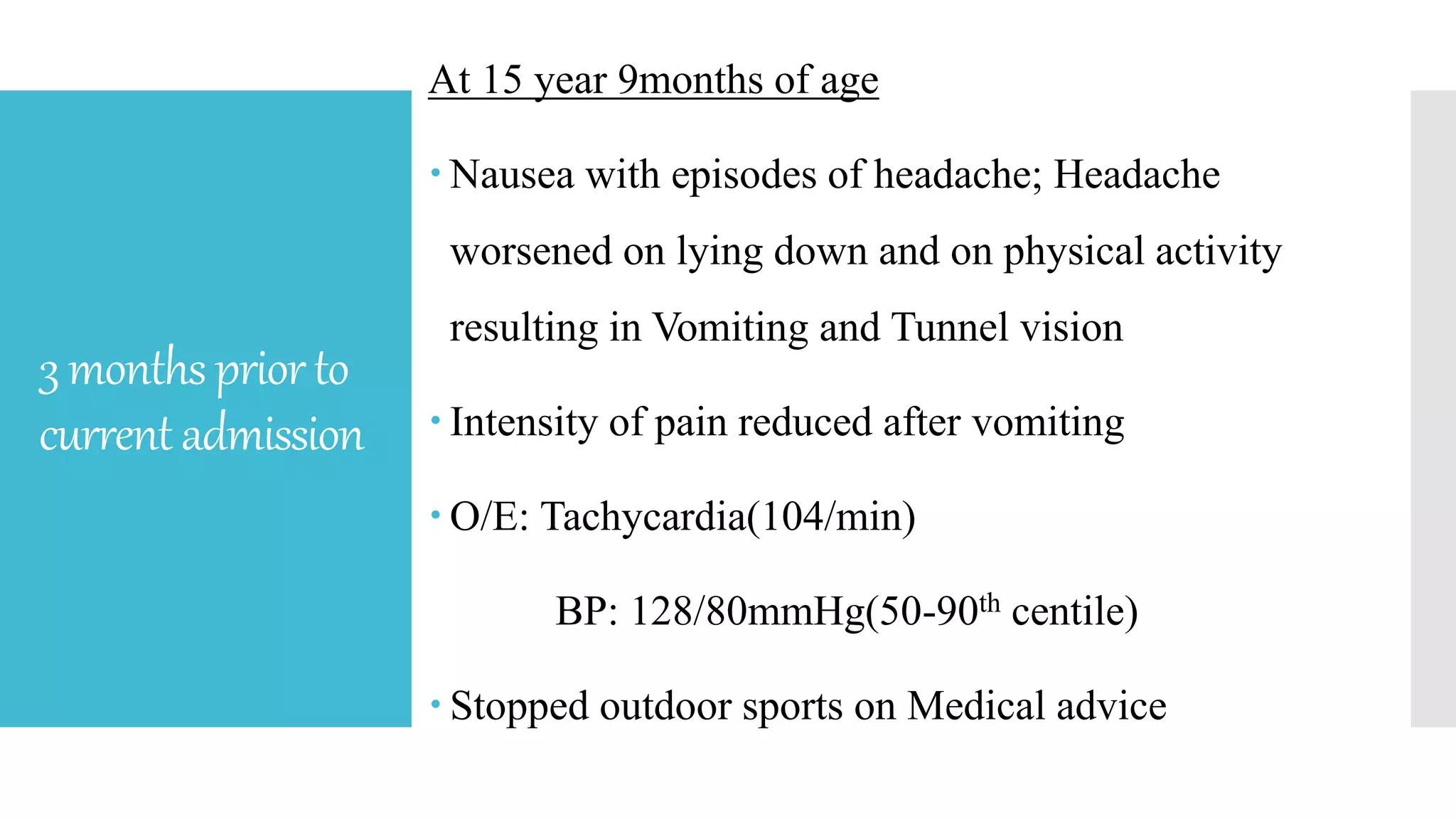
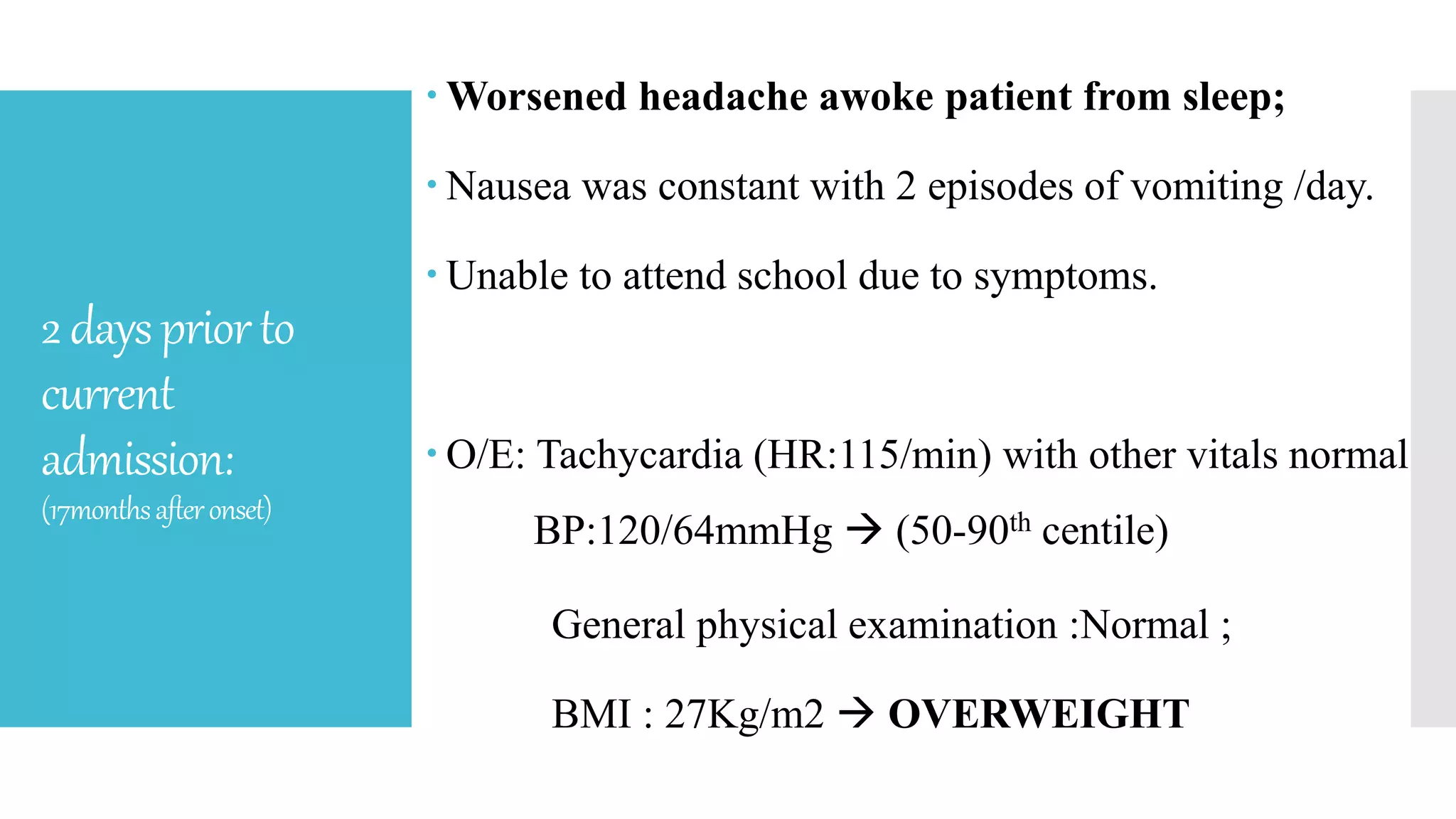
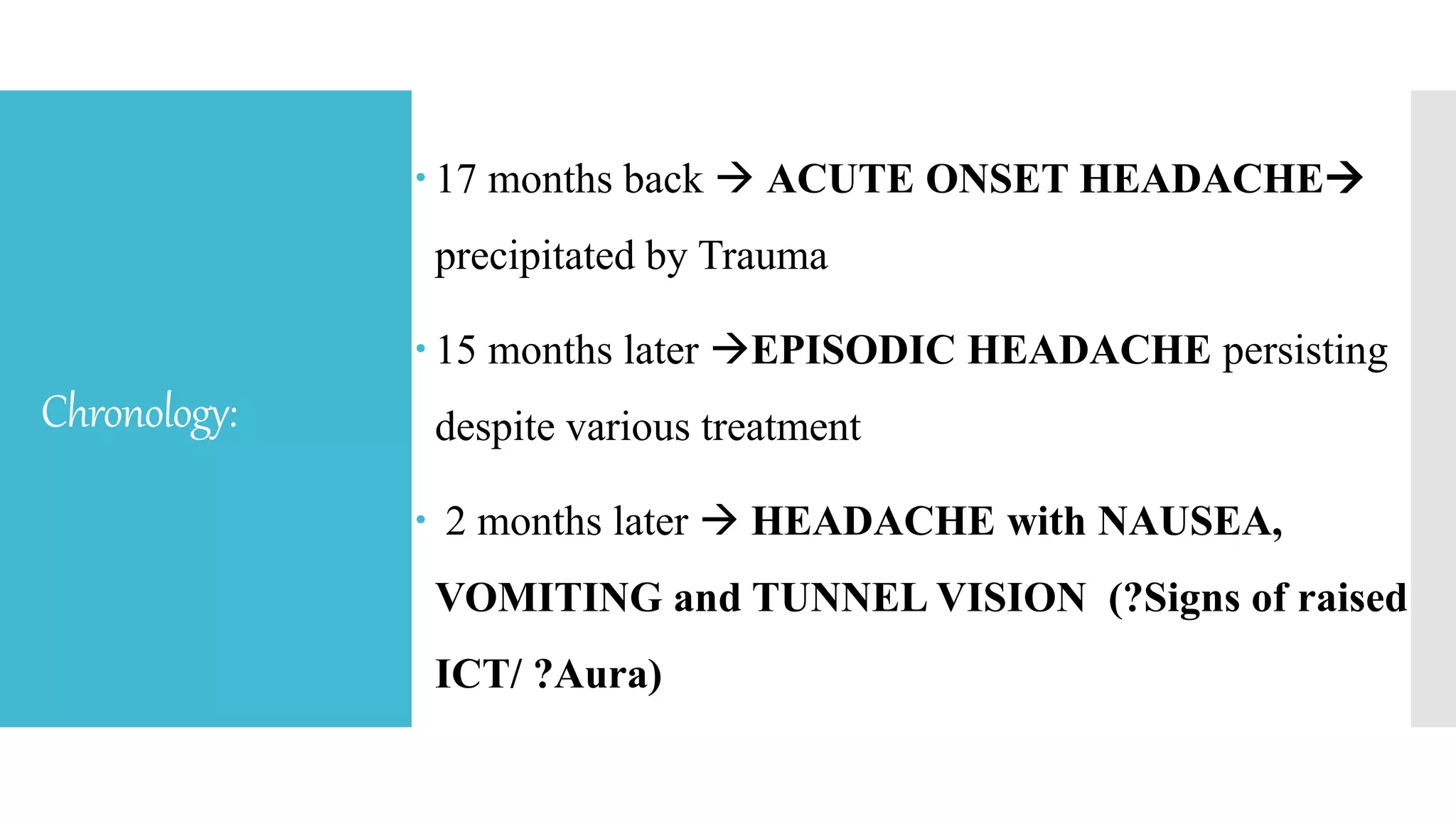
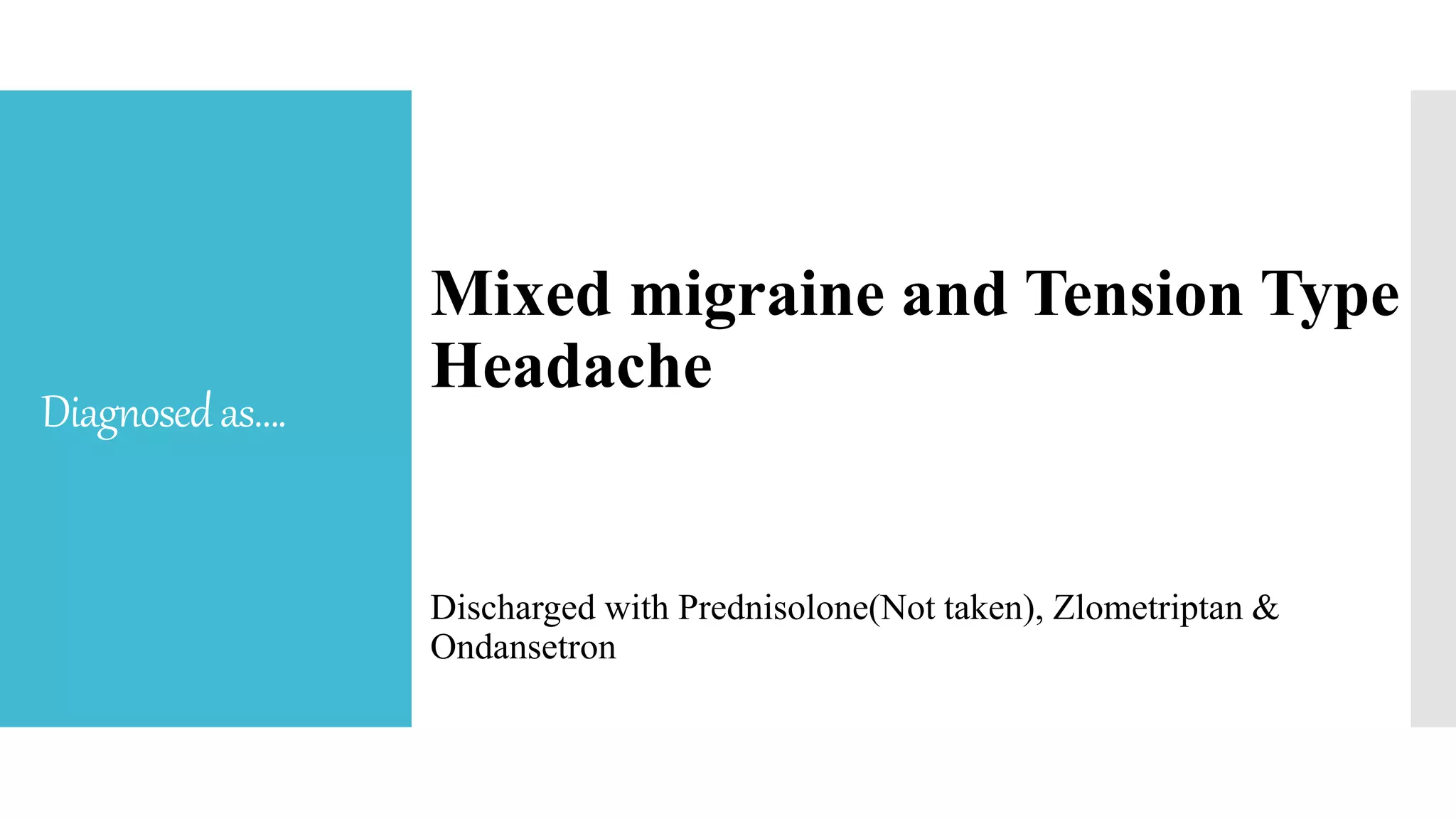
