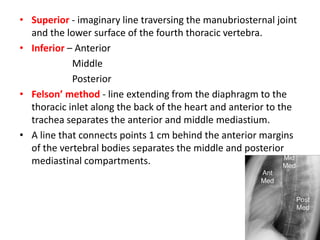
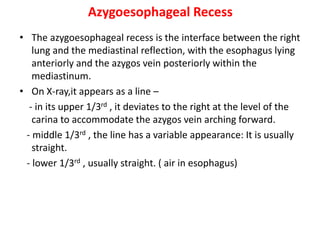
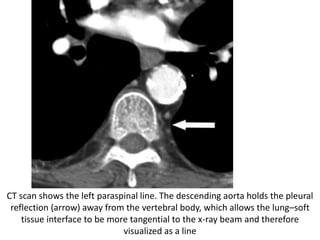
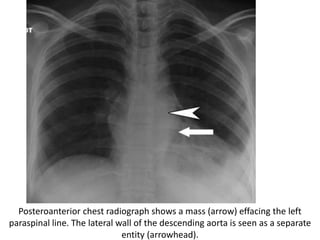
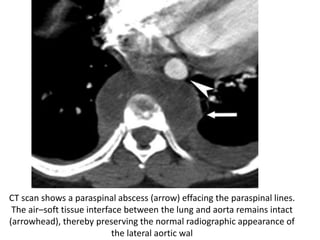
The document describes the anatomy and imaging features of the mediastinum and mediastinal masses. It defines the mediastinum and its subdivisions. Key points include:
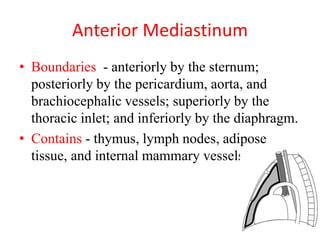
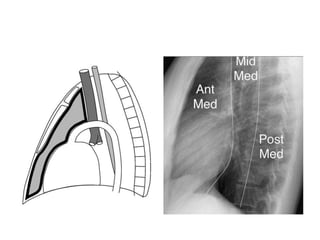
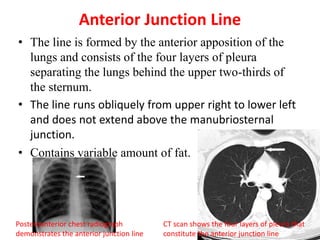
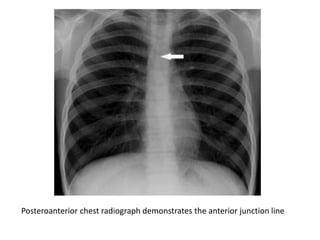
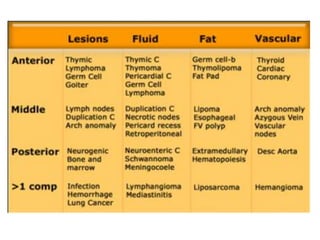
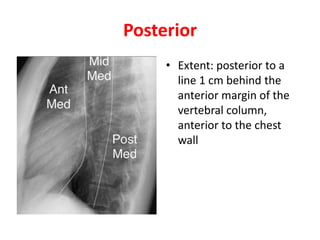
- The mediastinum is divided into anterior, middle, and posterior compartments
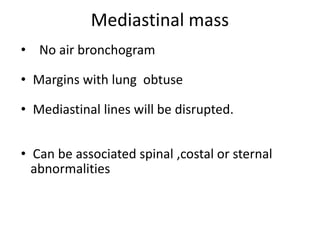
