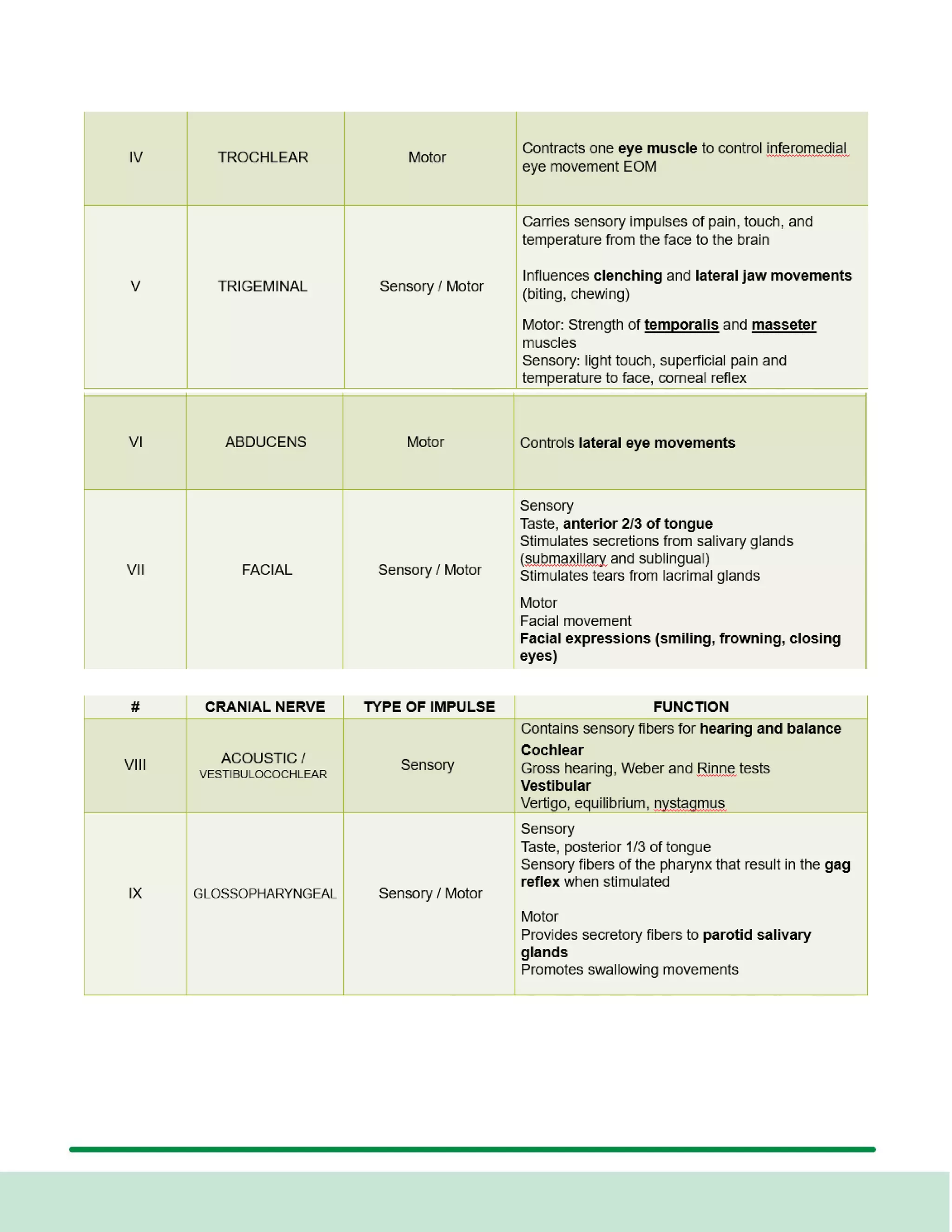
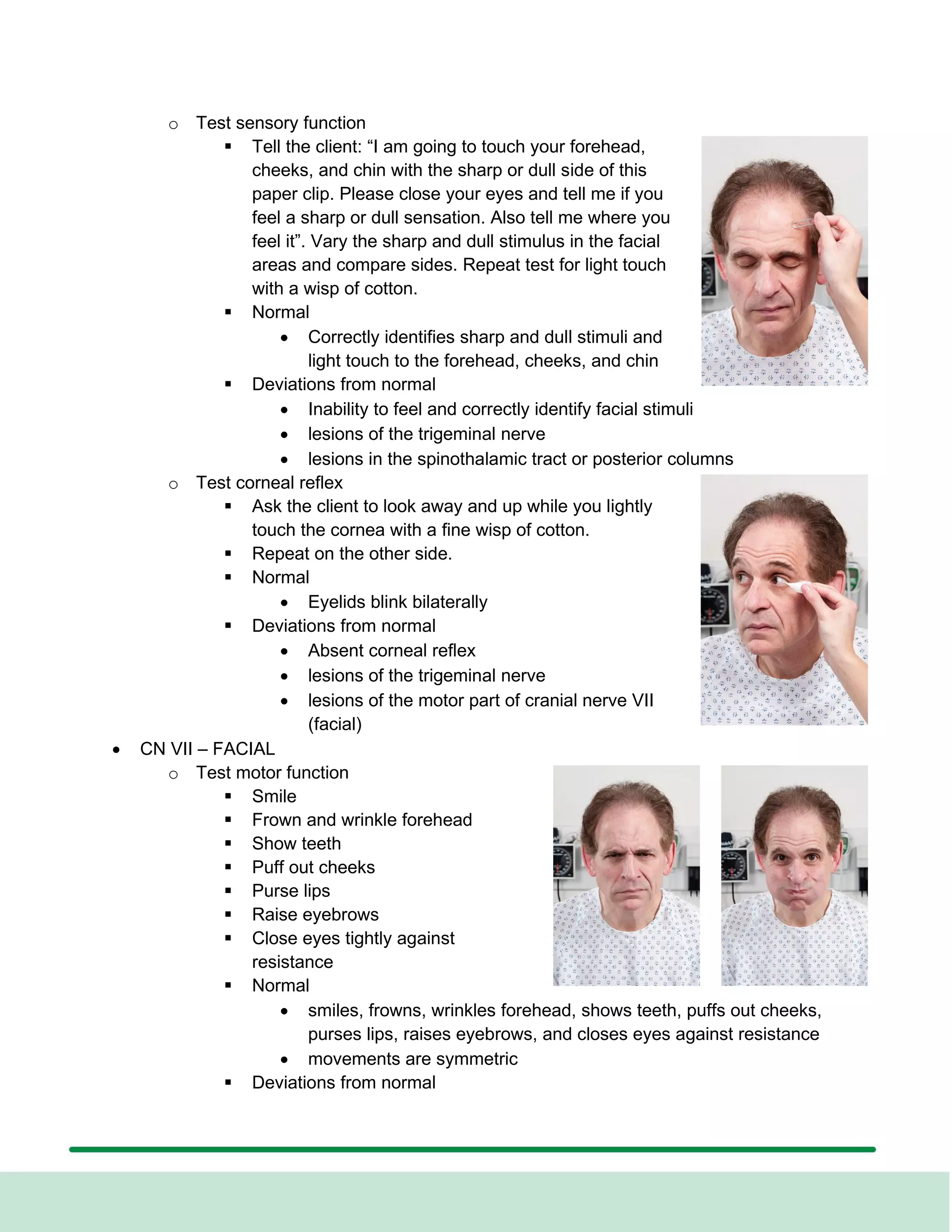
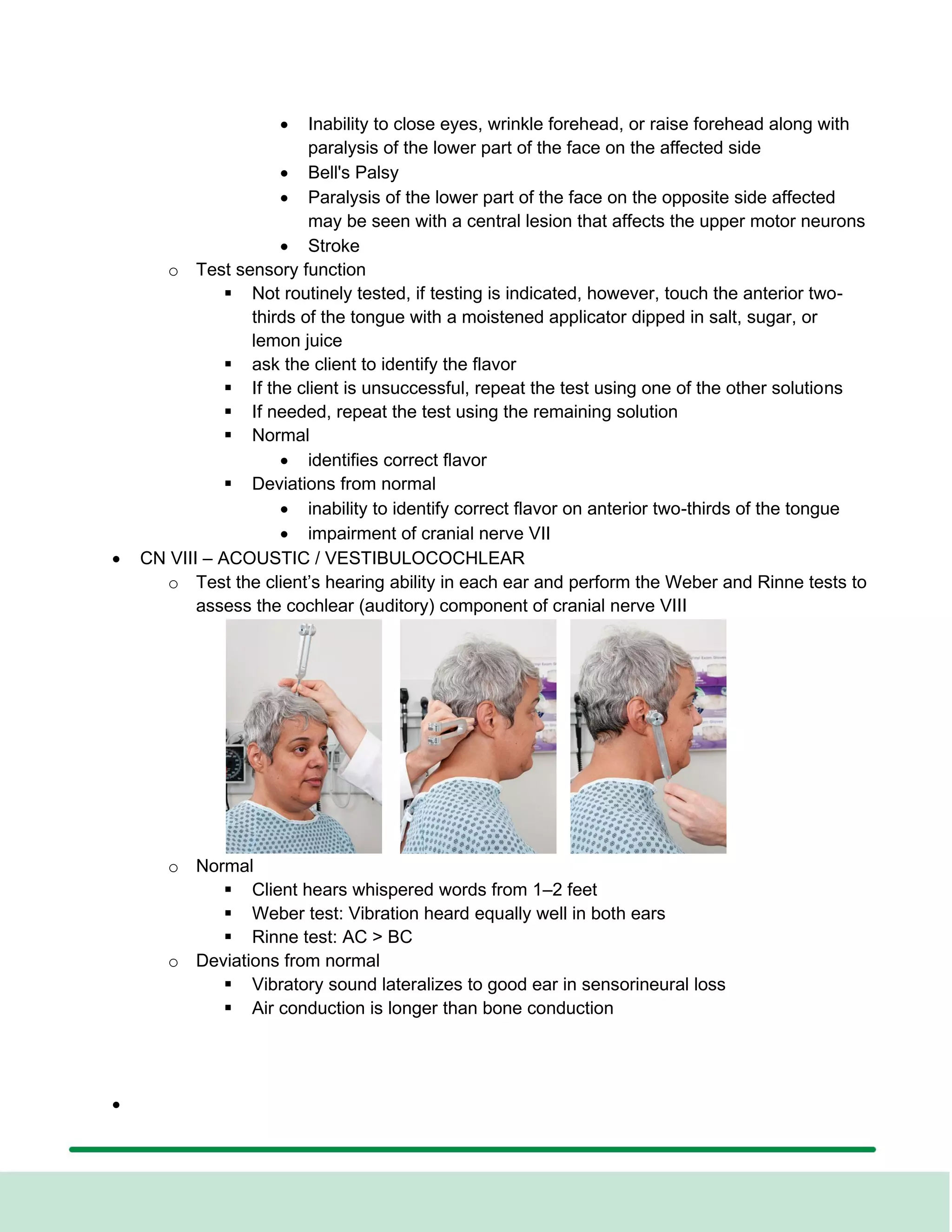