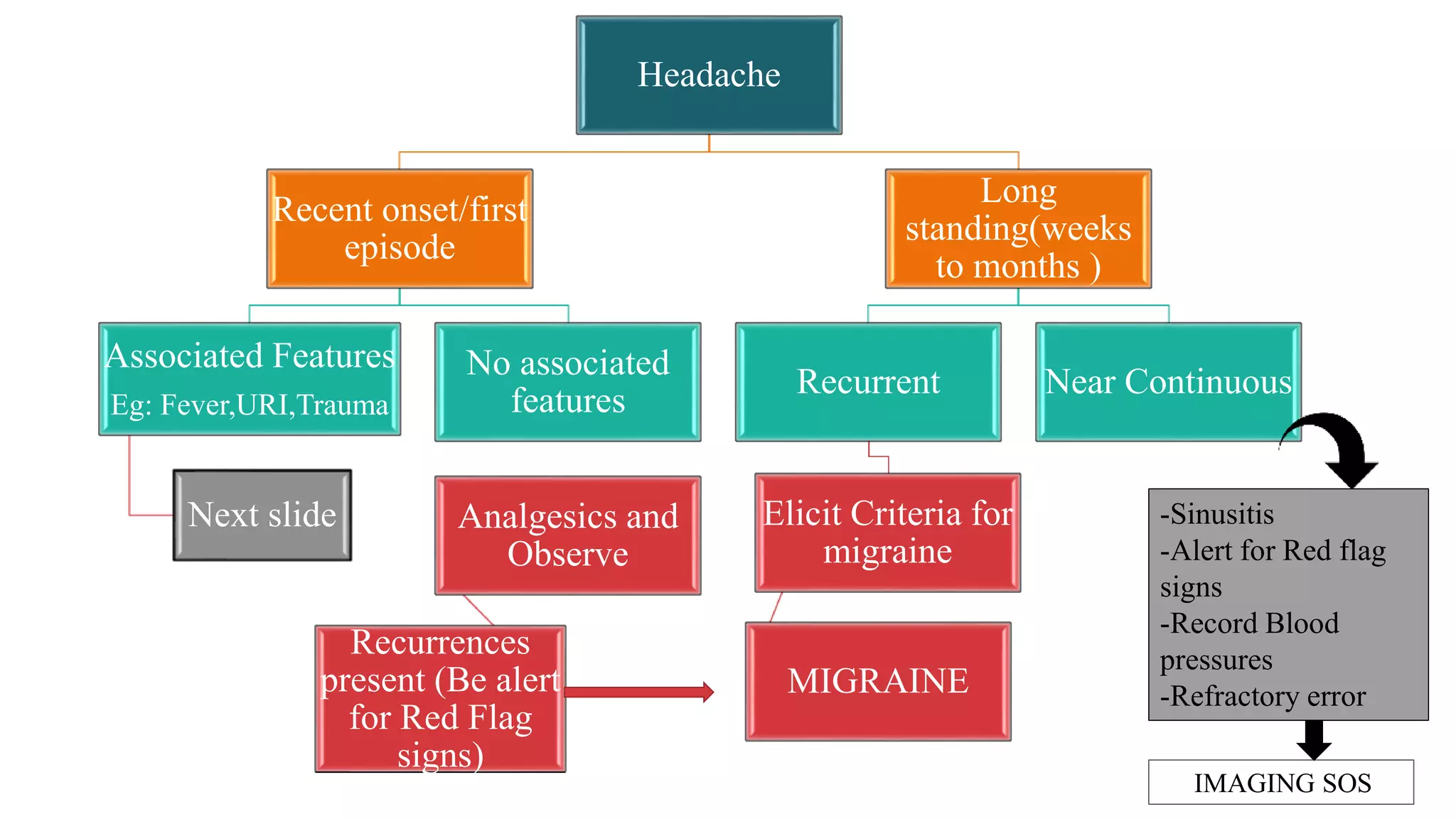
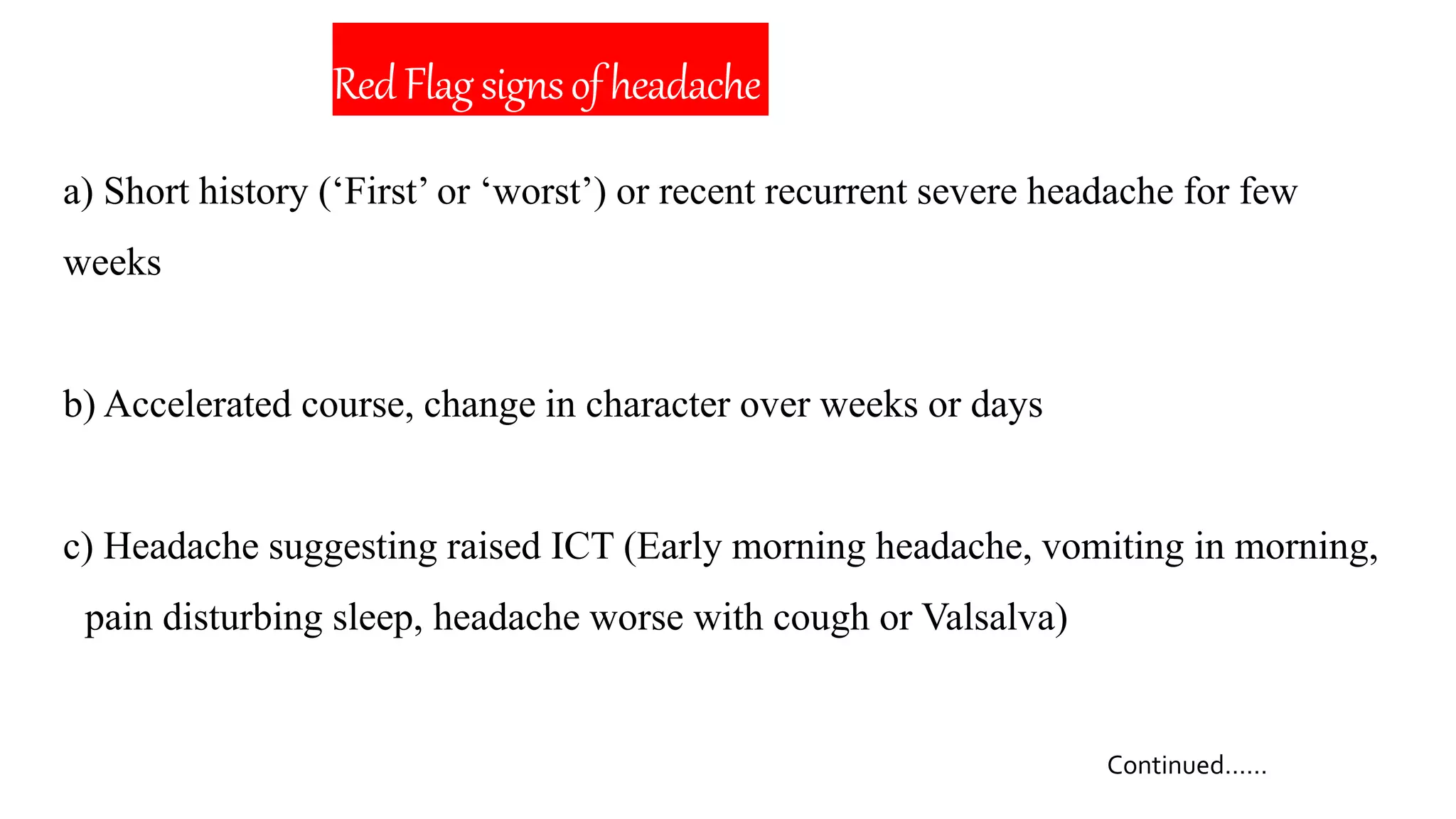
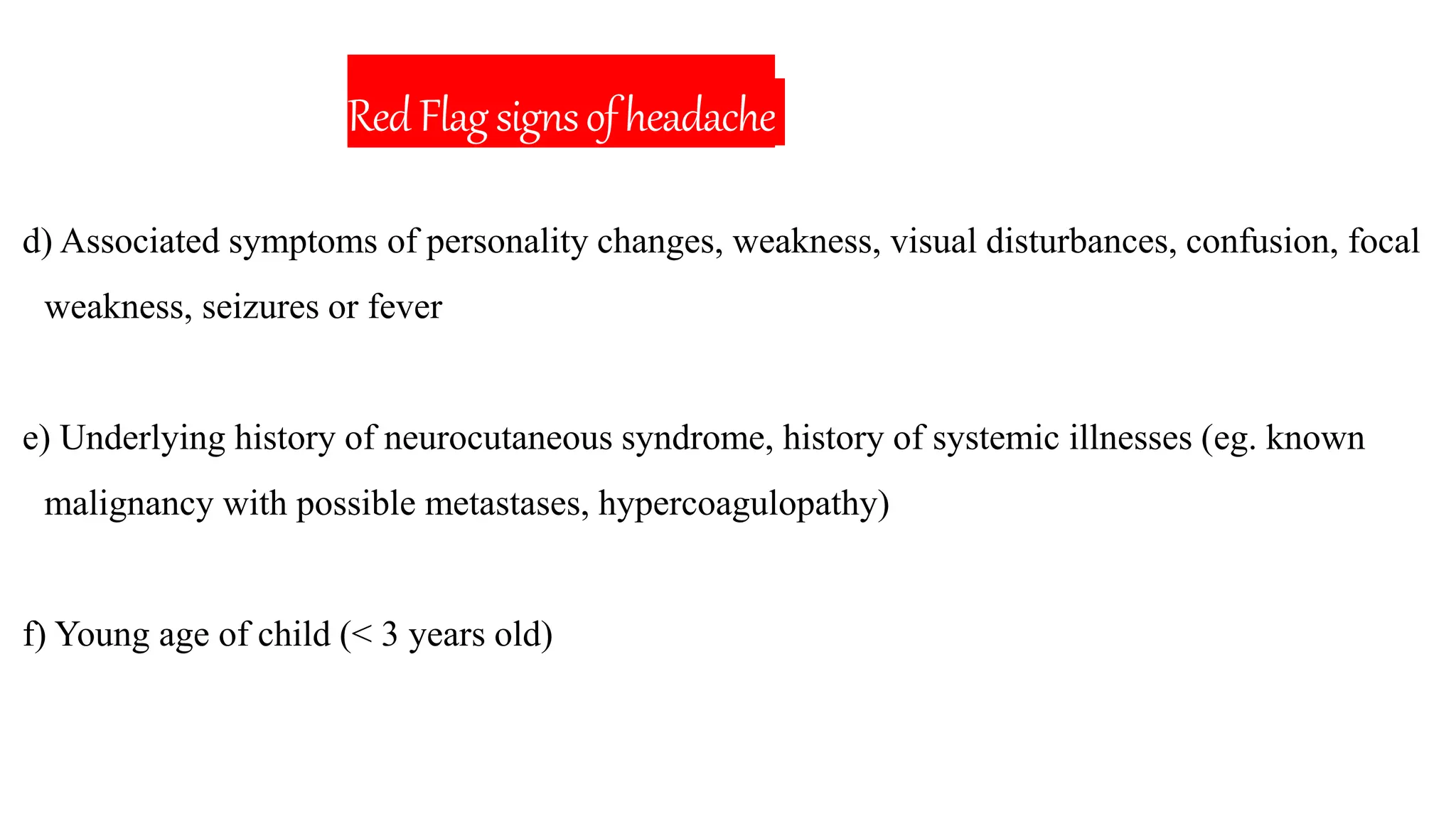
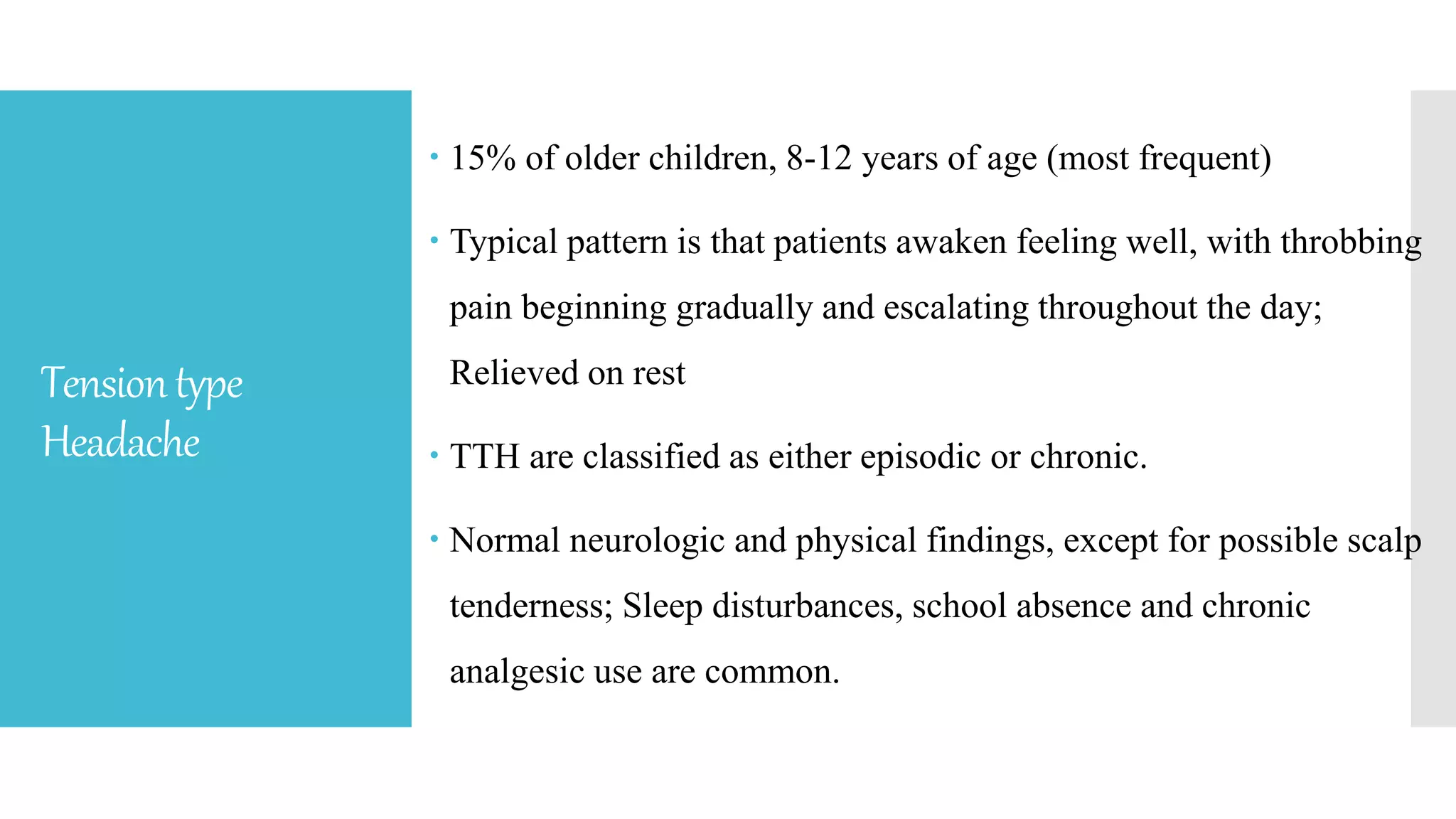