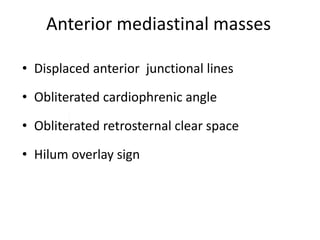
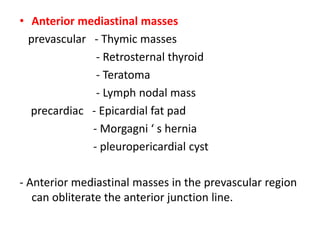
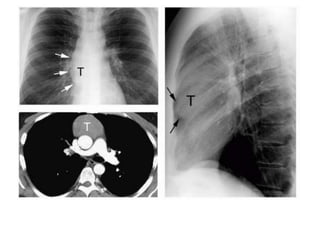
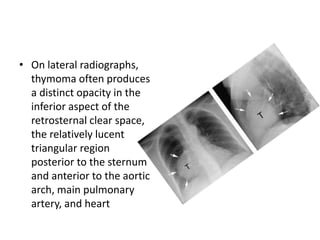
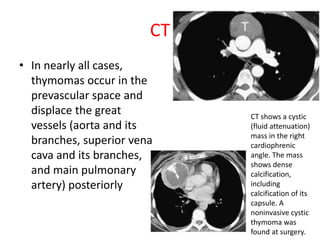
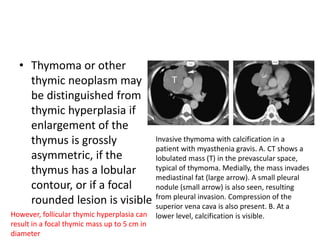
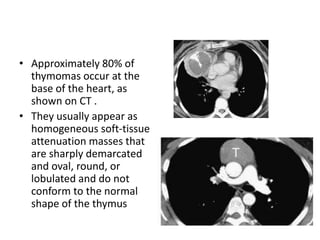
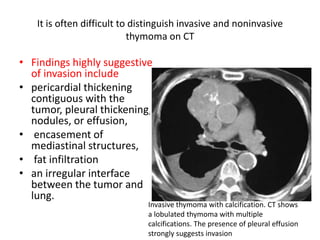
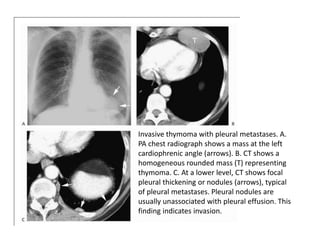
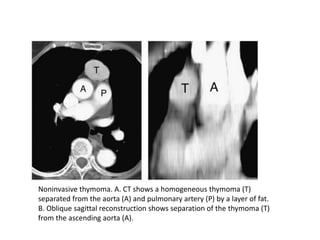
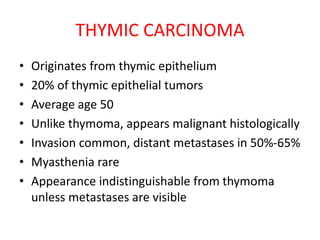
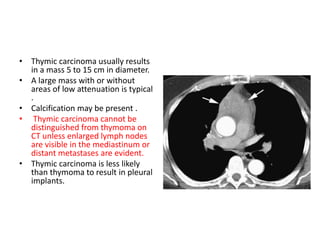
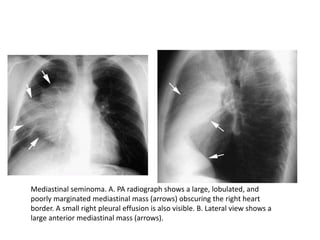
- Common anterior mediastinal masses include thymomas and lymphadenopathy which can displace mediastinal lines
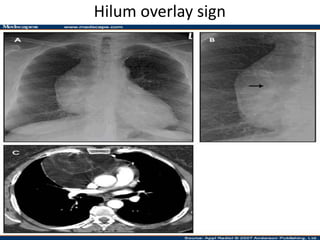
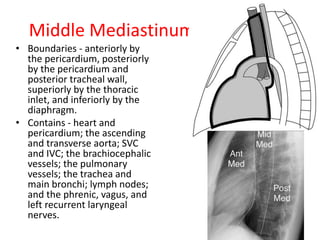