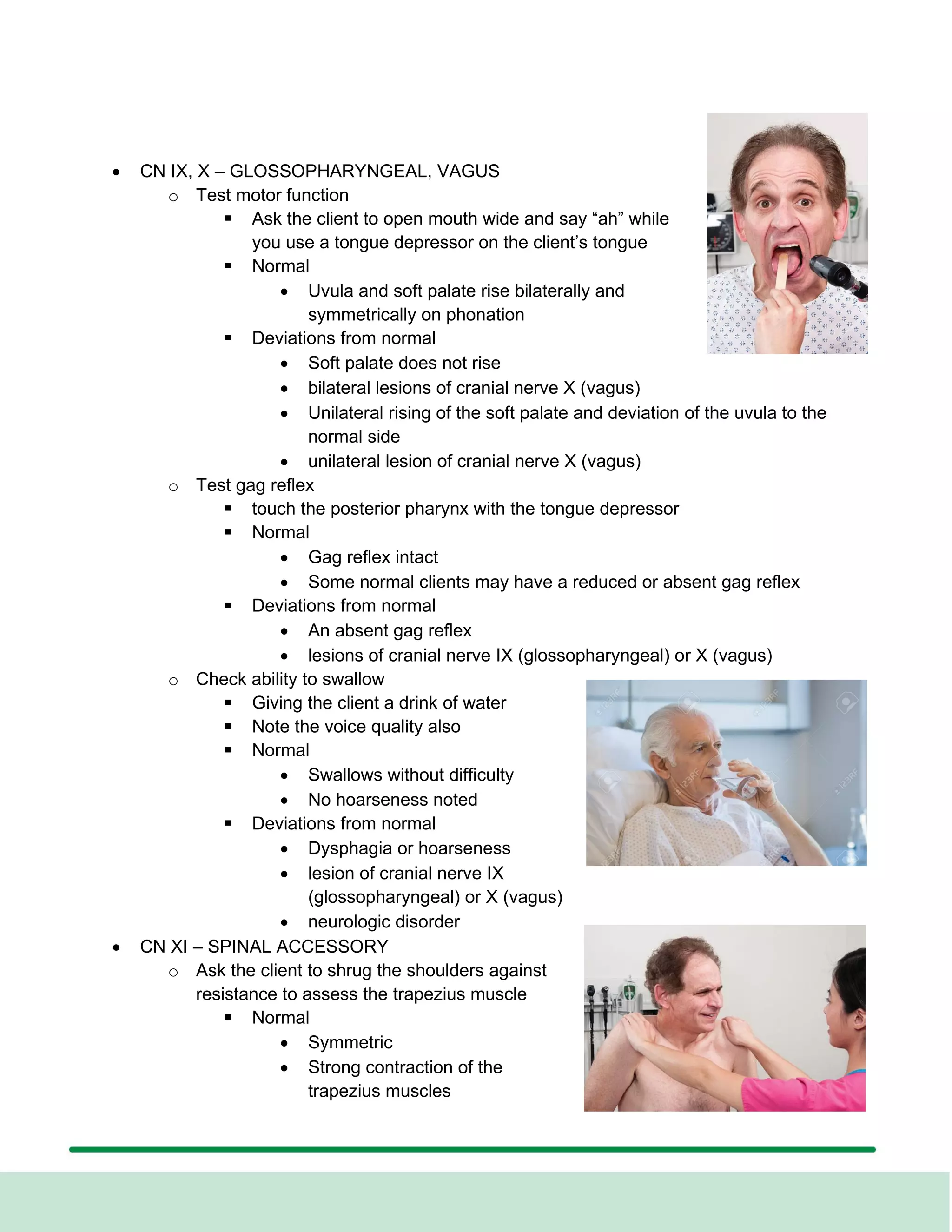
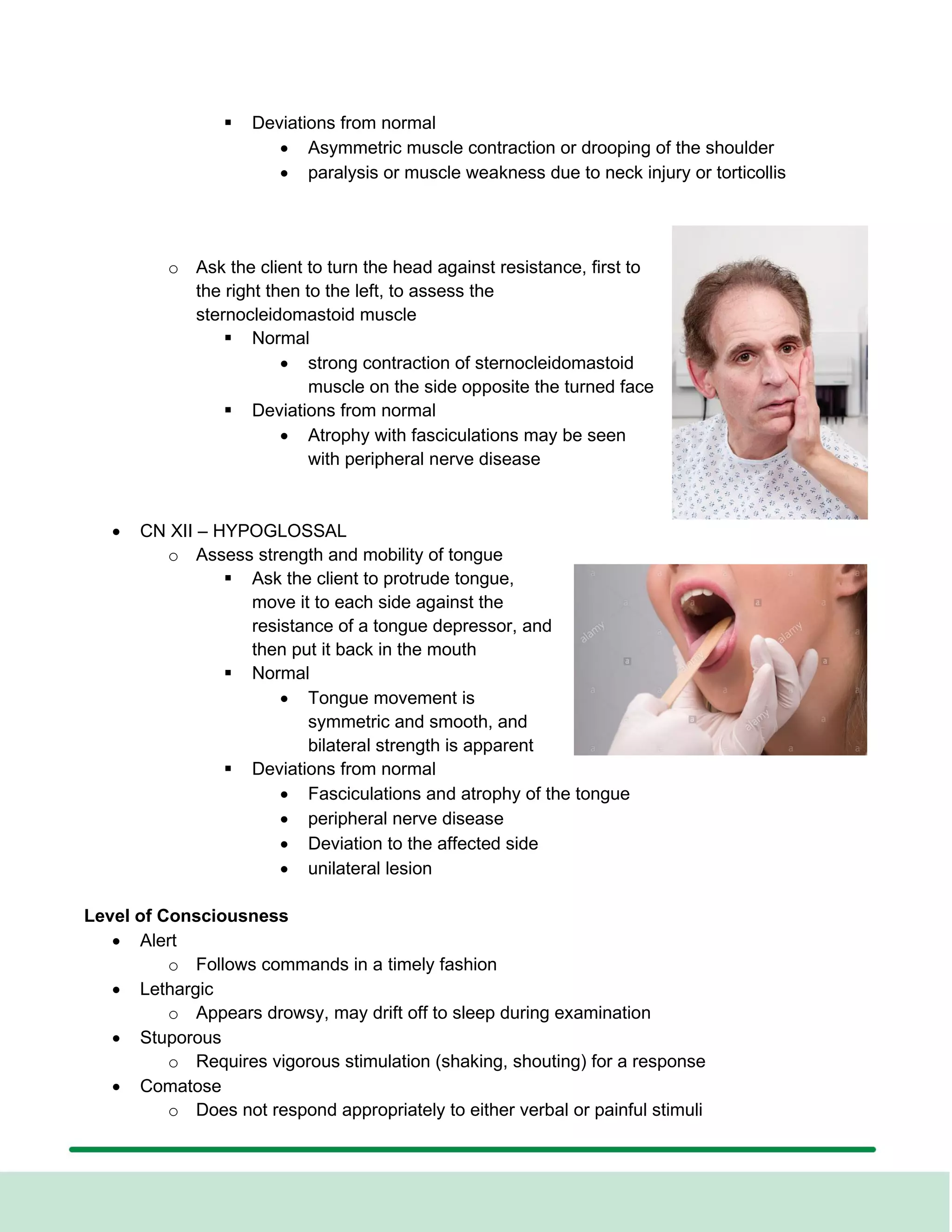