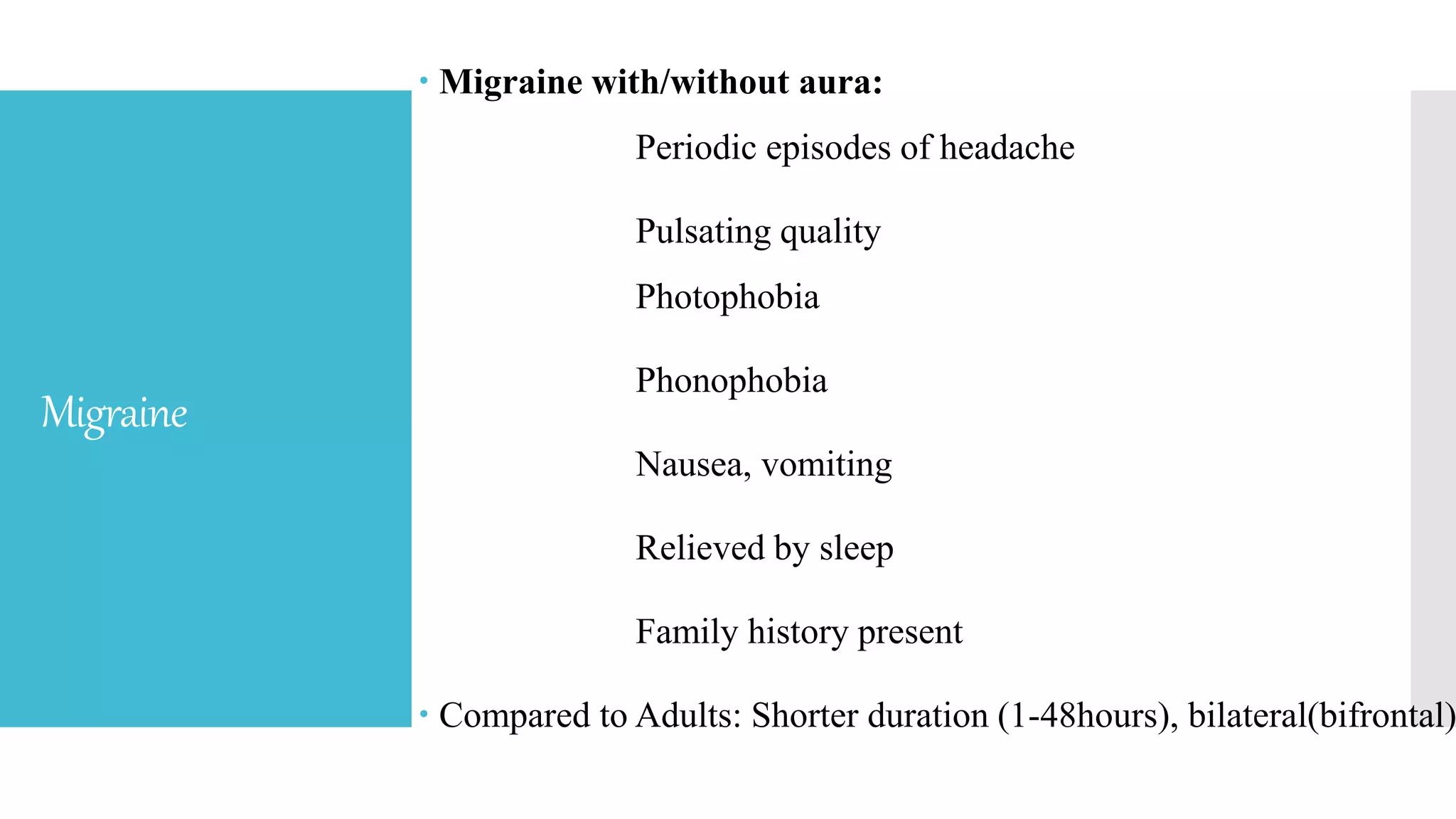
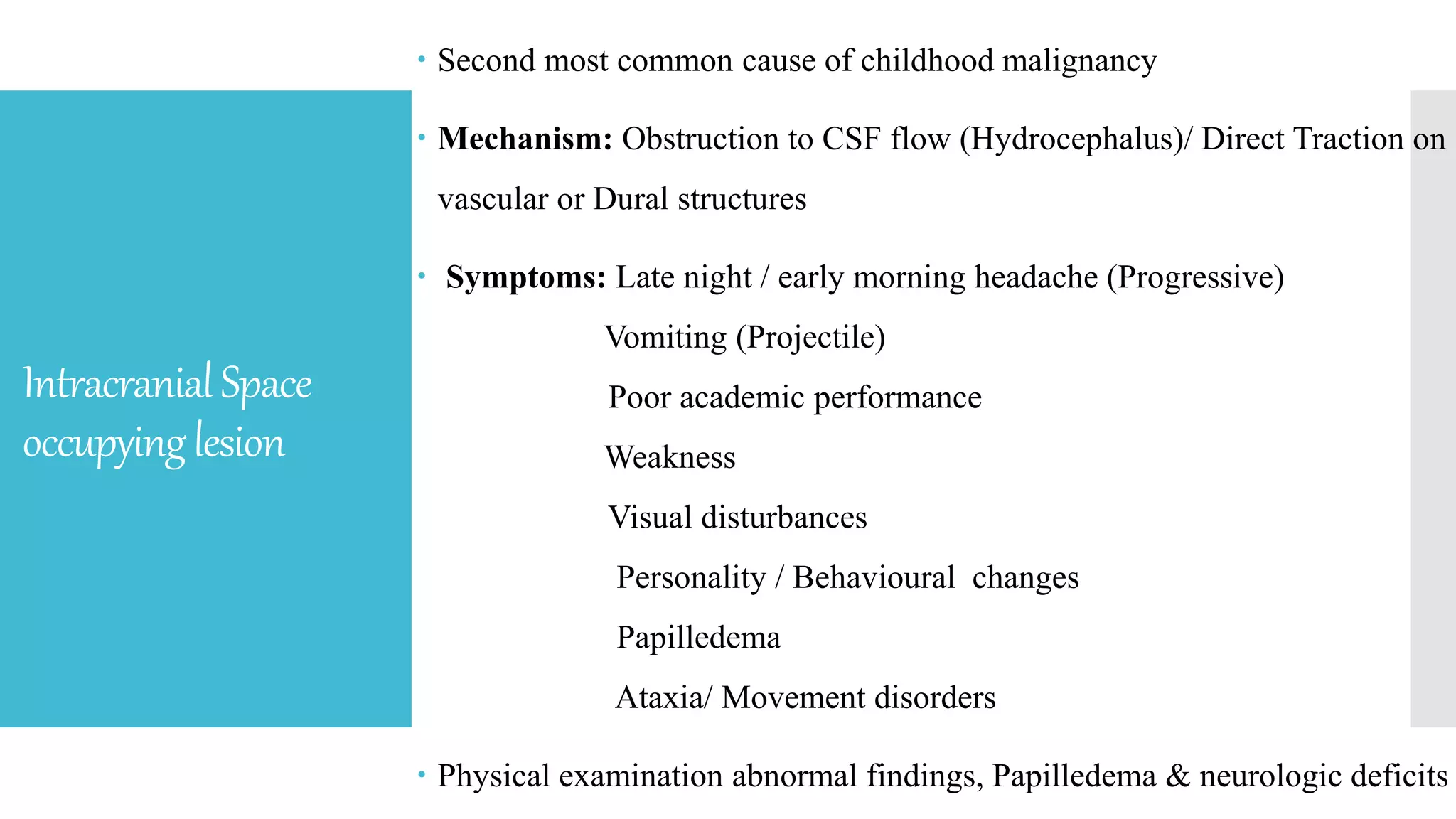
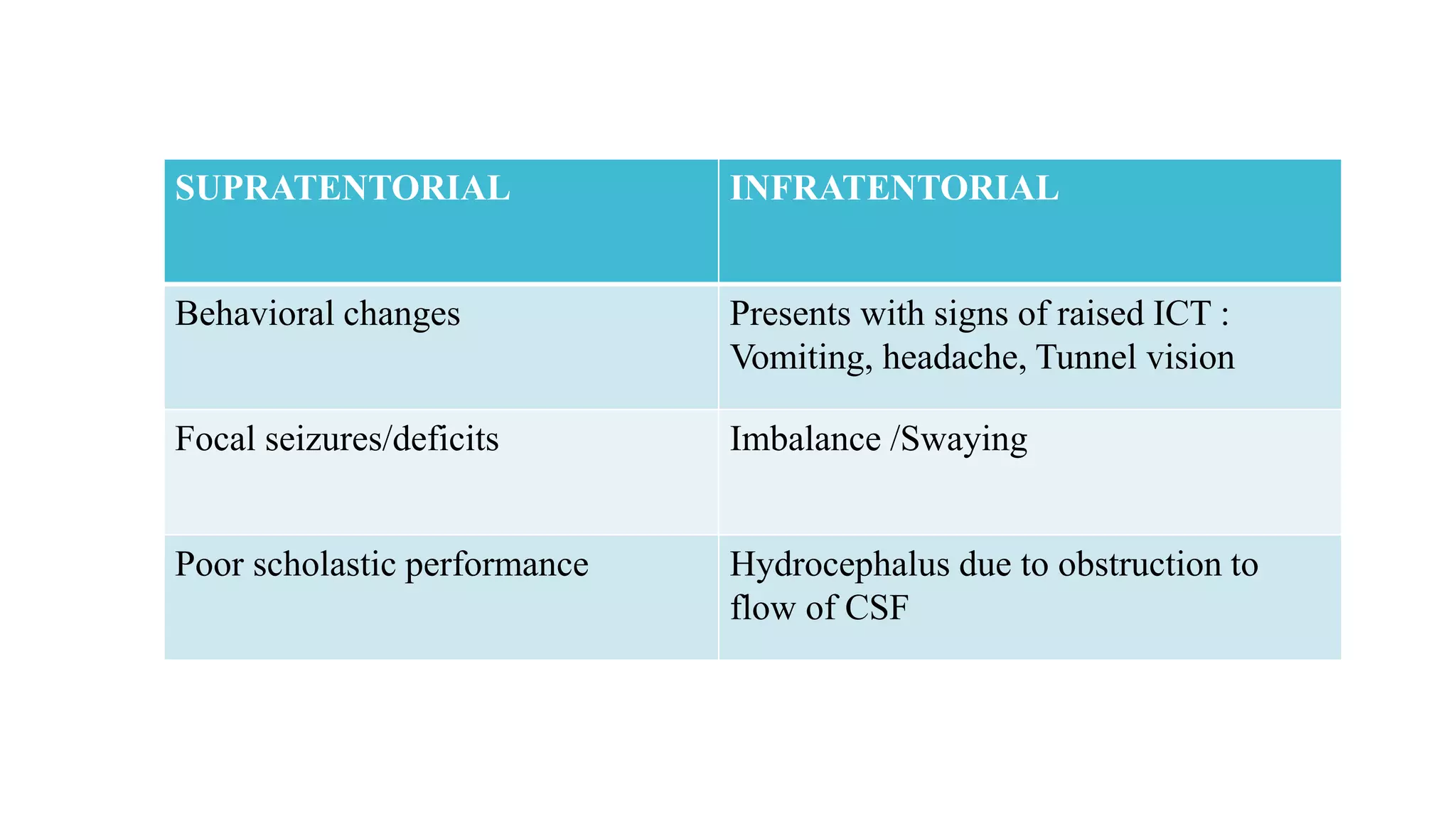
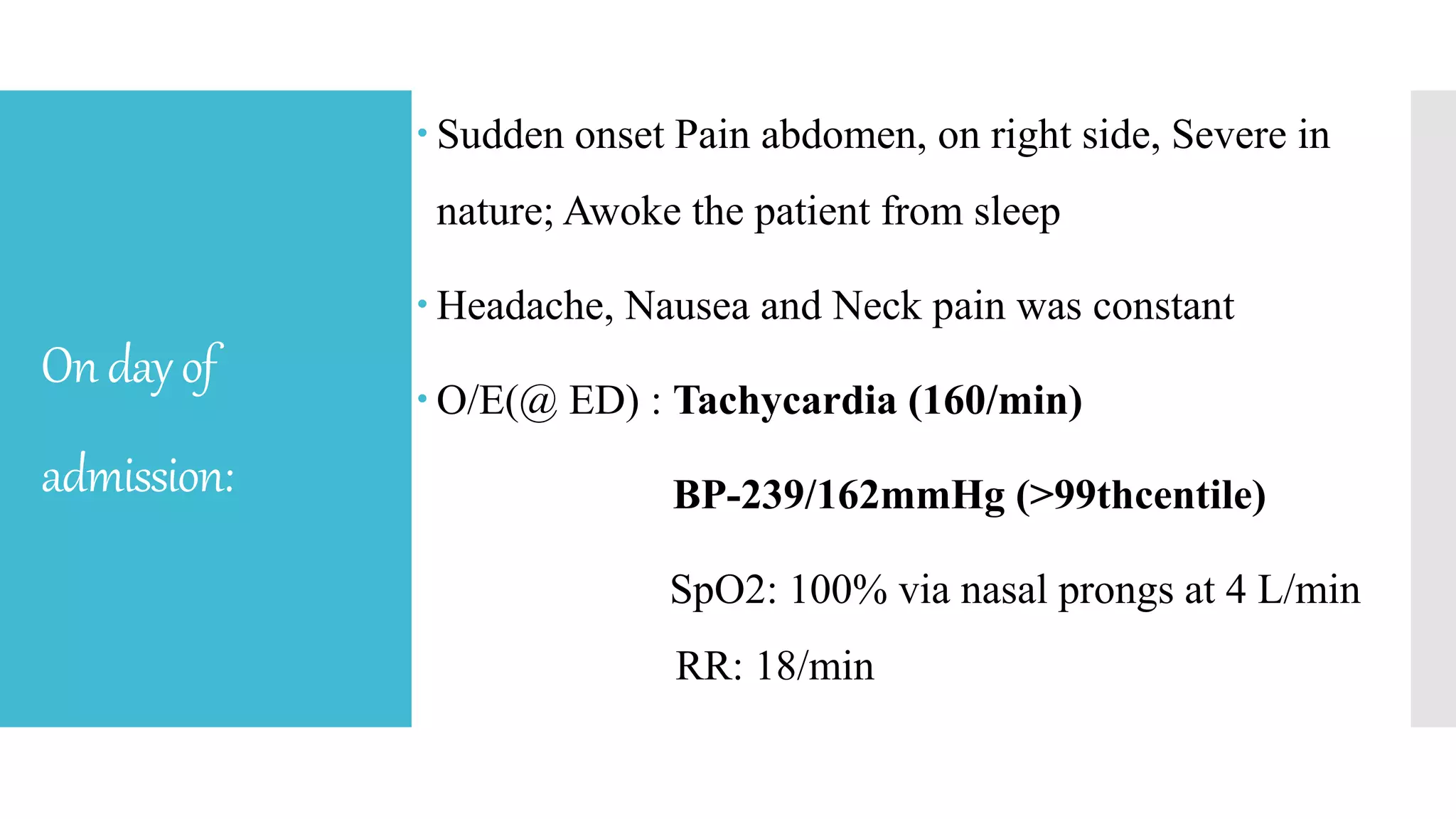
