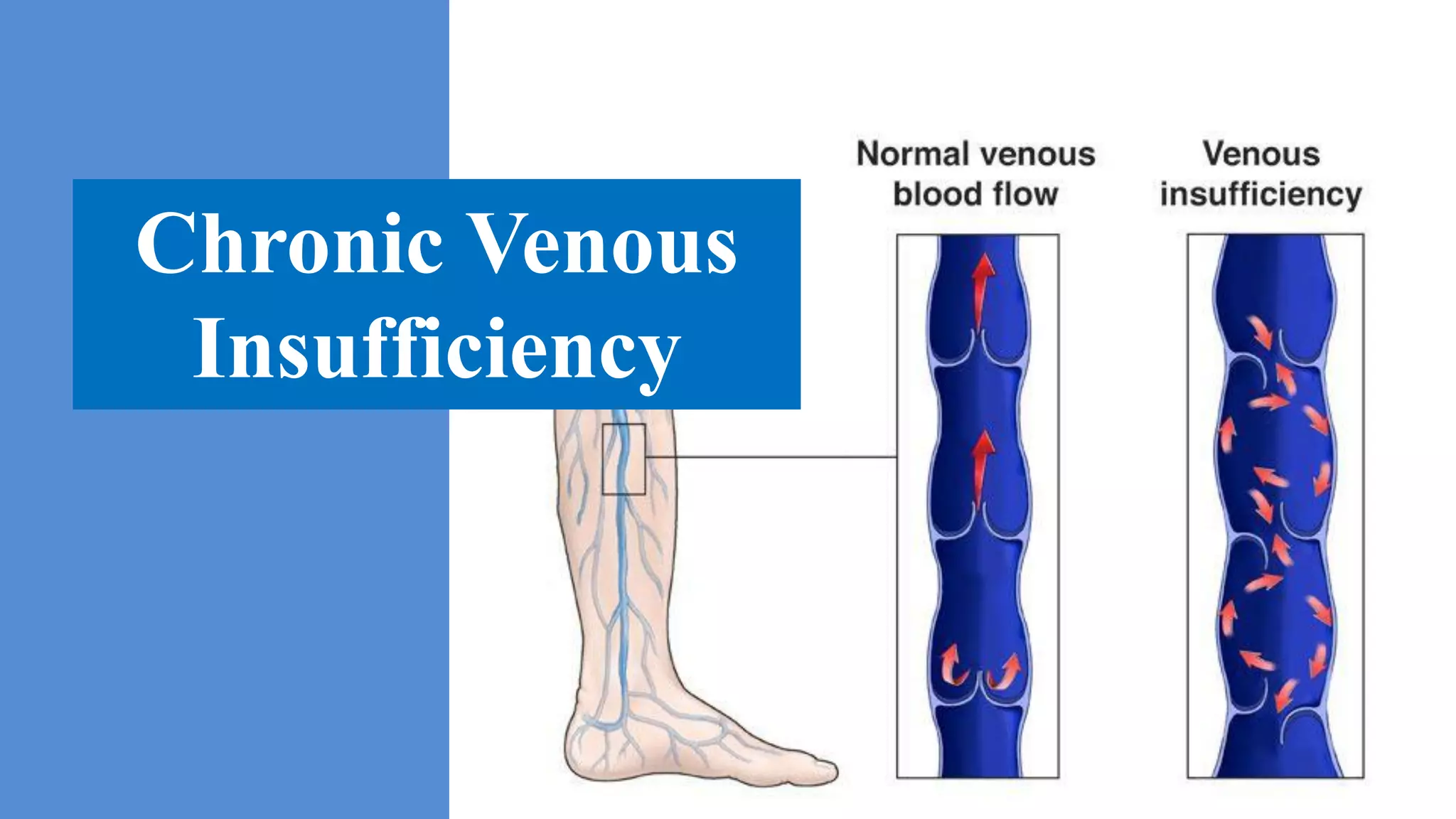
Chronic venous insufficiency (CVI) refers to functional changes that may occur in the lower extremity due to persistent elevation of venous pressures, most commonly resulting from venous reflux due to faulty valve function. CVI affects about 7% of the population and prevalence of venous leg ulcers ranges from 1% to 2%. Diagnosis involves clinical examination showing signs such as varicose veins, edema, skin changes, as well as noninvasive testing including venous duplex imaging and air plethysmography and invasive testing such as contrast venography. Pathophysiology involves retrograde blood flow due to valve incompetence leading to increased hydrostatic pressures, edema, skin changes, and ulceration through mechanisms such as venous microangiop