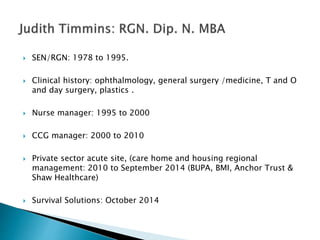
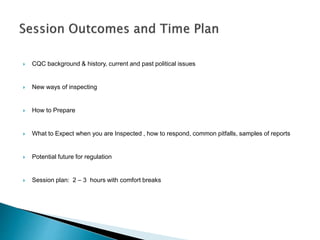
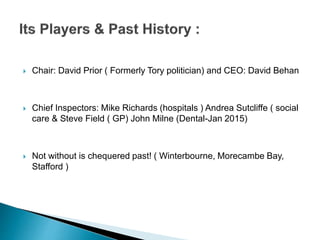
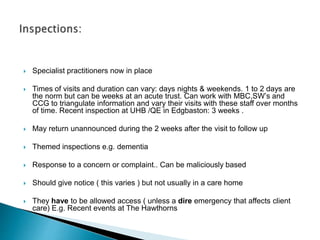
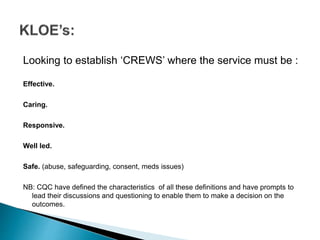
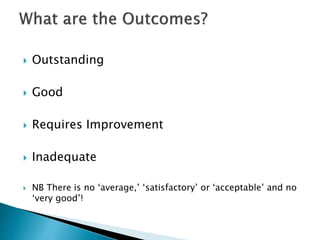
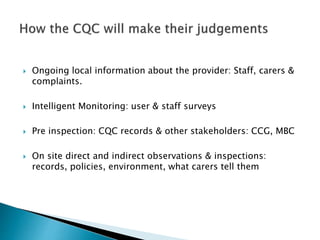
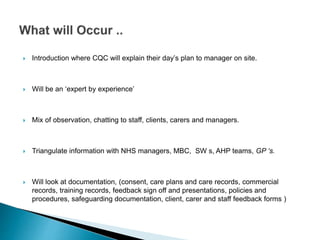
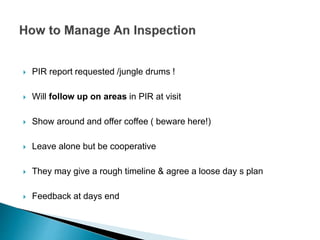
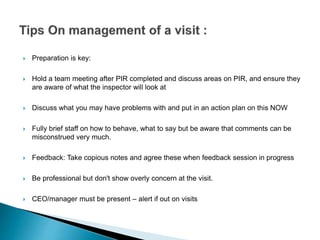
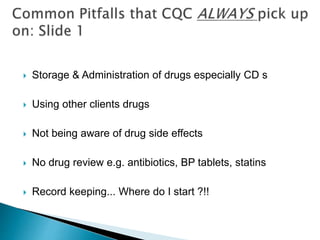
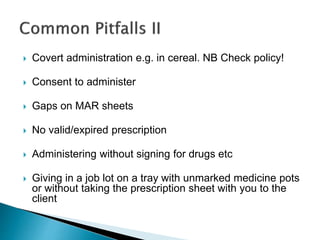
This document provides an overview and summary of a presentation on compliance with the Care Quality Commission (CQC) in the United Kingdom. It outlines the speaker's background and experience in nursing and healthcare management. The document then covers key topics that will be discussed in the presentation, including an introduction to the CQC, how inspections are conducted, what standards providers are evaluated on, common pitfalls seen during inspections, and potential future directions for healthcare regulation in the UK. The intended session length is 2-3 hours and will provide attendees with information to help their organizations prepare for and succeed during CQC inspections and evaluations of compliance.