1. The CQC has developed a new approach to inspecting hospitals that involves a 3 phase process of preparation, site visits, and reporting.
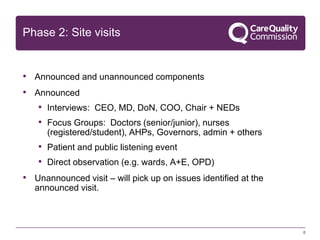
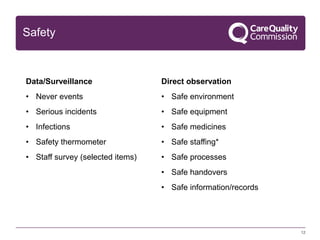
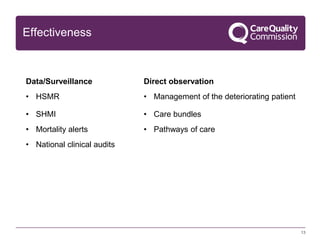
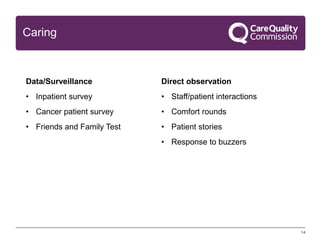
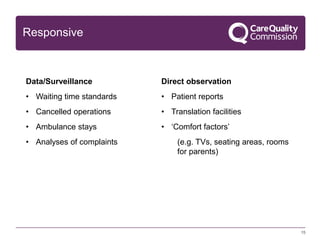
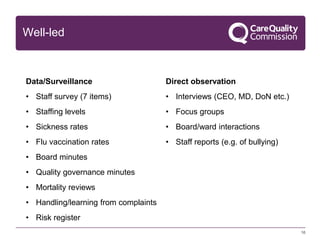
2. Site visits will involve both announced and unannounced components, including interviews, focus groups, observations, and reviewing data. Inspections will evaluate hospitals on whether they are safe, effective, caring, responsive, and well-led.
3. Hospitals will receive ratings of outstanding, good, requires improvement, or inadequate. The goal is to inspect all acute NHS hospitals by December 2015 and provide ratings to help improve quality of care.