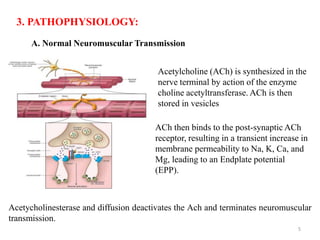
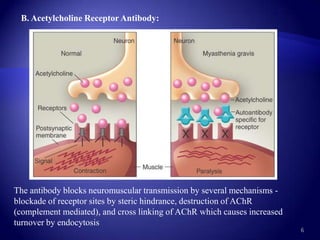
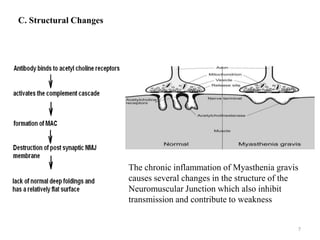
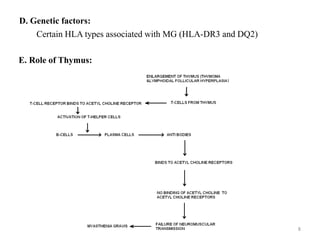
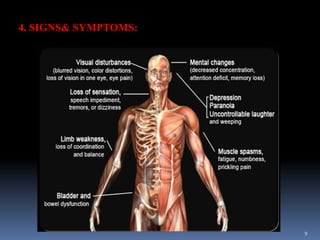
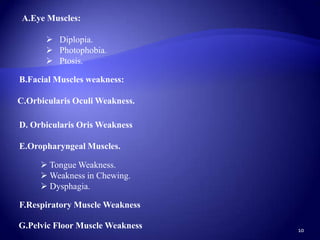
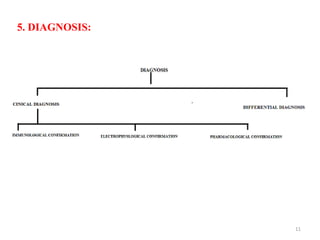
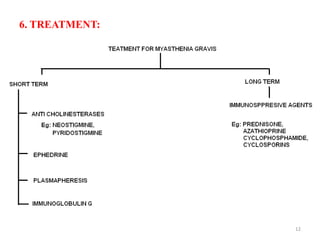
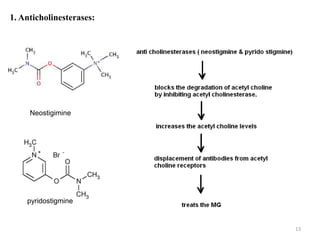
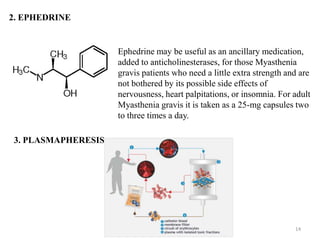
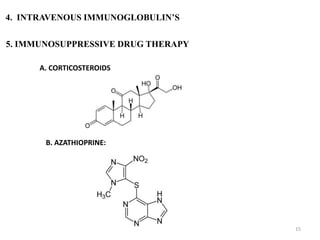
The document summarizes myasthenia gravis (MG), an autoimmune disorder causing muscle weakness. MG results from antibodies blocking acetylcholine receptors at the neuromuscular junction, inhibiting nerve signal transmission. Signs and symptoms include weakness of eye, facial, swallowing, and respiratory muscles. Diagnosis involves testing for acetylcholine receptor antibodies. Treatment includes anticholinesterases, immunosuppressants, plasmapheresis, IV immunoglobulins, and sometimes thymectomy. While the immune system's role is clear, further research is still needed to develop more effective medical treatments without adverse effects.