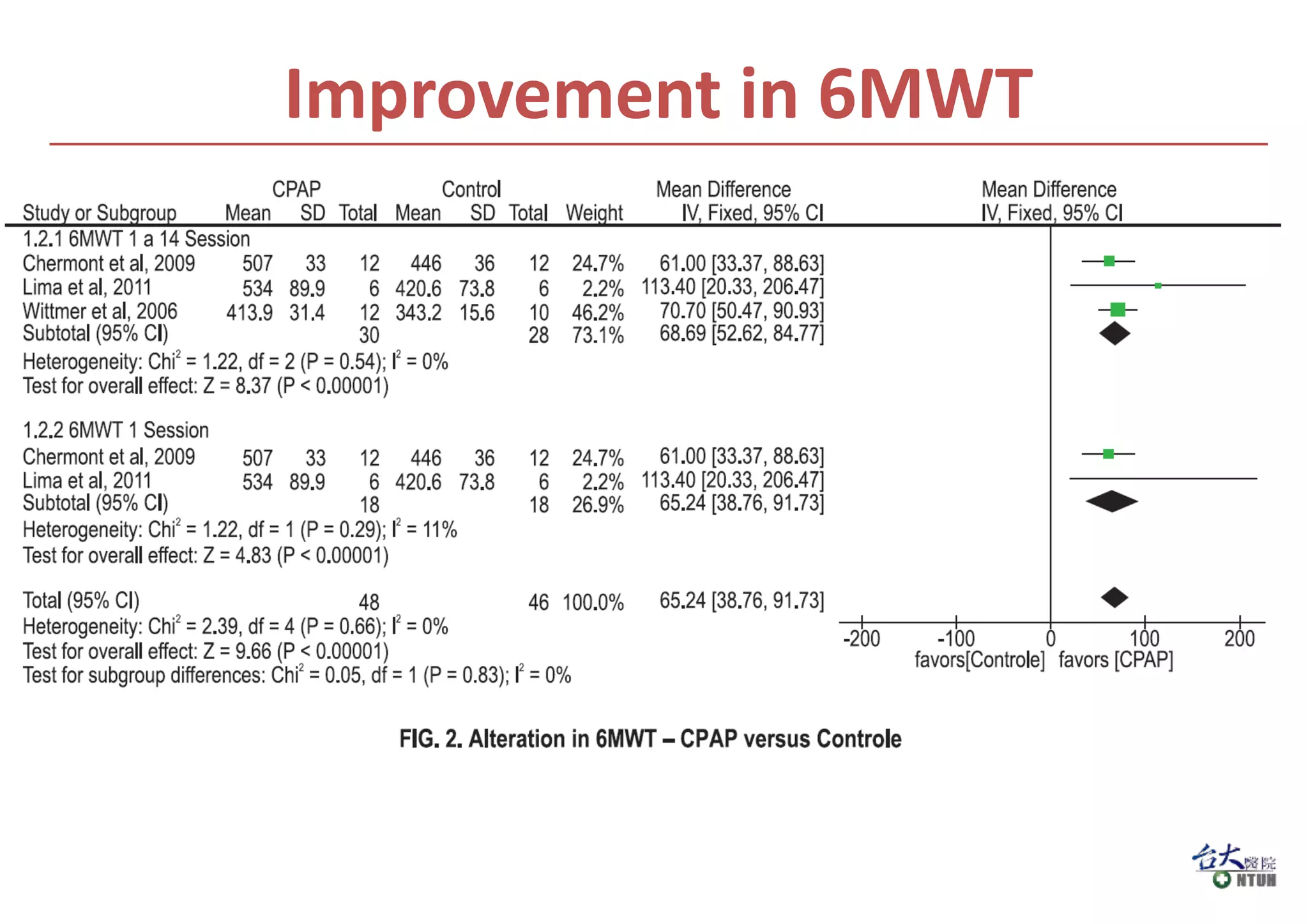
For chronic heart failure, NIV improved left ventricular ejection fraction and BNP