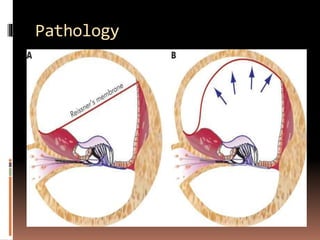
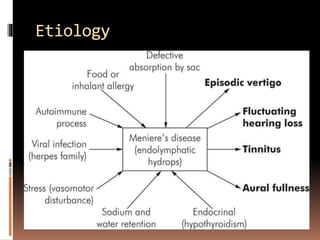
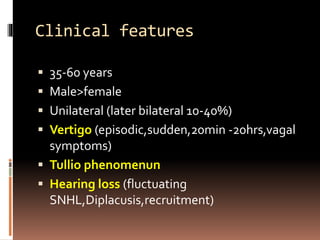
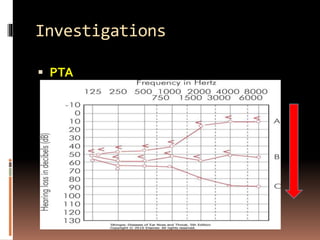
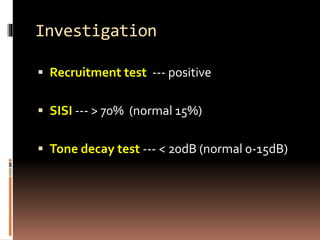
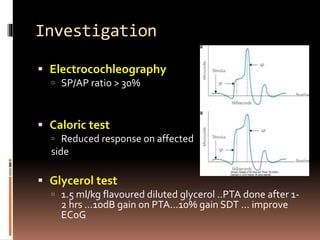
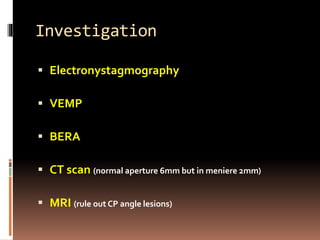
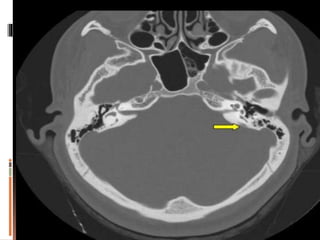
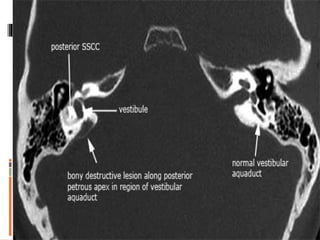
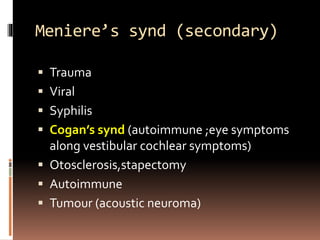
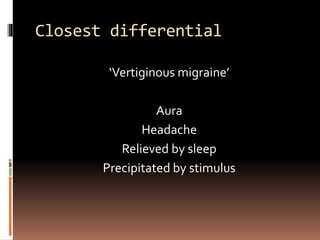
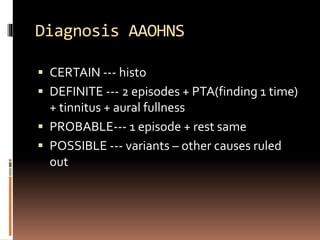
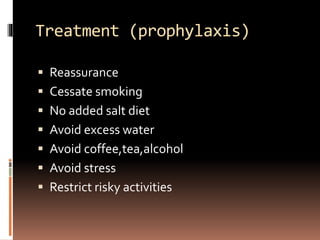
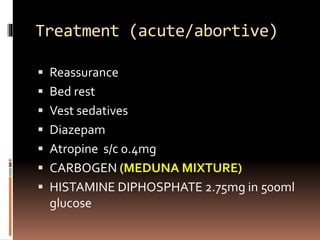
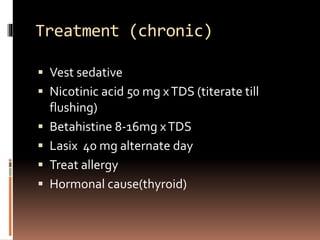
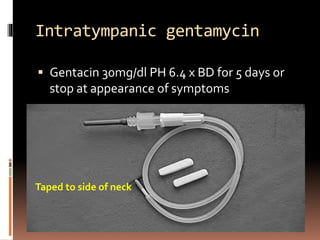
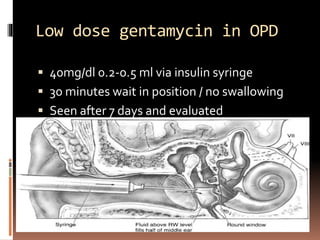
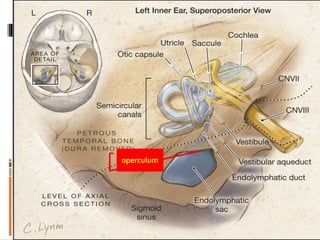
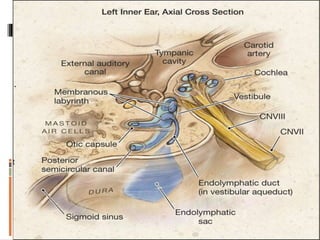
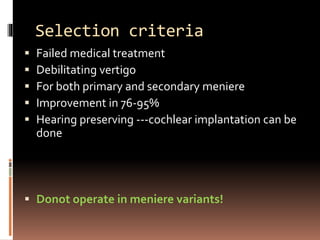
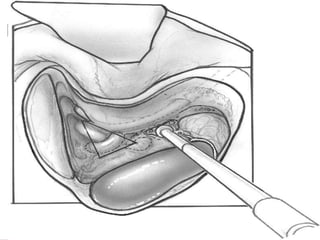
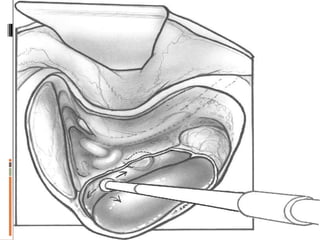