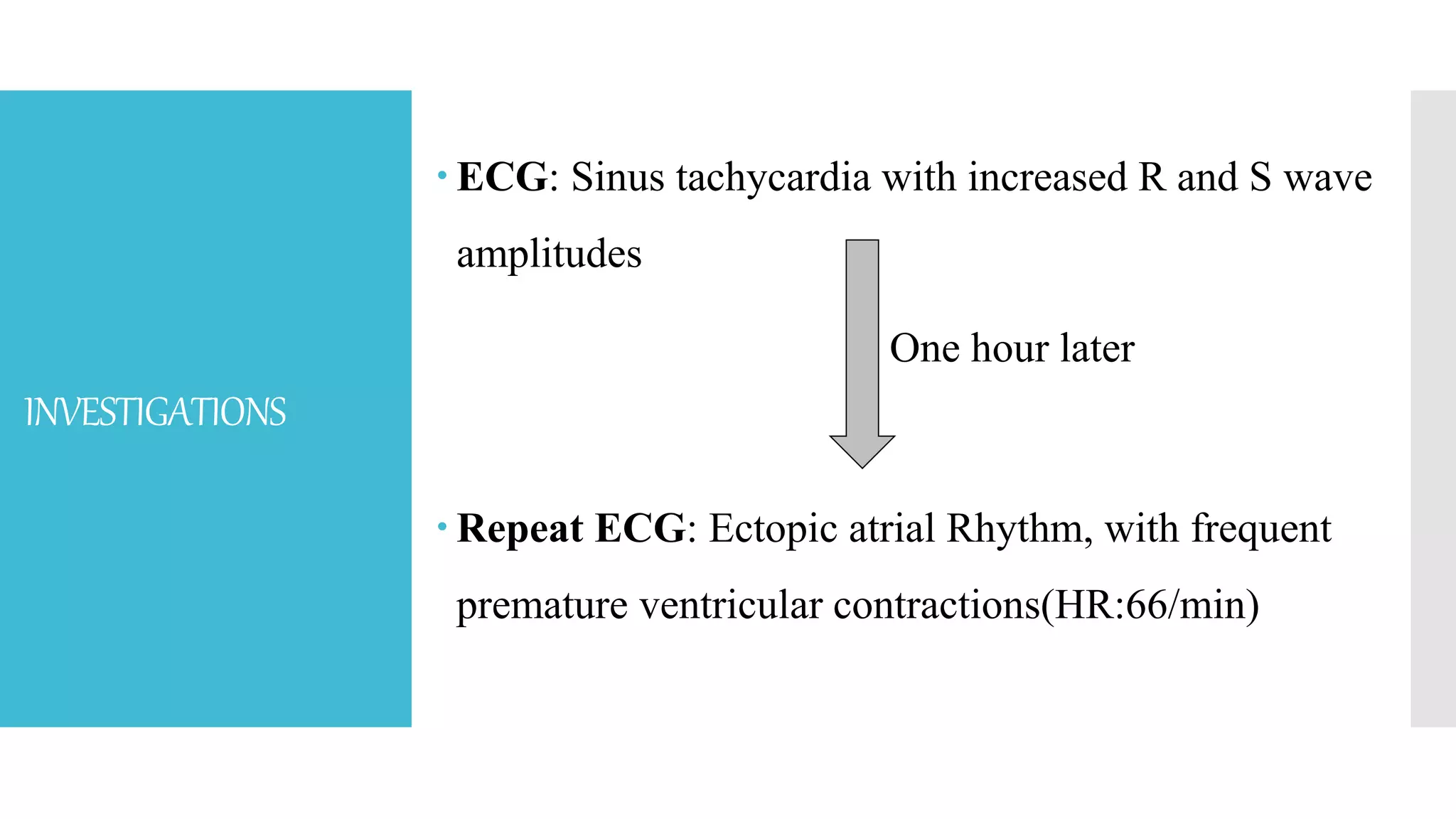
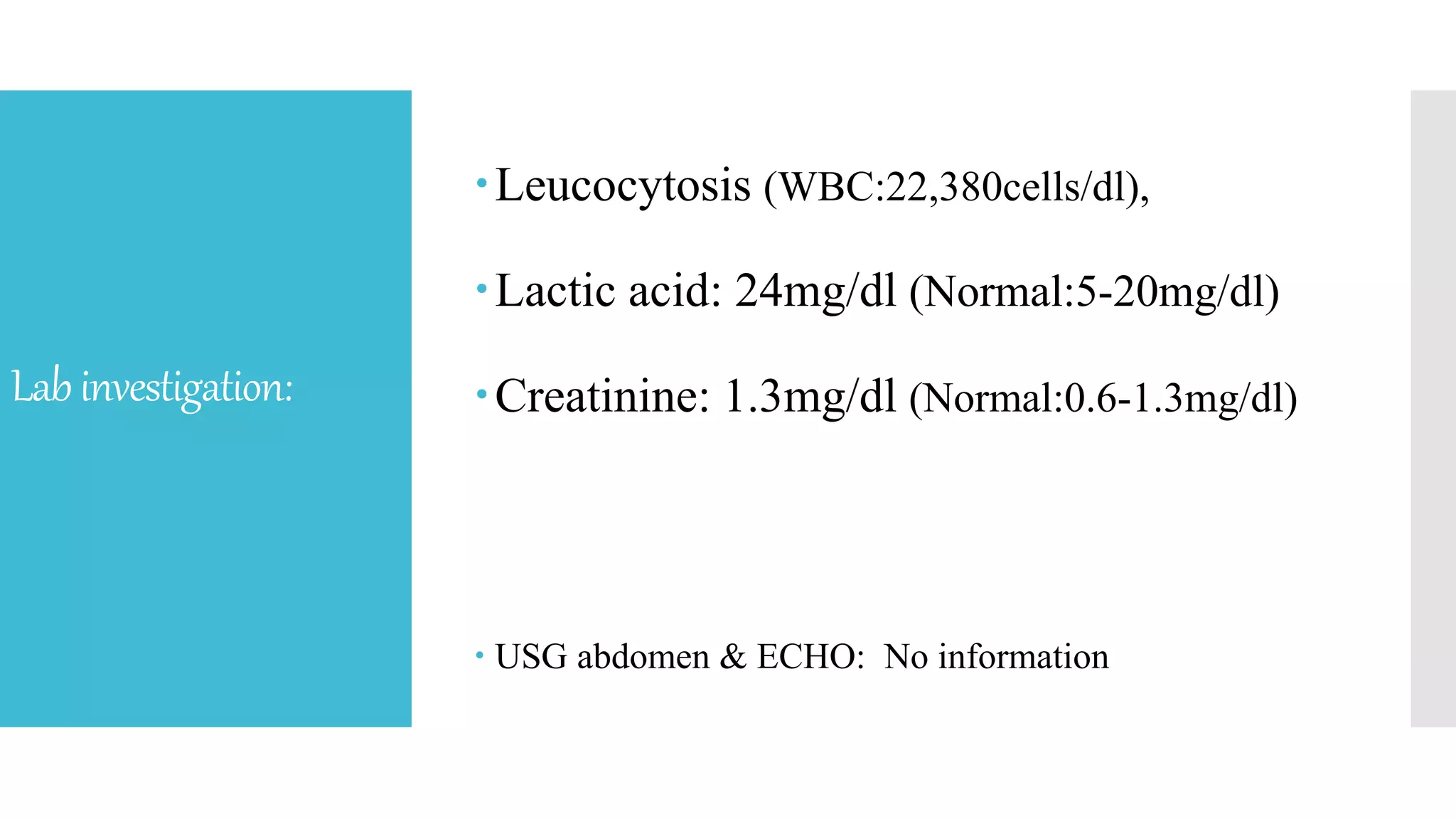
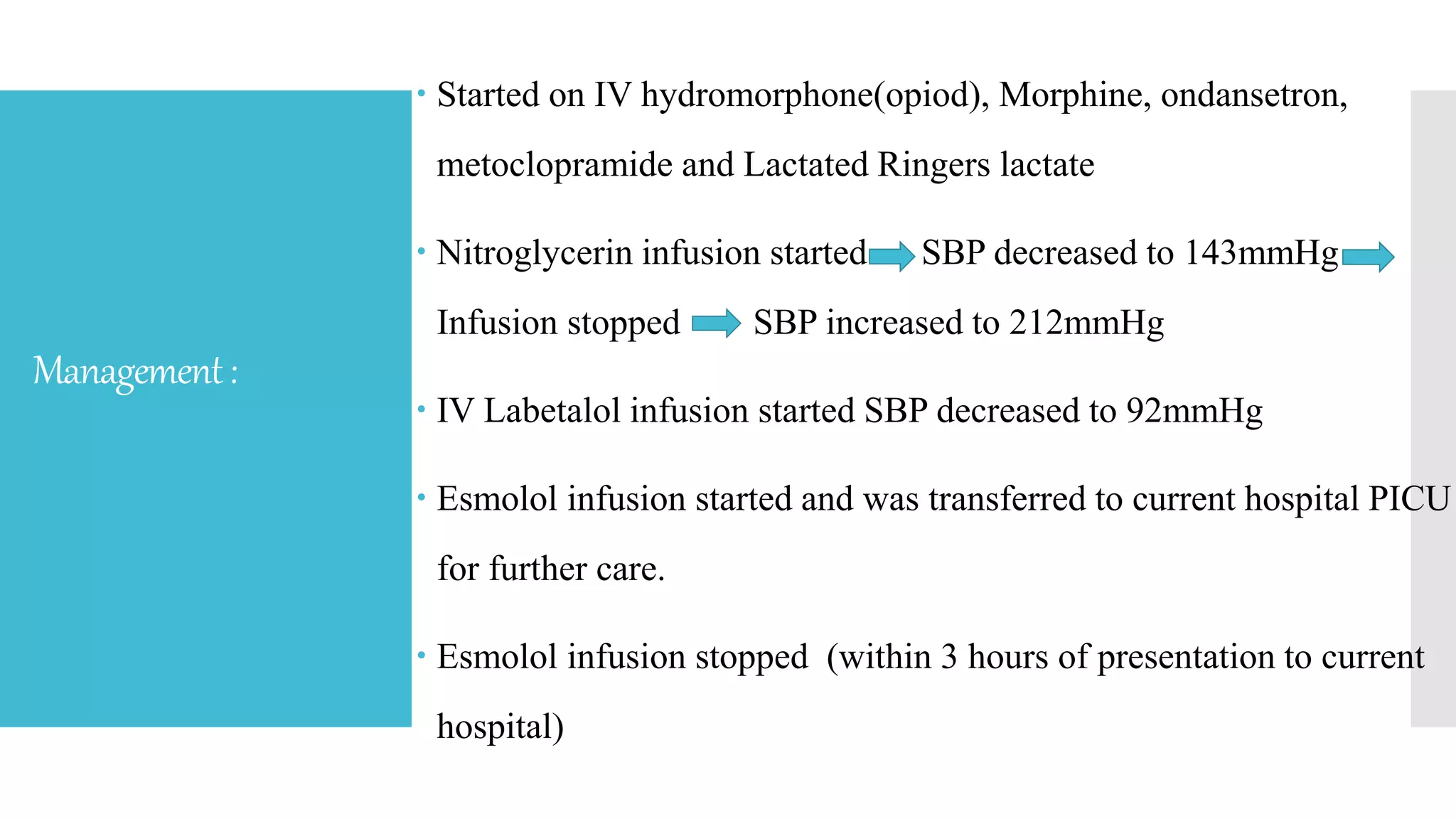
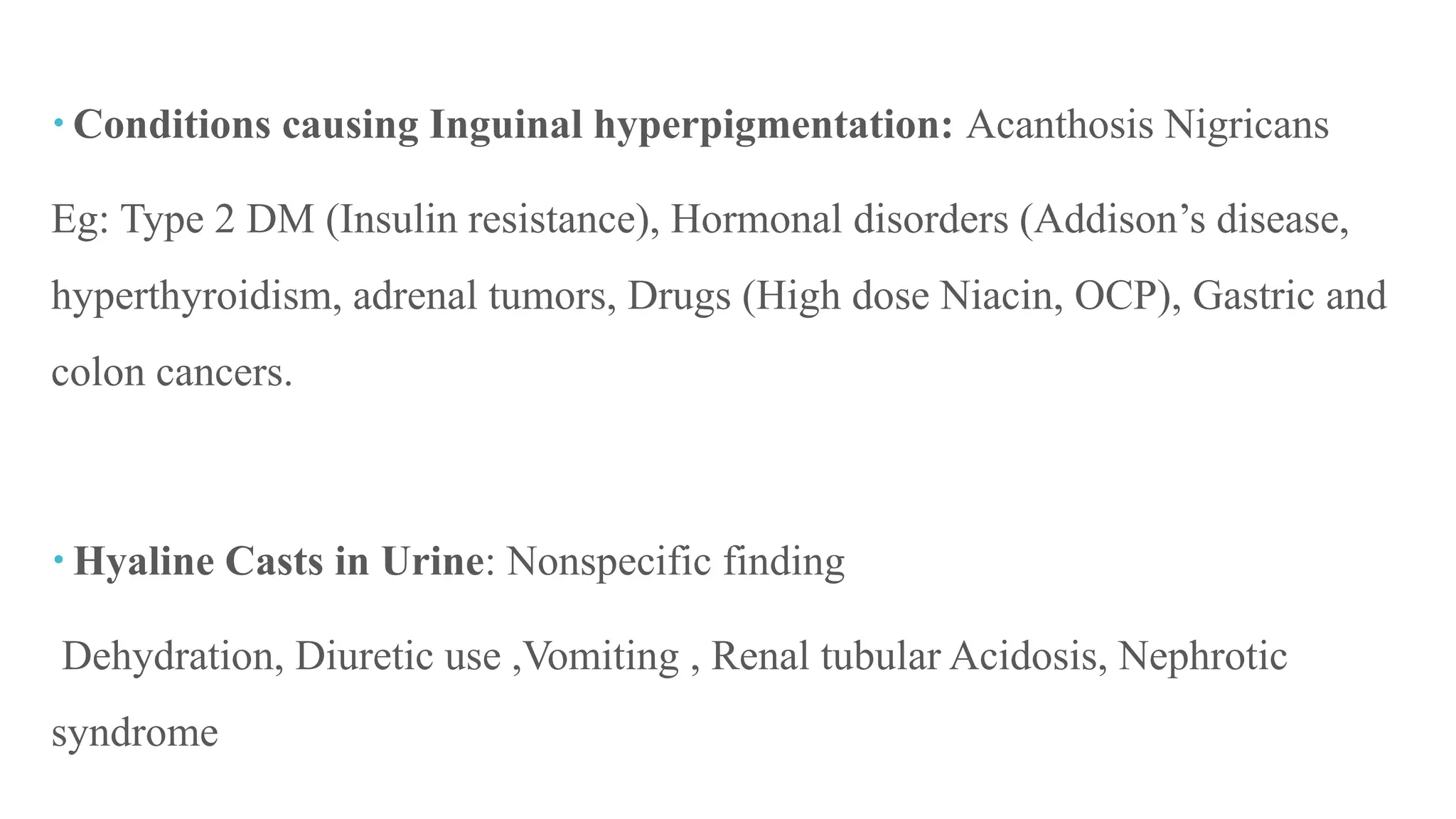
