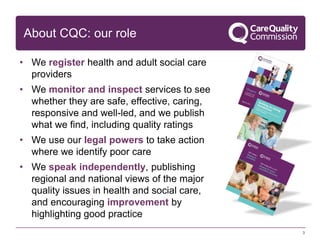
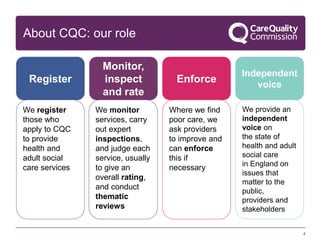
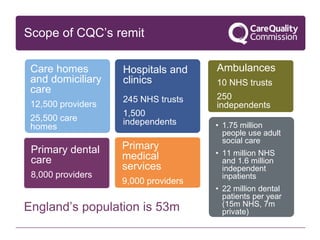
The document provides an overview of the Care Quality Commission (CQC) and its role in regulating health and social care services in England. Some key points:
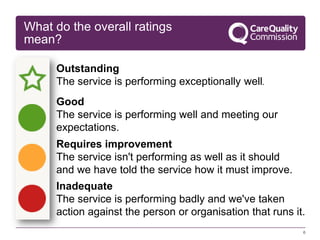
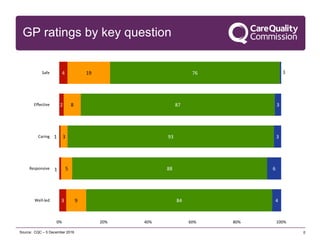
- CQC registers providers, monitors and inspects services to assess safety, effectiveness, caring, responsiveness and leadership. It publishes ratings and takes action on poor care.
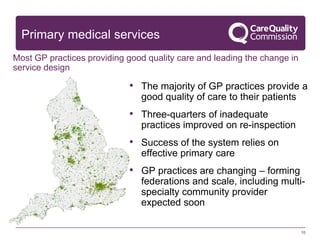
- Most GP practices provide good quality care, with 87% rated good or outstanding. Strong leadership and governance are important for delivering high quality care.
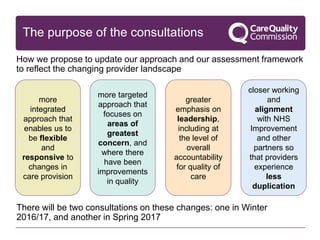
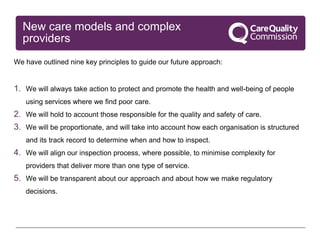
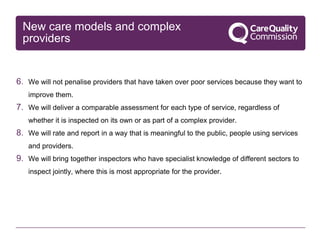
- CQC is moving to a more targeted and responsive approach focused on greatest risks. It will work more closely with other organizations to reduce duplication for providers.
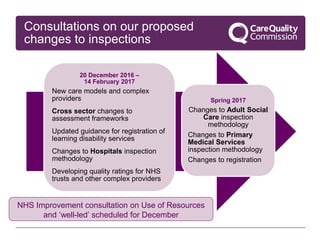
- Upcoming consultations will seek feedback on proposed changes to inspection