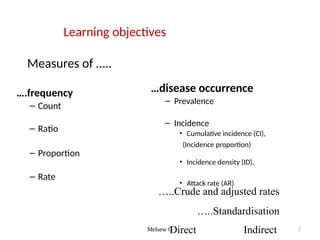
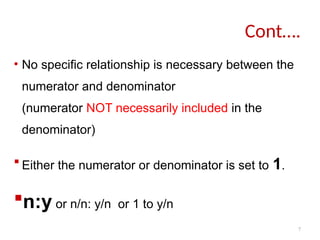
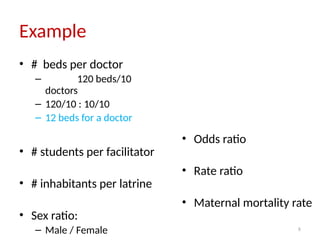
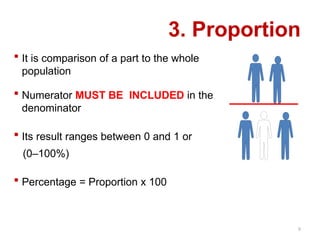
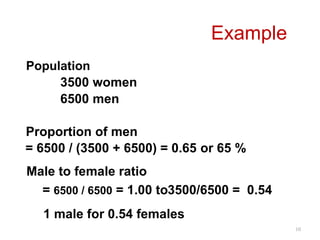
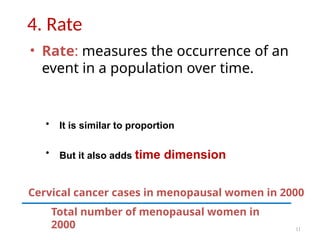
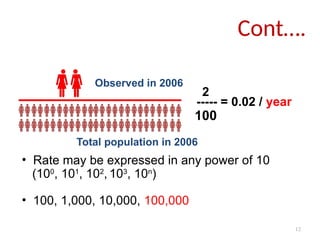
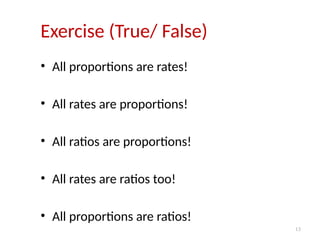
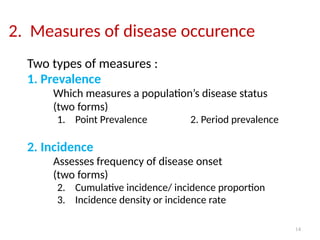
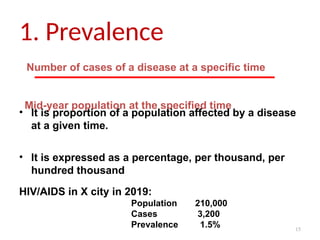
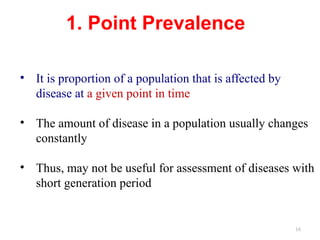
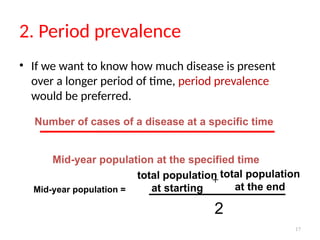
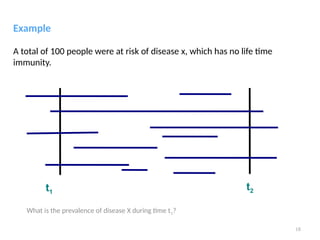
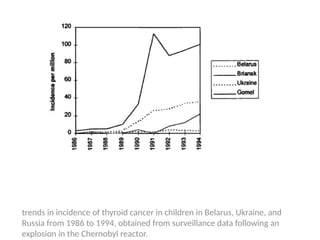
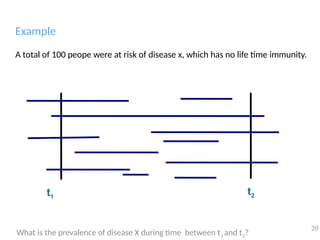
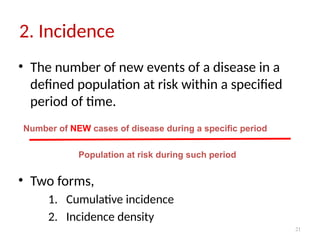
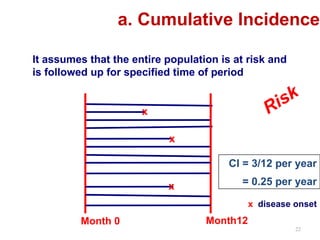
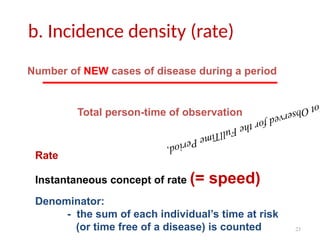
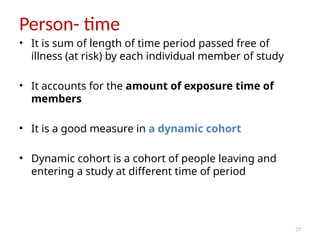
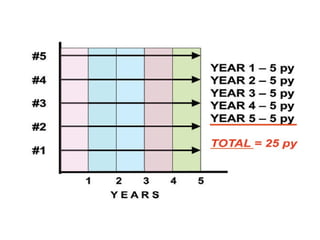
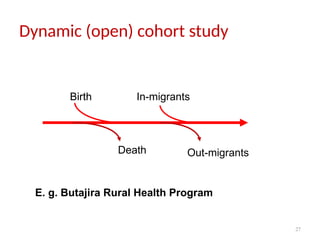
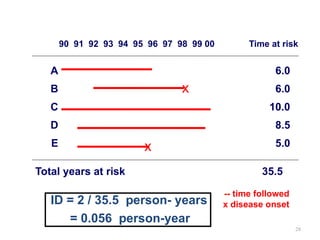
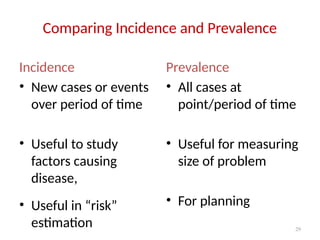
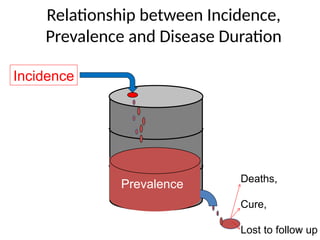
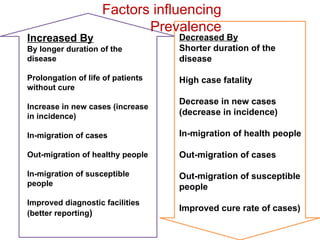