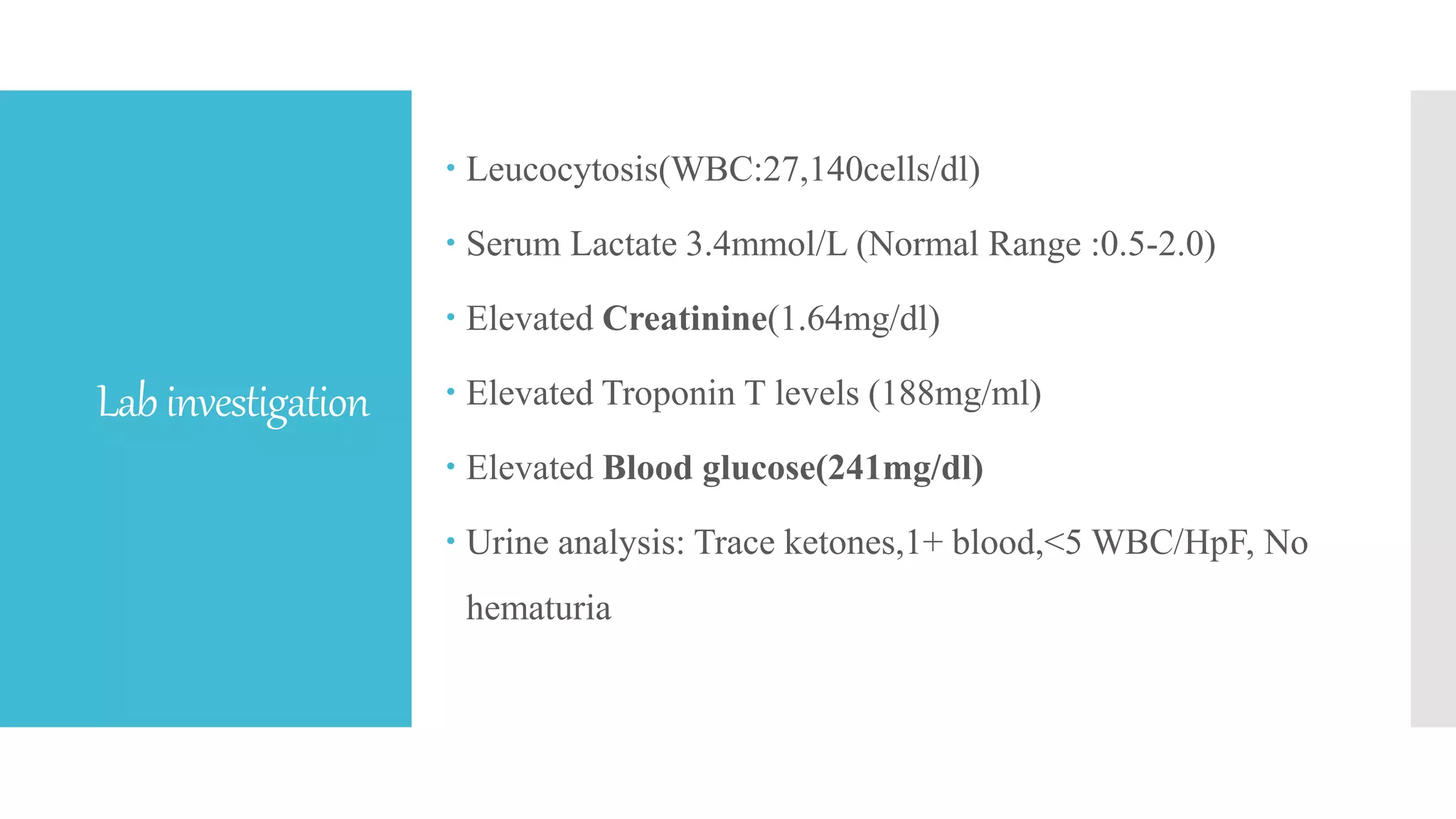
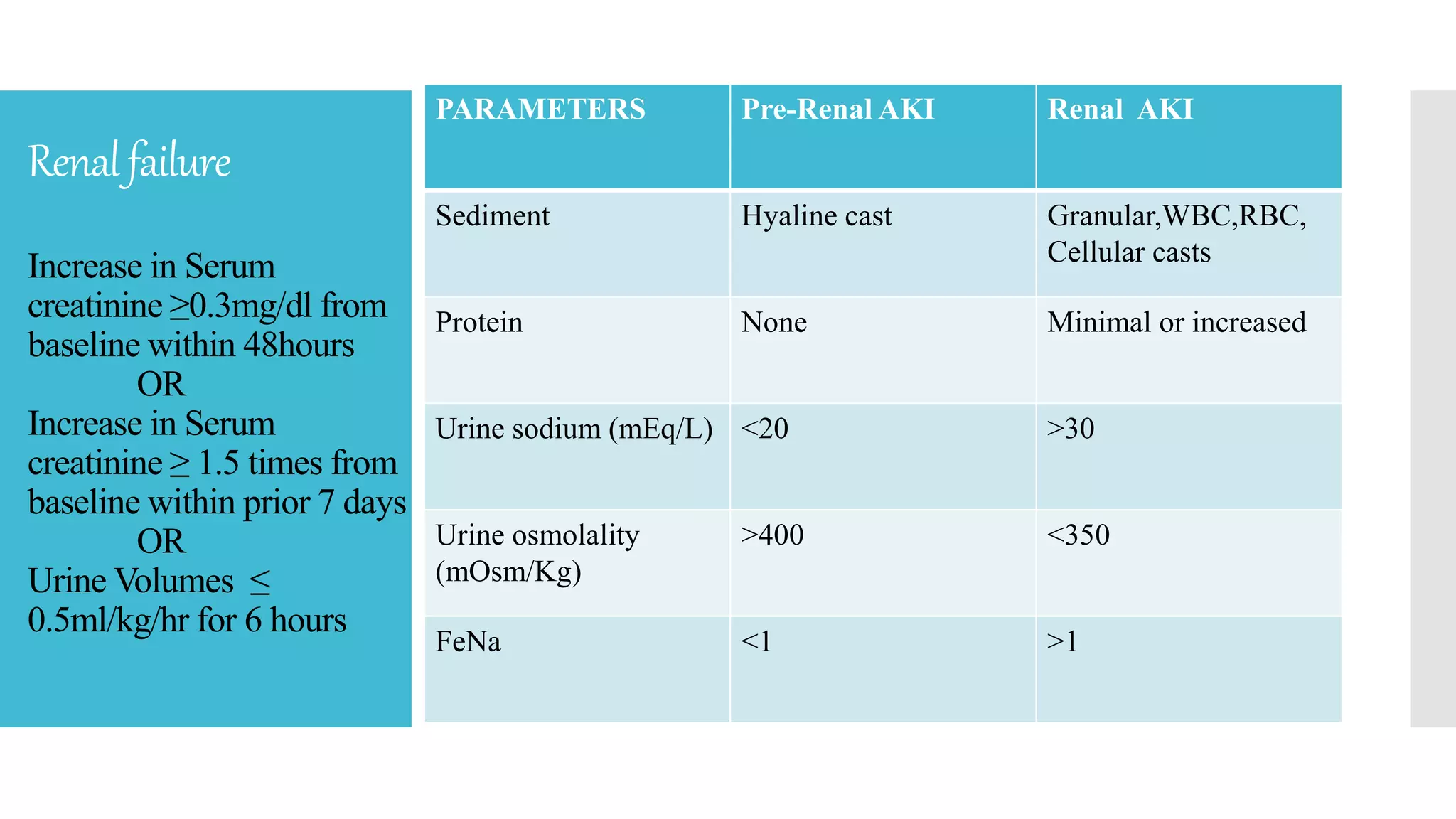
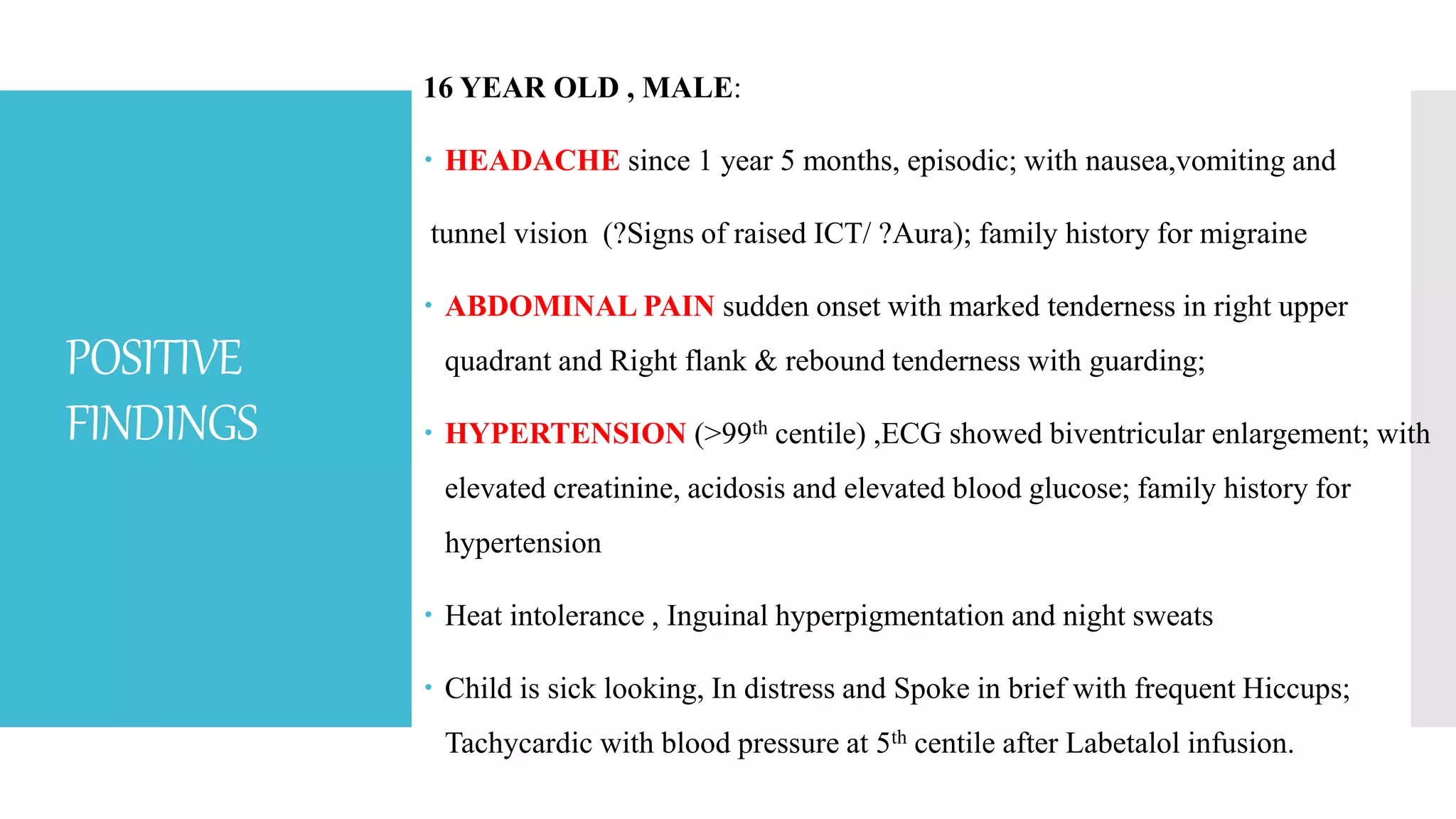
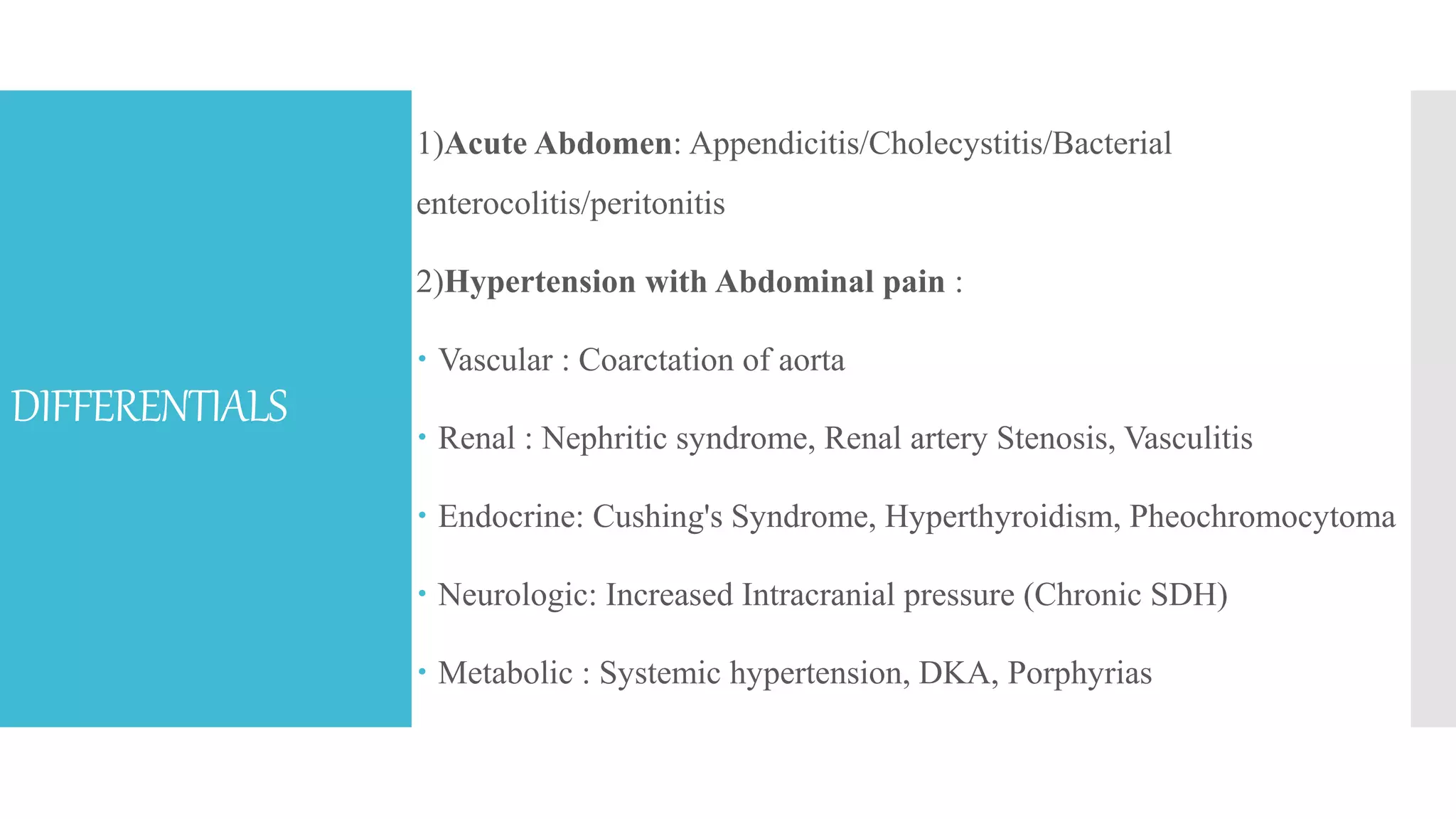
