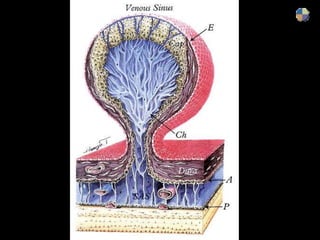
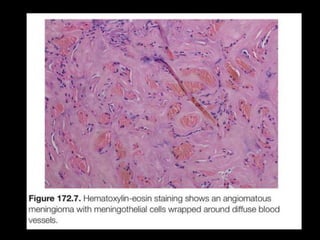
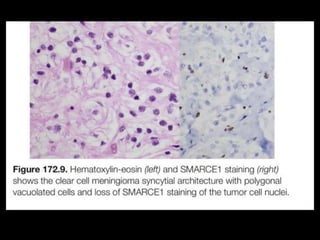
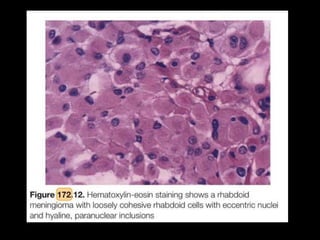
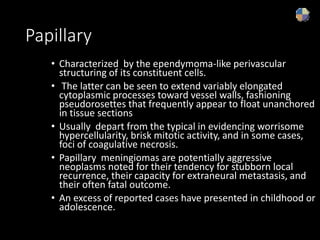
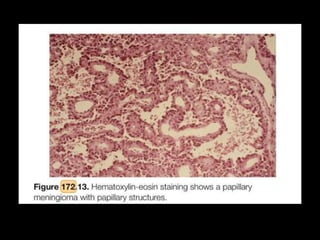
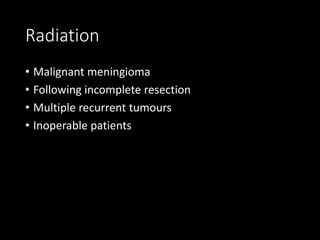
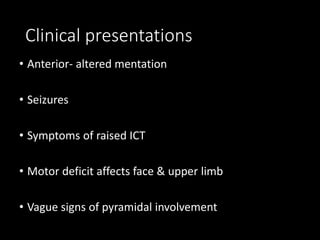
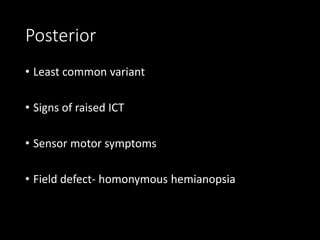
Meningiomas are tumors that arise from meningothelial cells of the arachnoid mater. They constitute 20% of all primary intracranial tumors with an incidence of 2.3 per 100,000 people. On pathology, meningiomas are graded based on their malignant potential from Grade I to Grade III. Grade I meningiomas include meningothelial, fibrous, transitional and psammomatous subtypes. Grade II are atypical meningiomas and Grade III include anaplastic, papillary and rhabdoid subtypes. Diagnosis is typically made based on imaging features seen on CT and MRI scans. Treatment involves surgical resection although radiation and medical management may