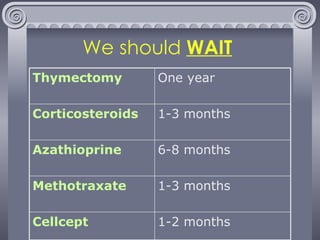
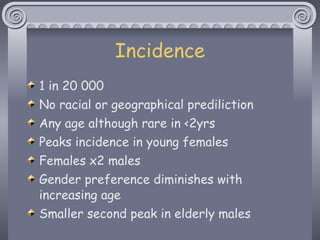
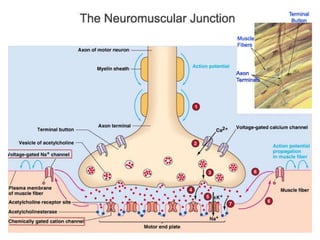
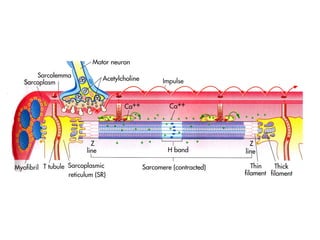
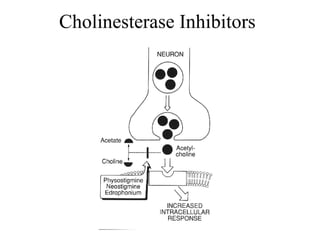
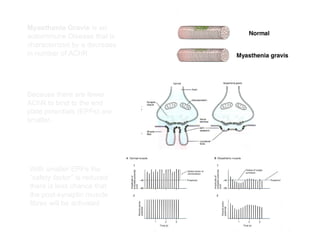
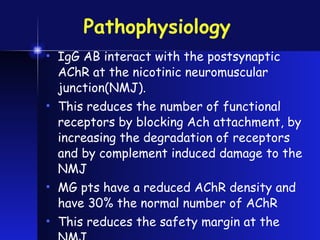
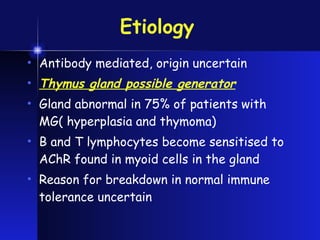
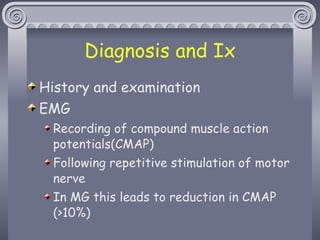
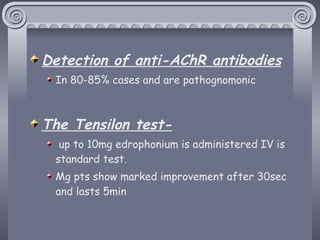
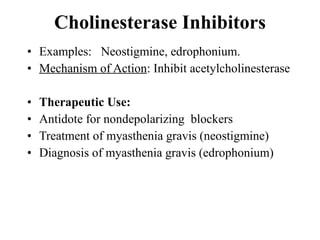
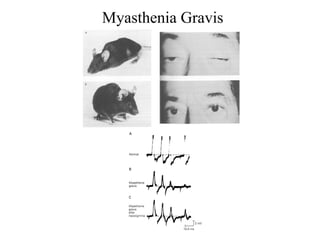
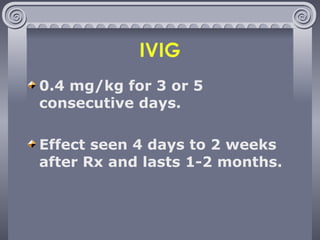
This document summarizes key information about Myasthenia Gravis (MG), an autoimmune disorder characterized by muscle weakness and fatigue. It discusses the epidemiology of MG, noting peaks in incidence among younger females. The pathophysiology involves antibodies interacting with acetylcholine receptors at the neuromuscular junction, reducing receptor numbers. Diagnosis involves testing for antibodies and response to cholinesterase inhibitors. Treatment focuses on immunomodulation including plasmapheresis, IVIG, thymectomy and immunosuppressive drugs.