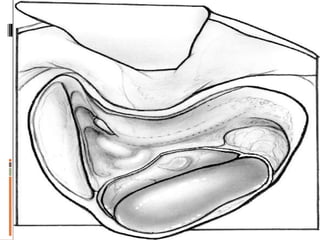
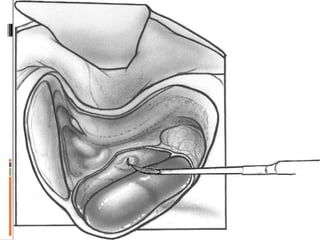
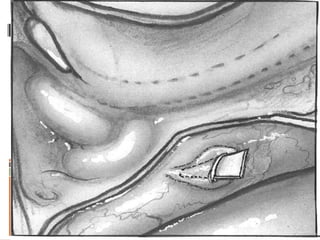
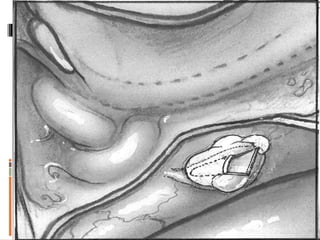
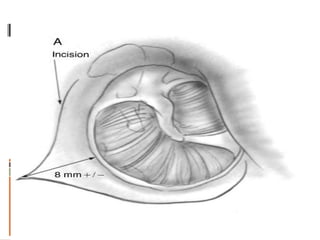
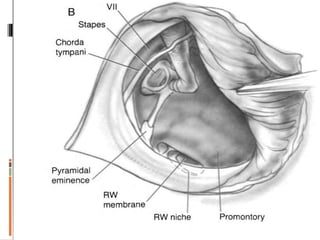
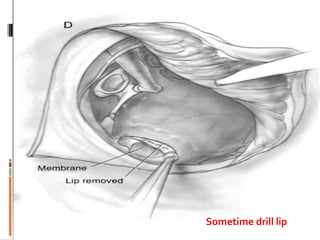
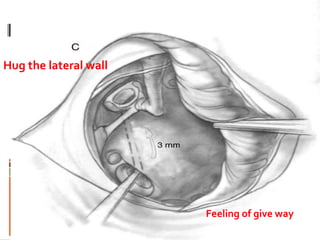
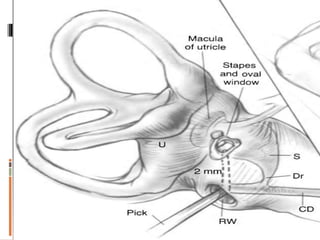
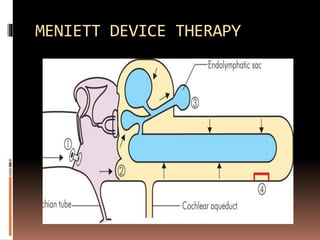
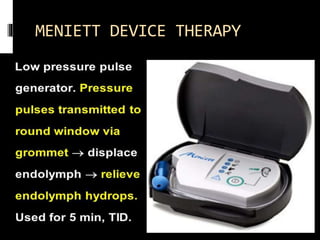
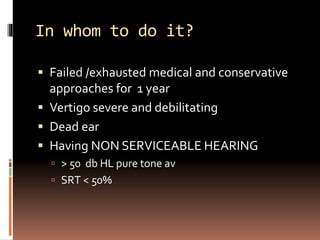
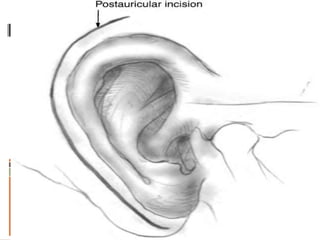
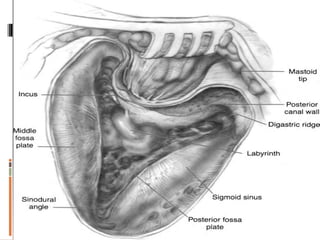
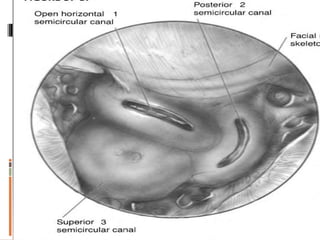
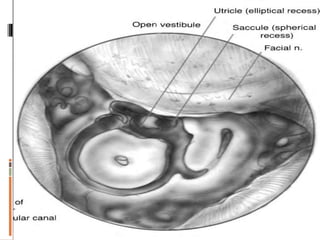
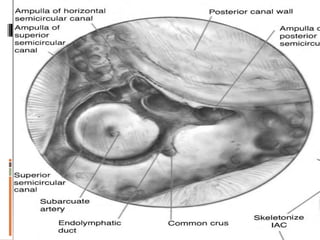
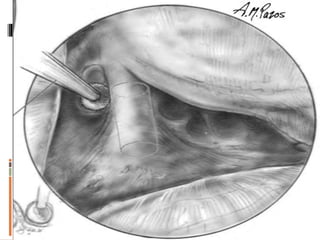
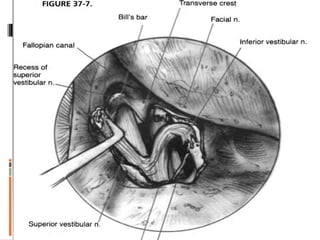
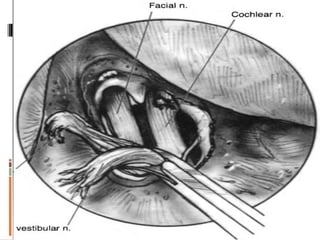
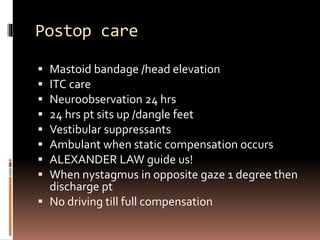
