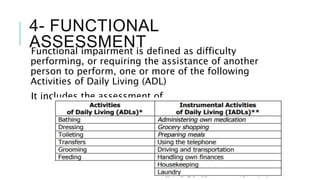
Geriatric assessment is a multidimensional evaluation of elderly patients that includes medical history, physical exam, and assessment of functional abilities. The assessment evaluates patients' physical and cognitive functioning, social support systems, nutritional status, and risk of functional impairment requiring assistance with activities of daily living. A comprehensive geriatric assessment provides a holistic view of elderly patients to develop appropriate care plans.