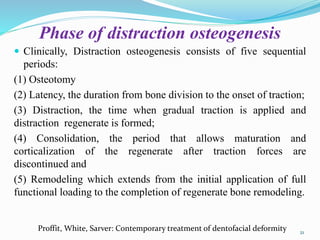
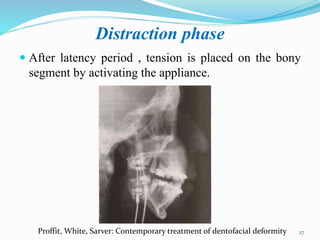
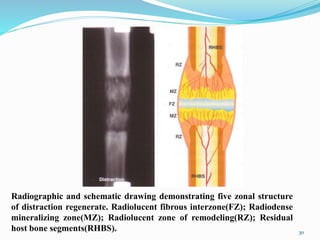
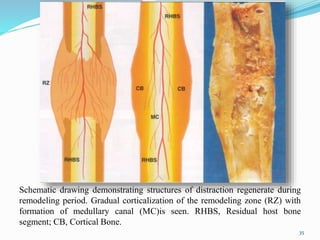
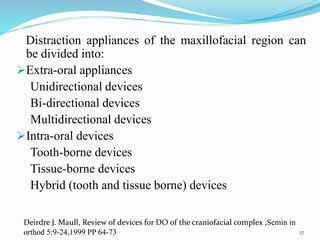
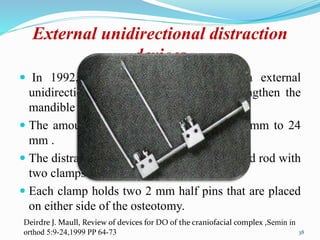
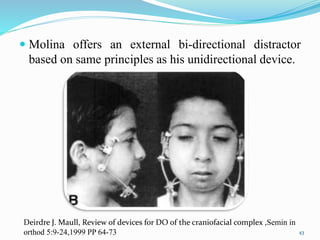
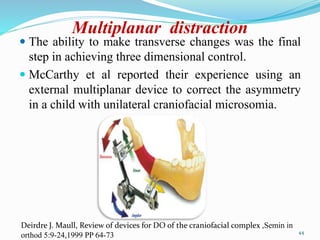
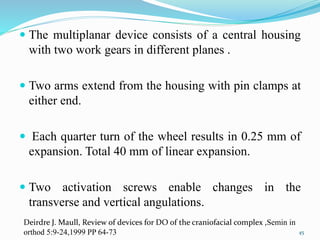
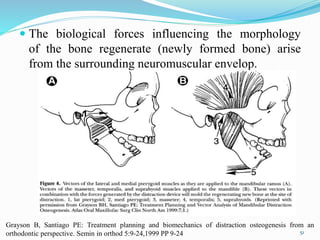
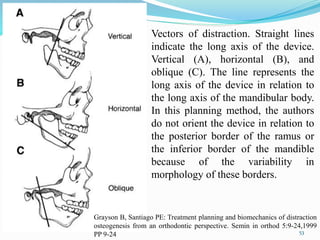
This document provides a history of distraction osteogenesis. It began in 1905 with lengthening of long bones, was pioneered for the maxillofacial region by Ilizarov in the 1950s using gradual traction to regenerate bone, and was first applied to the human mandible by McCarthy in 1989. Since then, distraction techniques have been used increasingly as alternatives to orthognathic surgery, with applications to the maxilla beginning in the 1990s and advances in device design improving three-dimensional control and outcomes. The biology of distraction osteogenesis involves regeneration of new bone between segments separated by gradual traction applied during the distraction phase.