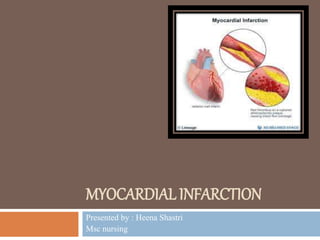
The document discusses myocardial infarction (MI), defining it as a severe decrease in oxygen supply to the heart, leading to tissue necrosis. It details the causes, clinical classifications, pathophysiology, manifestations, diagnostic evaluations, and treatments for MI, including both medical and surgical options. Additionally, it lists nursing diagnoses related to the management of patients experiencing MI.