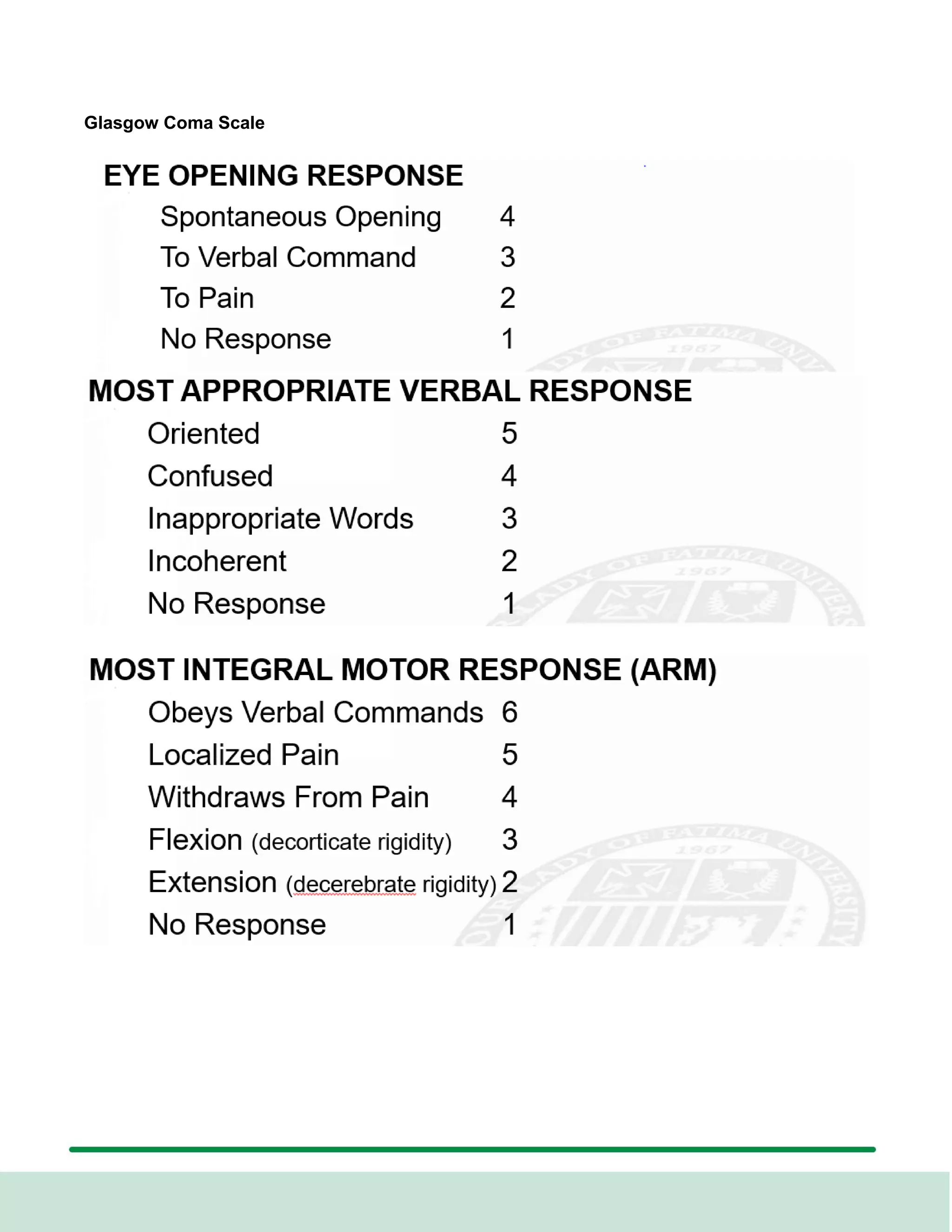
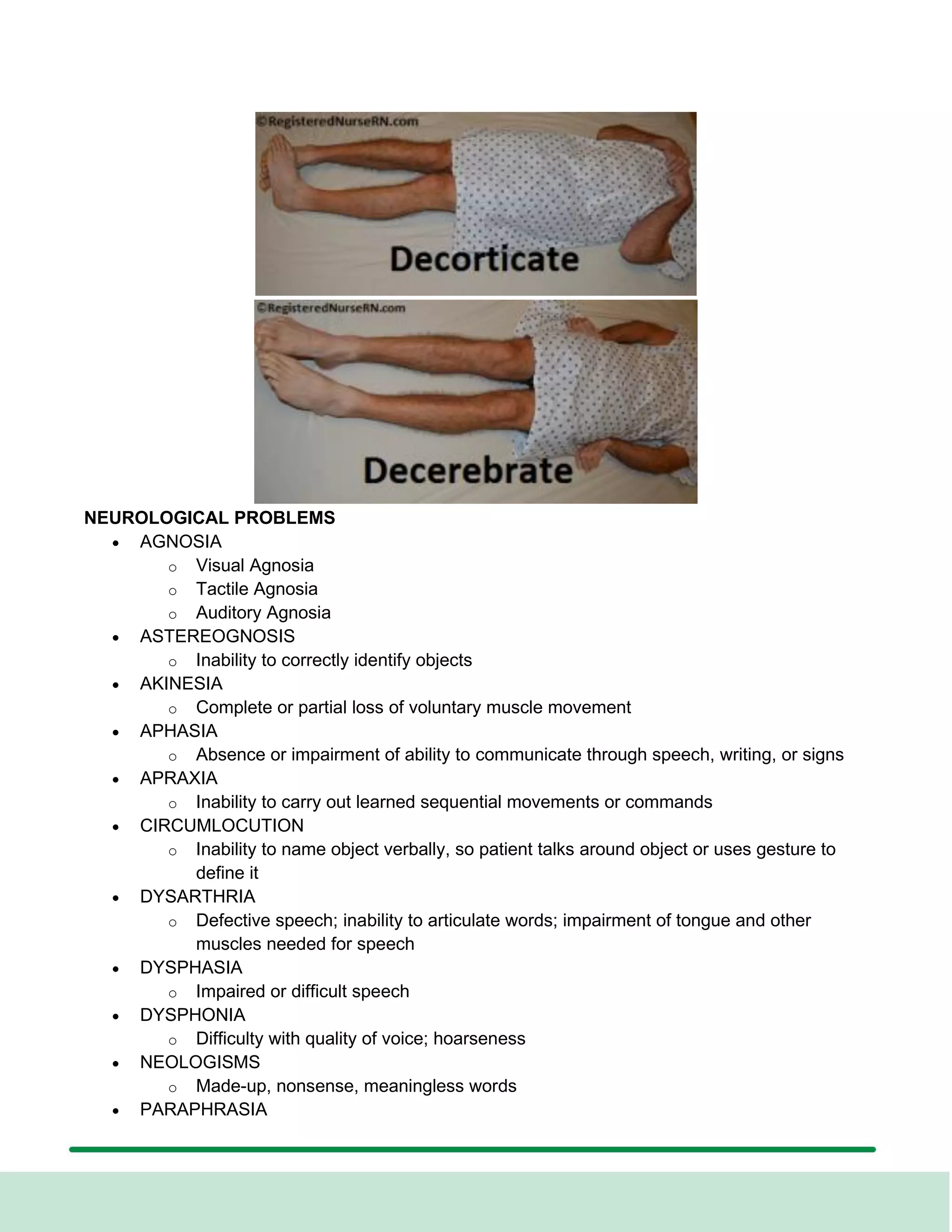
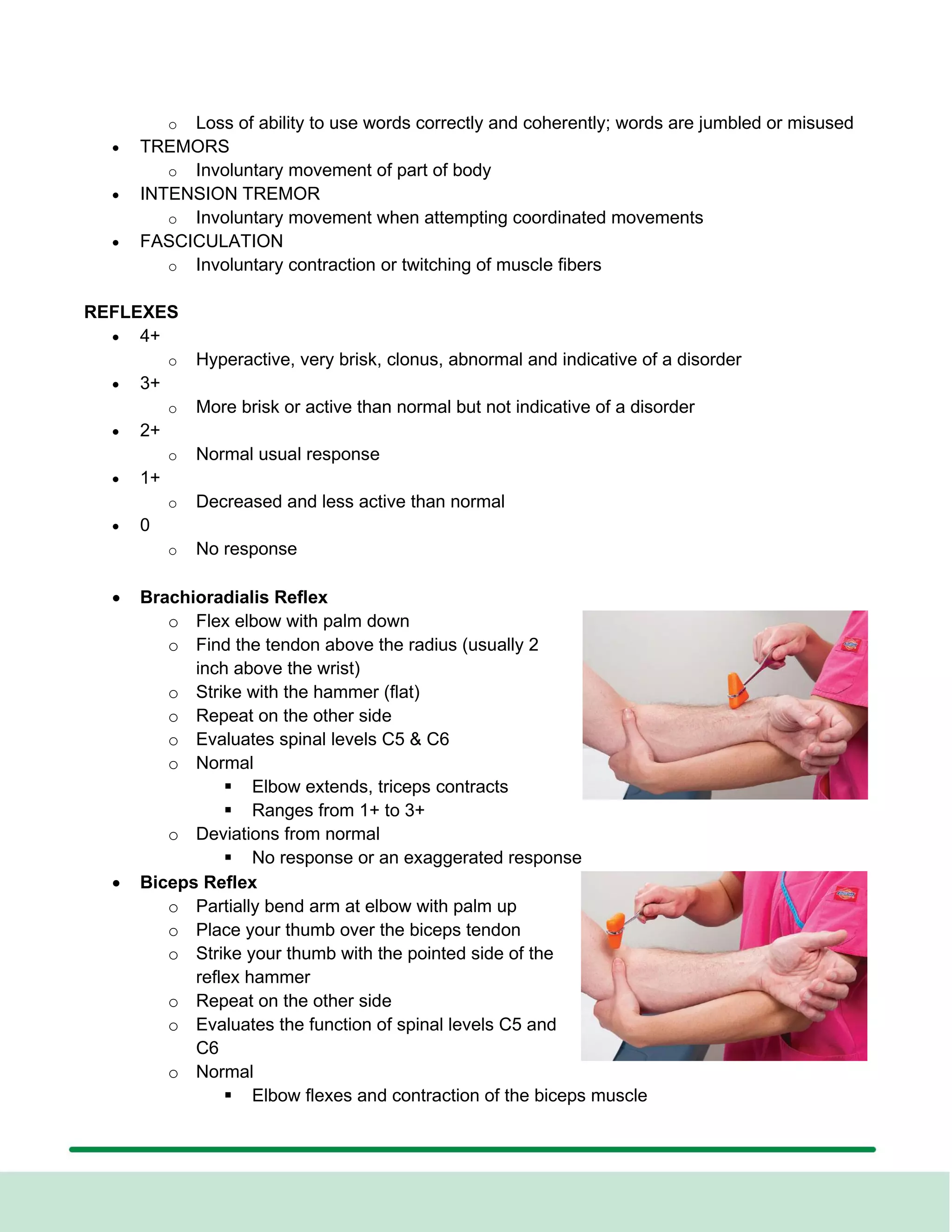