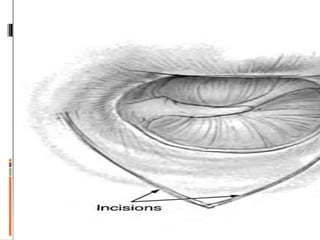
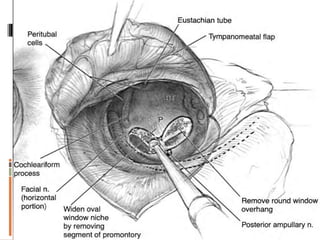
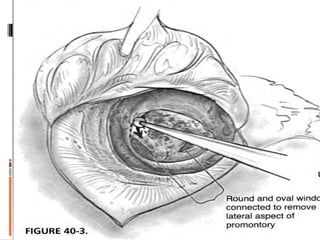
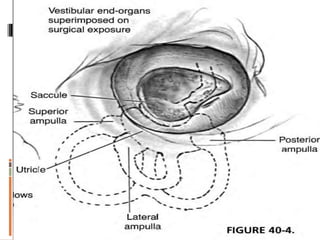
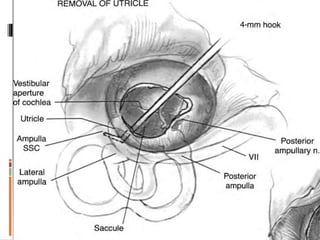
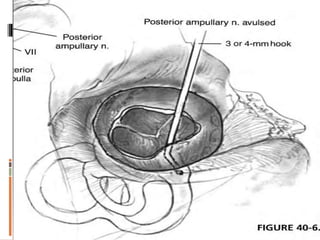
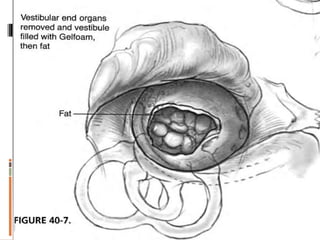
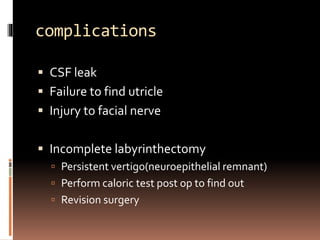
This document discusses Meniere's disease, a disorder of the inner ear that causes spontaneous episodes of vertigo, hearing loss, and tinnitus. It outlines the potential causes, clinical features, diagnostic tests, treatment options including medications, intratympanic injections, and surgical procedures like endolymphatic sac decompression or vestibular nerve sectioning. Surgical intervention is considered for patients with severe, treatment-resistant vertigo. The goal of treatment is to control vertigo attacks while preserving hearing if possible.