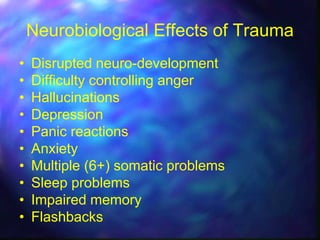
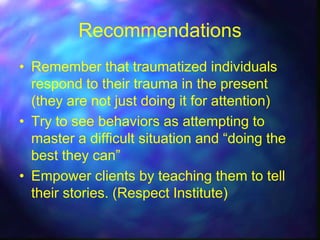
This document discusses trauma-informed care for forensic clients at Fulton State Hospital. It provides information on the hospital's clients, which include those deemed incompetent to stand trial or not guilty by reason of insanity. It also describes the hospital's security levels and treatment programs. The document discusses how trauma is prevalent among clients, especially those with disabilities or mental illness, and explains the neurological and social effects of trauma. It emphasizes the importance of trauma-informed care and providing a safe environment to avoid re-traumatization. It recommends treating trauma as a universal precaution, developing specific trauma treatment plans, and training staff to engage compassionately with clients.