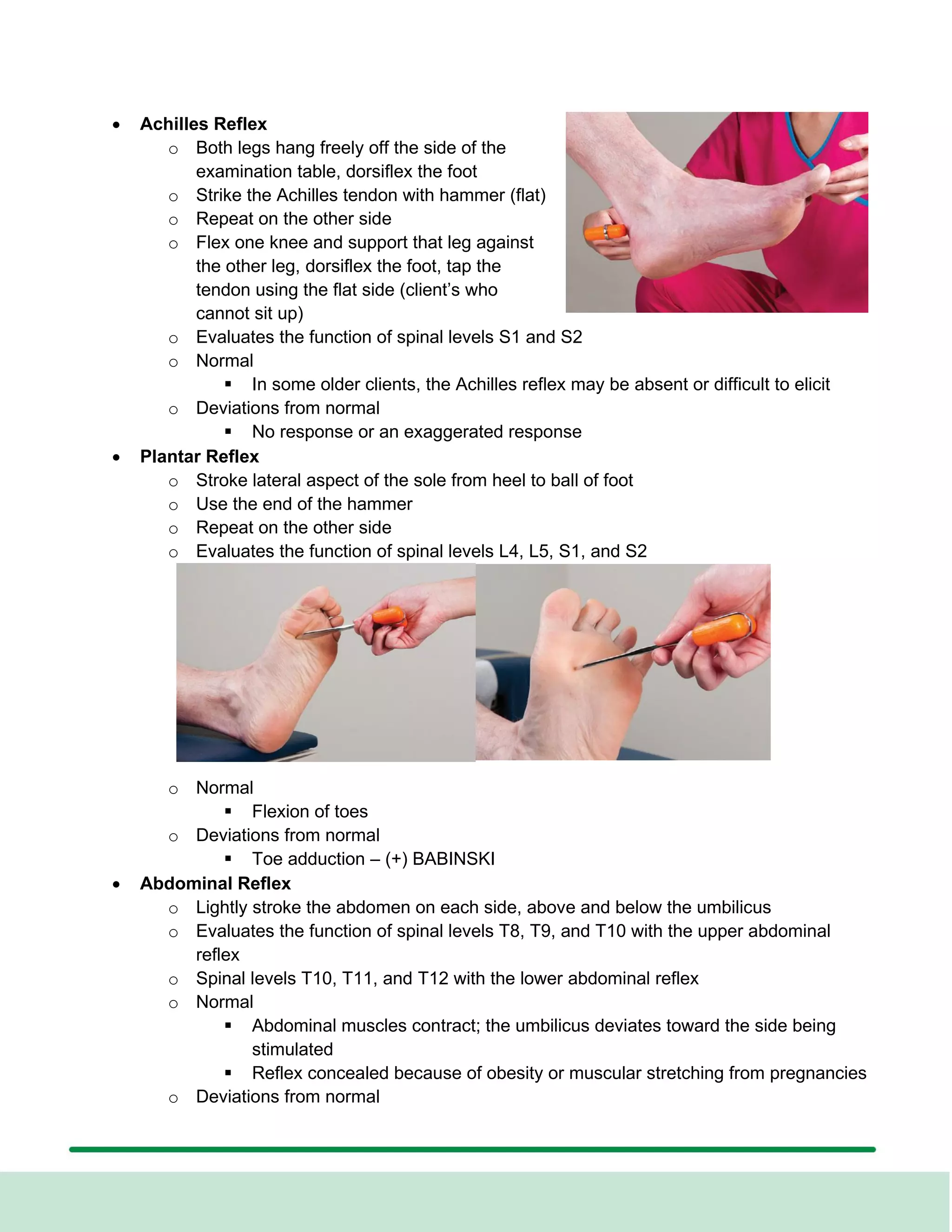
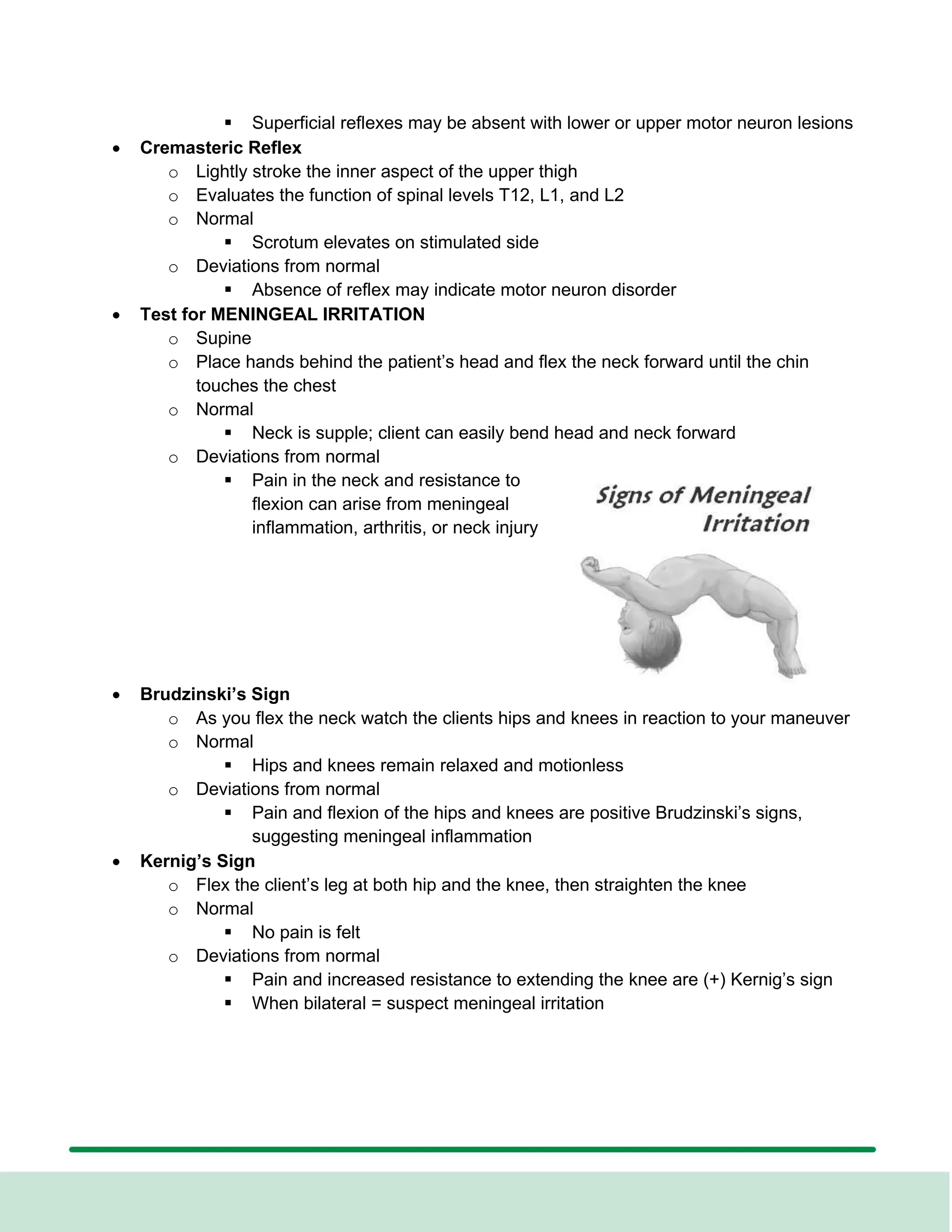
This document provides guidance for assessing the neurologic system as part of a physical examination for nursing students. It outlines the assessment of the 12 cranial nerves including their functions and tests to evaluate sensory and motor function. It also describes how to assess reflexes, level of consciousness, and other aspects of the neurologic exam such as problems to check for. The goal is for students to learn to differentiate normal from abnormal neurologic findings.