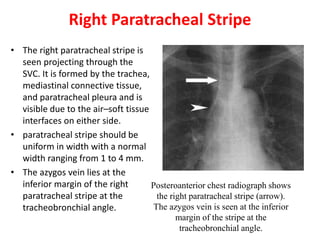
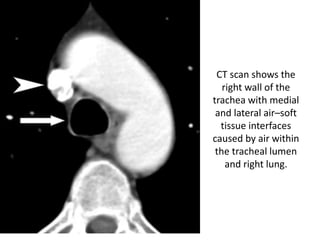
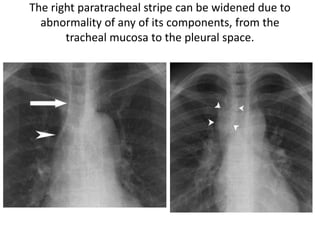
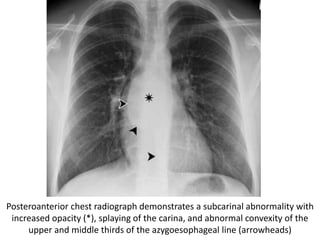
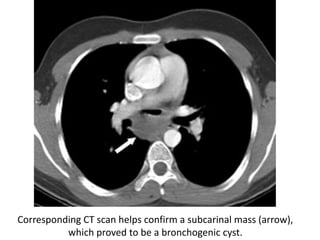
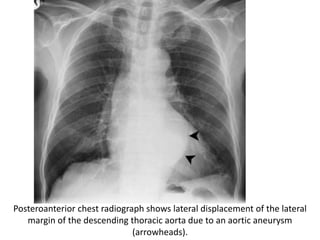
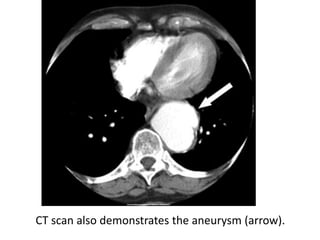
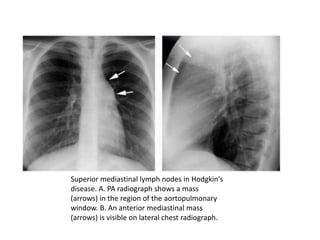
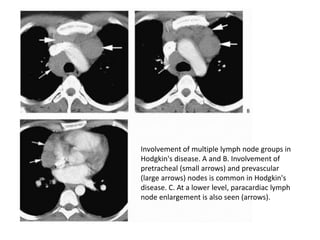
- Middle mediastinal masses include enlarged lymph nodes and vascular structures
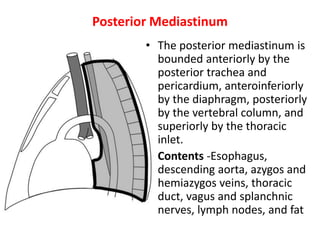
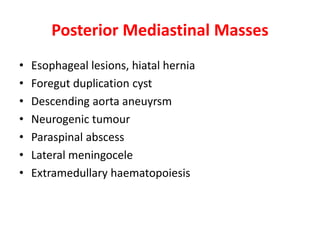
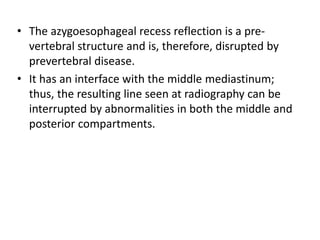
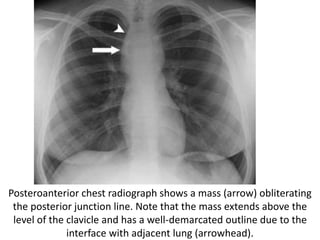
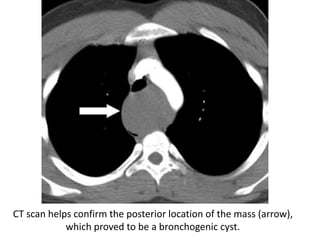
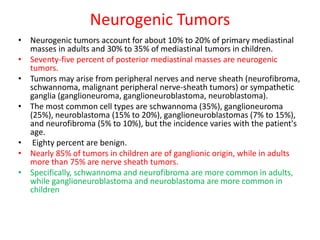
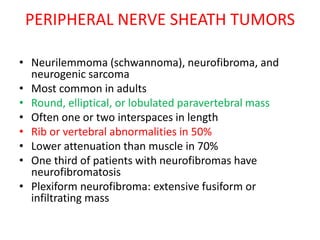