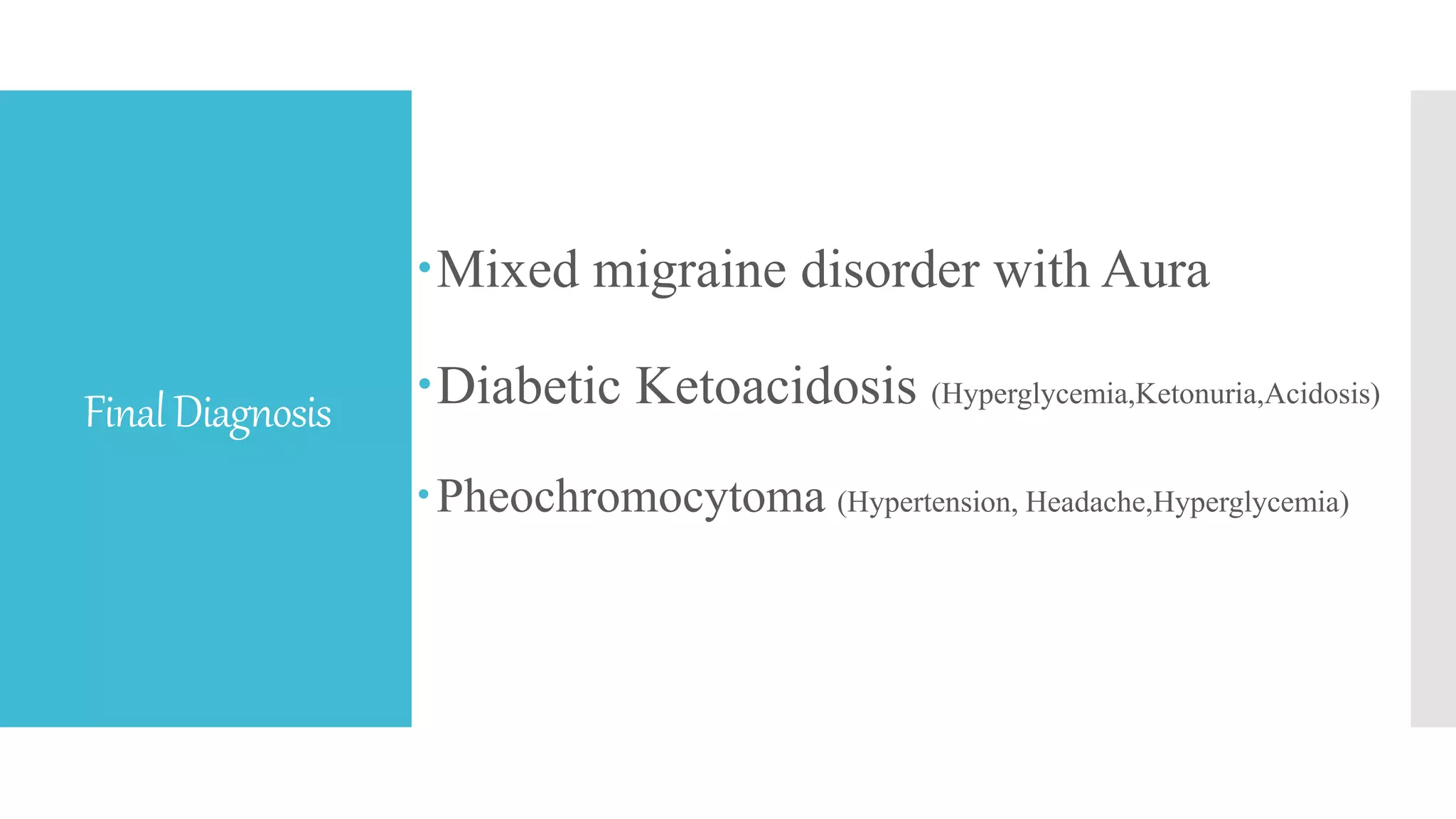
This case discusses a 16-year-old male who presented with worsening headache, abdominal pain, and elevated blood pressure. He had a history of headaches for over a year since a motor vehicle accident, which had been treated unsuccessfully. On admission, he was hypertensive to dangerous levels and found to have leukocytosis, lactic acidosis, elevated troponin, and renal failure. Further evaluation revealed inguinal hyperpigmentation and right upper quadrant tenderness.