![http://groups.google.com/group/alexneuropsych E-mail: [email_address] [email_address]](https://image.slidesharecdn.com/myastheniagravis-101216150838-phpapp02/85/Myasthenia-gravis-3-320.jpg)
![Clinical Myasthenia gravis (MG) is a neuromuscular junction transmission disorder characterized by muscle weakness and fatigue. Peaks around the 2 nd and 3 rd decades and the 6 th and 7 th decades of life. The prevalence of myasthenia gravis ranges between 4-14/100,000. [Orphan disease]](https://image.slidesharecdn.com/myastheniagravis-101216150838-phpapp02/85/Myasthenia-gravis-5-320.jpg)
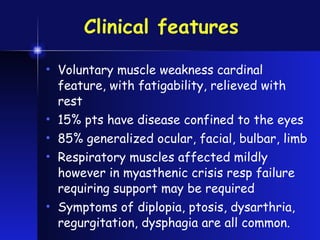
![Clinical [cont.] The salient clinical features of myasthenia gravis are skeletal muscle weakness and fatigability. Symptoms are usually aggravated by physical activity and relieved by rest. 60% starts in the ocular muscles , with ptosis and/or diplopia. 15% remain confined to the eye muscles. 85% weakness spreads to facial, bulbar, and limb muscles.](https://image.slidesharecdn.com/myastheniagravis-101216150838-phpapp02/85/Myasthenia-gravis-16-320.jpg)

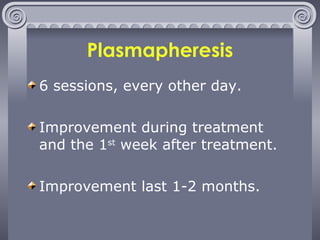
![Immunomodulatory therapy [Short-term] Plasmapheresis. IVIG When acute temporary improvement is needed.](https://image.slidesharecdn.com/myastheniagravis-101216150838-phpapp02/85/Myasthenia-gravis-24-320.jpg)
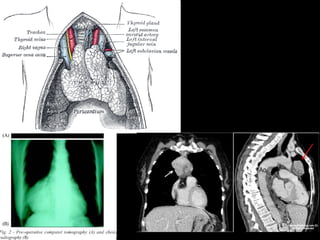
![Immunomodulatory therapy [long-term] Thymectomy. Immunomodulatory drugs. To induce remission](https://image.slidesharecdn.com/myastheniagravis-101216150838-phpapp02/85/Myasthenia-gravis-27-320.jpg)
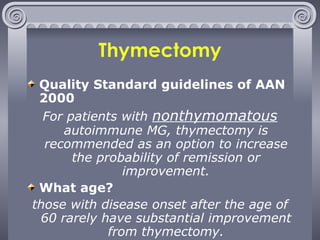
![Thymectomy [cont.] Thymoma : Do thmectomy due to risk of invasive thymoma, heart and lung damage, phrenic nerve damage, and other problems. Acetylcholine receptor antibodies : thymectomy may help. MUSK antibodies : thymectomy does not help. No antibodies : unknown if thymectomy helps.](https://image.slidesharecdn.com/myastheniagravis-101216150838-phpapp02/85/Myasthenia-gravis-29-320.jpg)
![Immunomodulatory Drugs [Long-term] Corticosteroids.[15 $/month] Azathioprine.[70-140$/month] Methotrexate [10-25 mg q week – 13-30$/month] Mycophenolate mofetil (CellCept). [1g BID – 400-600$/month] Cyclosporine A [5 mg/kg BID – 400-600$/month] Cyclophosphamide. [20 mg q week IV – 100-300$/month]](https://image.slidesharecdn.com/myastheniagravis-101216150838-phpapp02/85/Myasthenia-gravis-30-320.jpg)