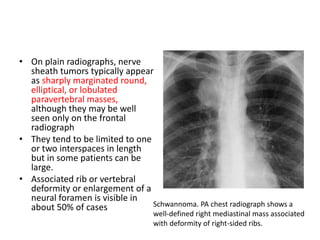
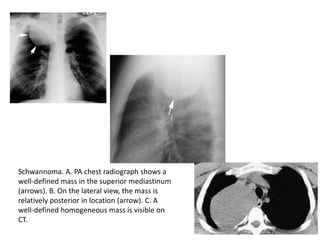
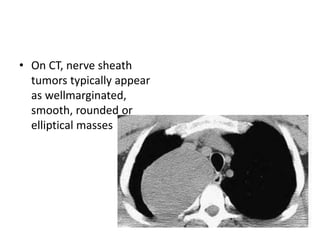
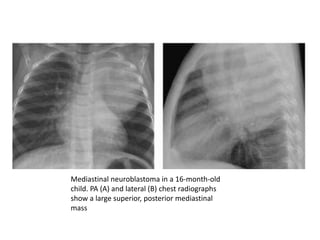
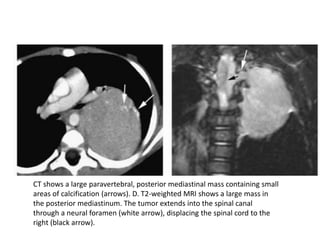
- Posterior mediastinal masses involve the esophagus and include neurogenic tumors
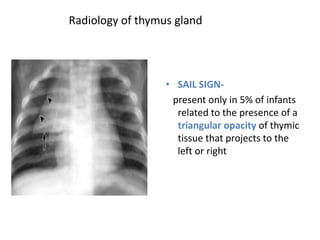
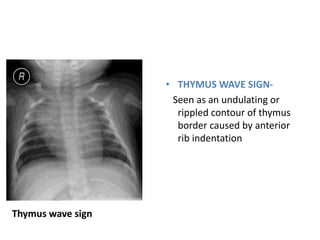
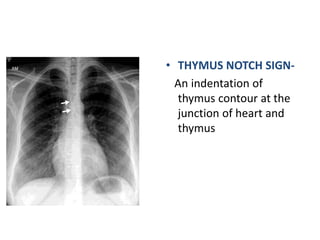
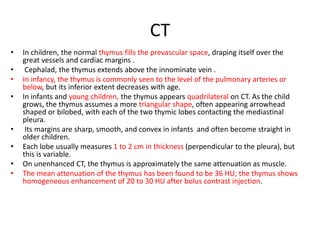
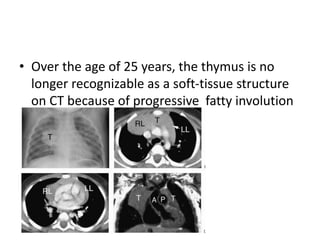
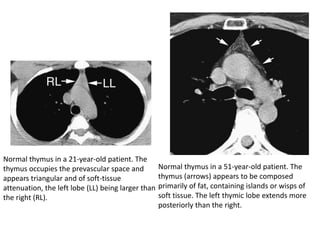
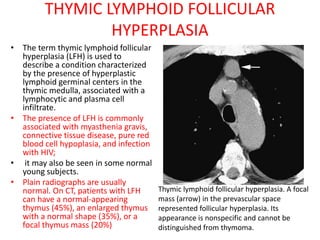
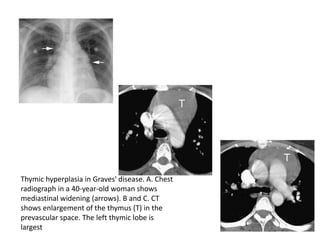
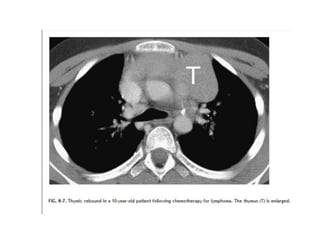
- Normal thymus anatomy and imaging signs are described as well as thymic hyperplasia and rebound