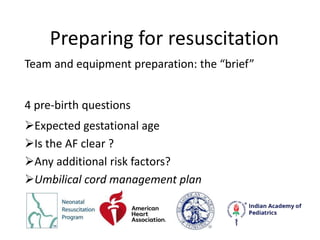
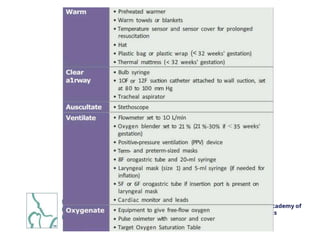
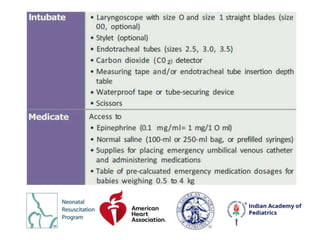
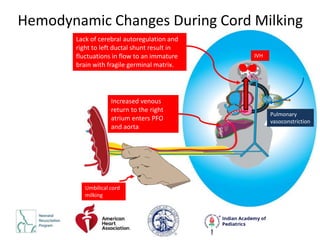
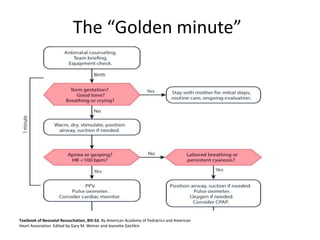
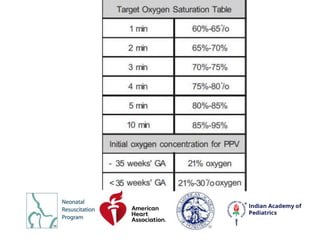
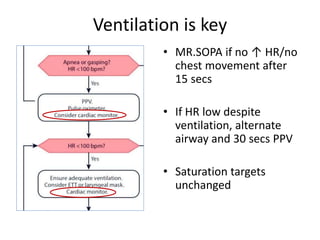
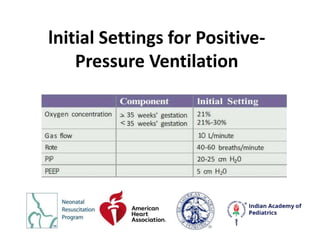
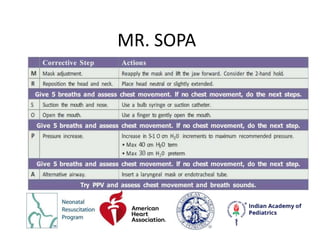
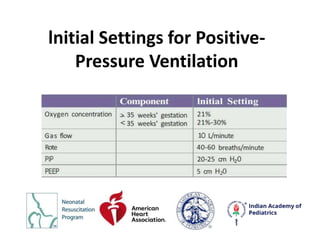
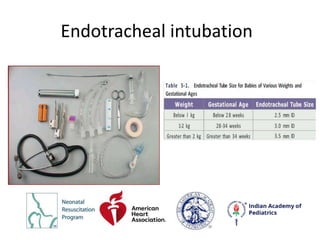
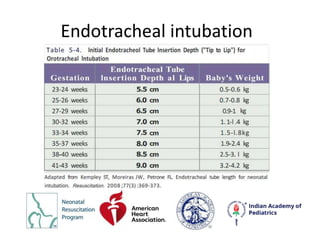
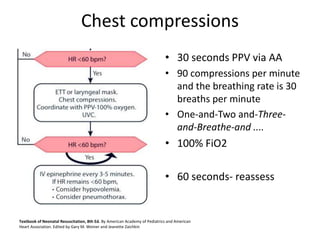
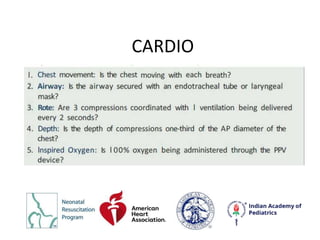
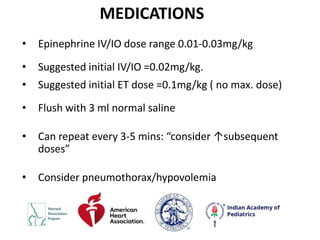
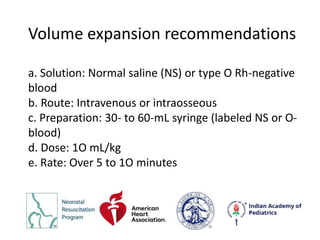
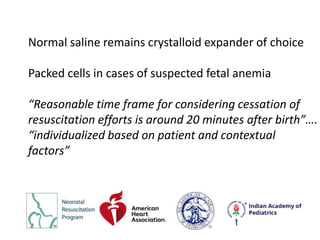
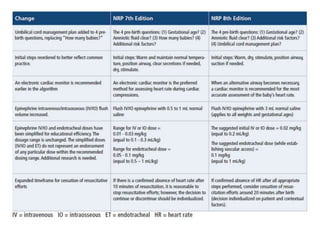
The document outlines the protocols and considerations of neonatal resuscitation as detailed in the 8th edition of the textbook by the American Academy of Pediatrics and American Heart Association. Key points include the importance of pre-birth preparation, ventilation techniques, administration of medications like epinephrine, and post-resuscitation care, emphasizing close monitoring and individualized assessment. Recommendations for umbilical cord management and the significance of timely interventions are highlighted throughout.