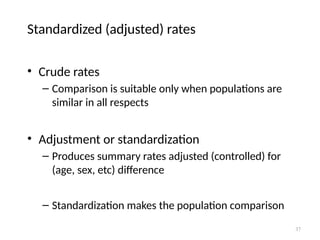
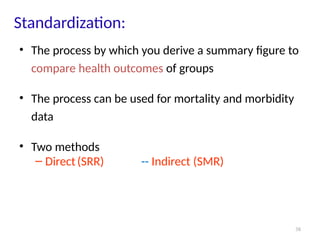
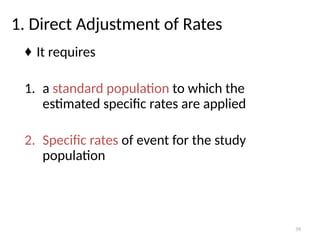
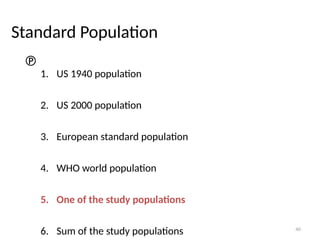
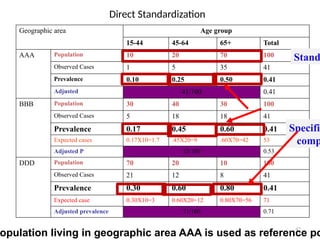
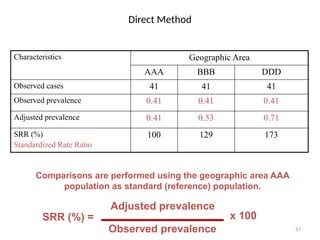
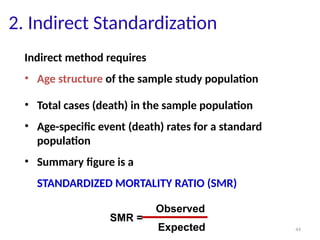
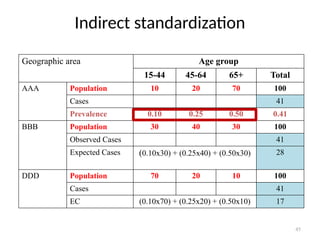
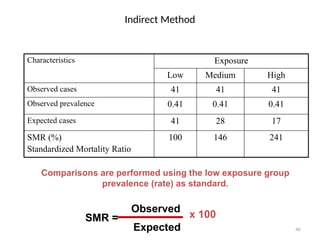
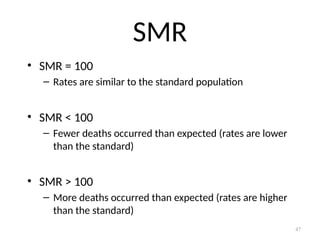
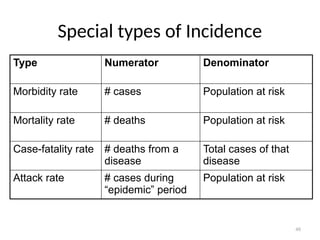
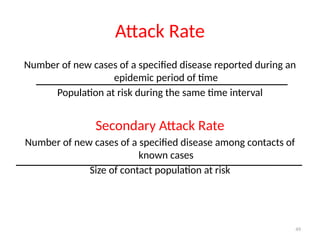
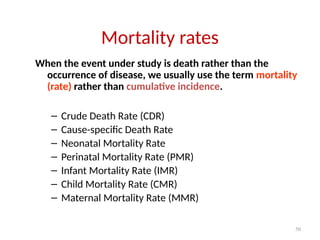
The document provides an overview of basic measurements in epidemiology, including counts, ratios, proportions, rates, prevalence, and incidence. It discusses the importance of these measures in assessing disease occurrence and understanding health outcomes, as well as different types of standardization used in calculating mortality and morbidity rates. The content emphasizes the differences between crude, specific, and standardized rates, and illustrates these concepts with various examples.