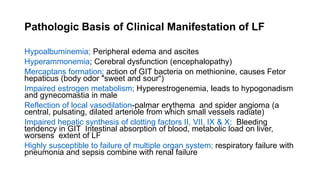
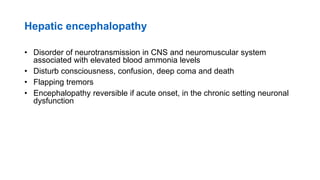
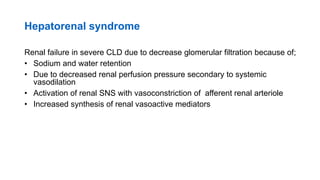
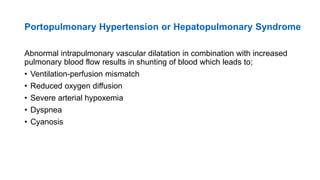
This document provides an overview of liver failure, including its causes, types, and pathophysiology. It discusses the major causes of acute and chronic liver failure. Acute liver failure can result from drug or toxin damage, viral hepatitis, or the end stage of chronic liver disease leading to cirrhosis. Chronic liver failure is usually the end result of chronic hepatitis or liver disease progressing to cirrhosis. The document describes the pathophysiology behind several clinical manifestations of liver failure, including hepatic encephalopathy, hepatorenal syndrome, and hepatopulmonary syndrome. It also discusses the mechanisms leading to ascites in liver failure patients.