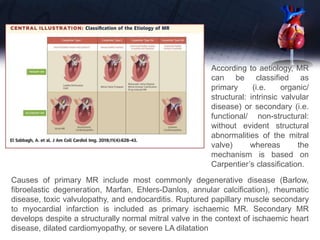
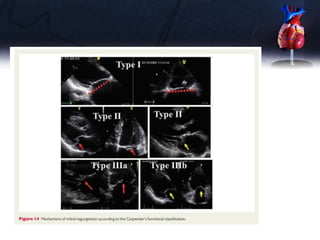
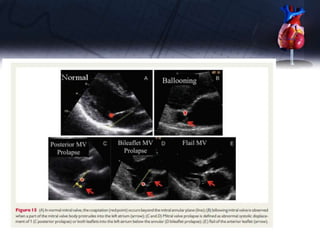
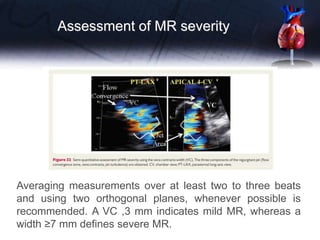
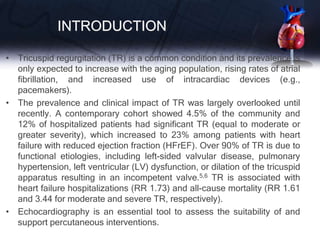
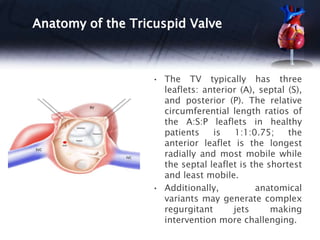
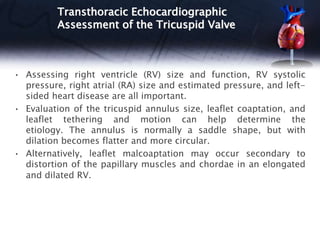
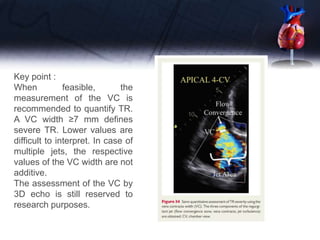
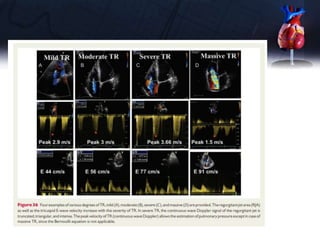
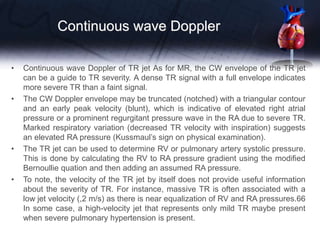
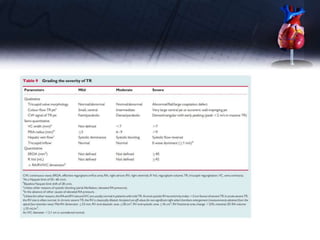
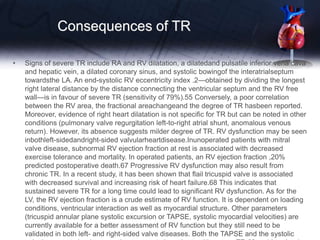
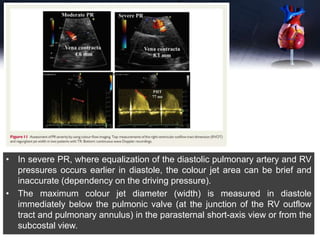
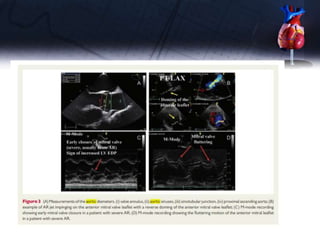
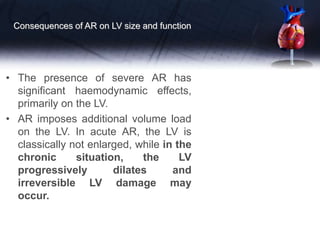
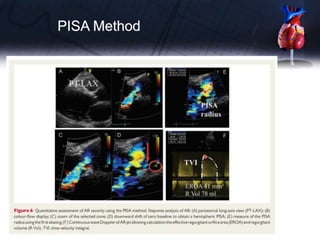
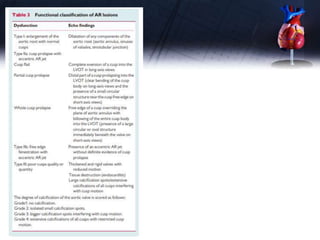
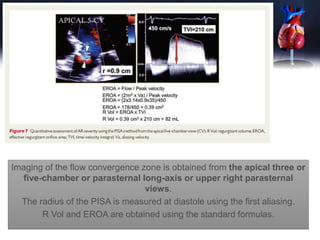
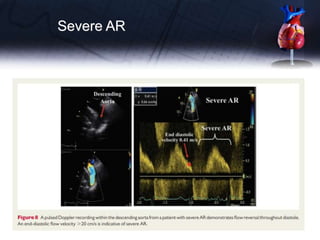
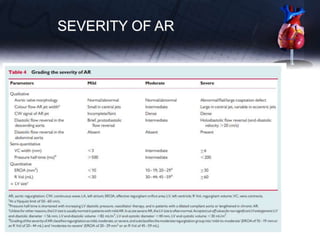
This document discusses the echocardiographic assessment of valvular regurgitation, focusing on mitral and tricuspid regurgitation. It describes the anatomy and causes of mitral and tricuspid regurgitation. Quantitative methods for assessing regurgitation severity include vena contracta width, proximal isovelocity surface area, and regurgitant volume. Consequences of significant regurgitation include left ventricular and atrial enlargement. Echocardiography is important for evaluating regurgitation severity and mechanisms to guide treatment decisions.

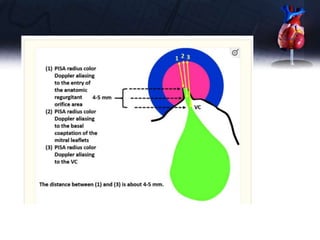
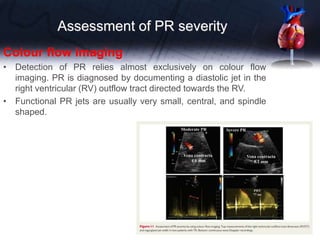
![• A careful assessment of the regurgitant jet by
colour Doppler, using multiple views, can rapidly
diagnose minimal regurgitation, which requires a
priori no further quantification.
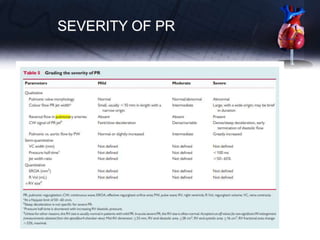
• In the other cases, the use of a more quantitative
method is advised when feasible [vena contracta
(VC); proximal isovelocity surface area (PISA)]](https://image.slidesharecdn.com/pptvalveregurgitation-230913155533-c60ce715/85/ppt-VALVE-REGURGITATION-pptx-6-320.jpg)