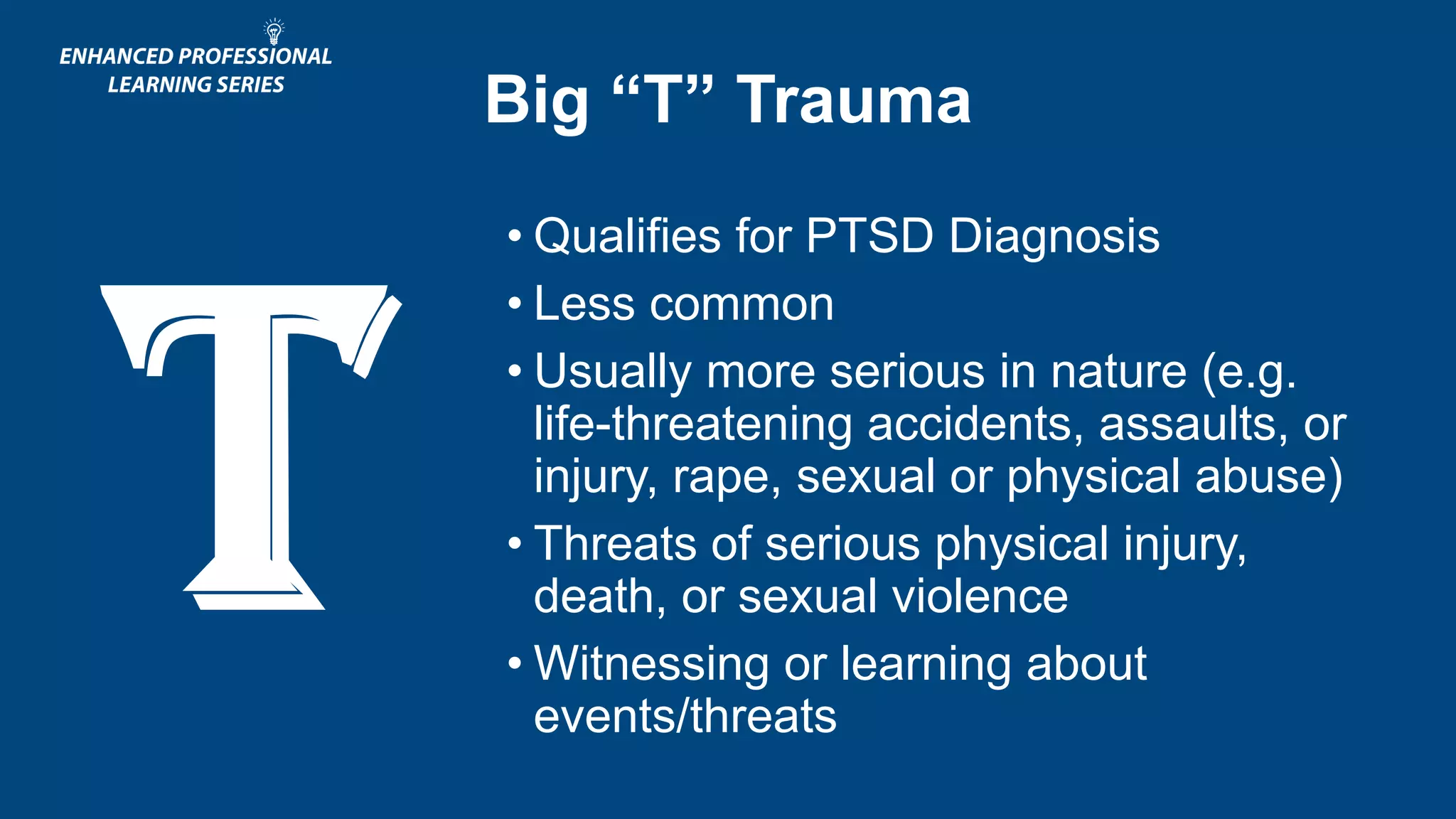
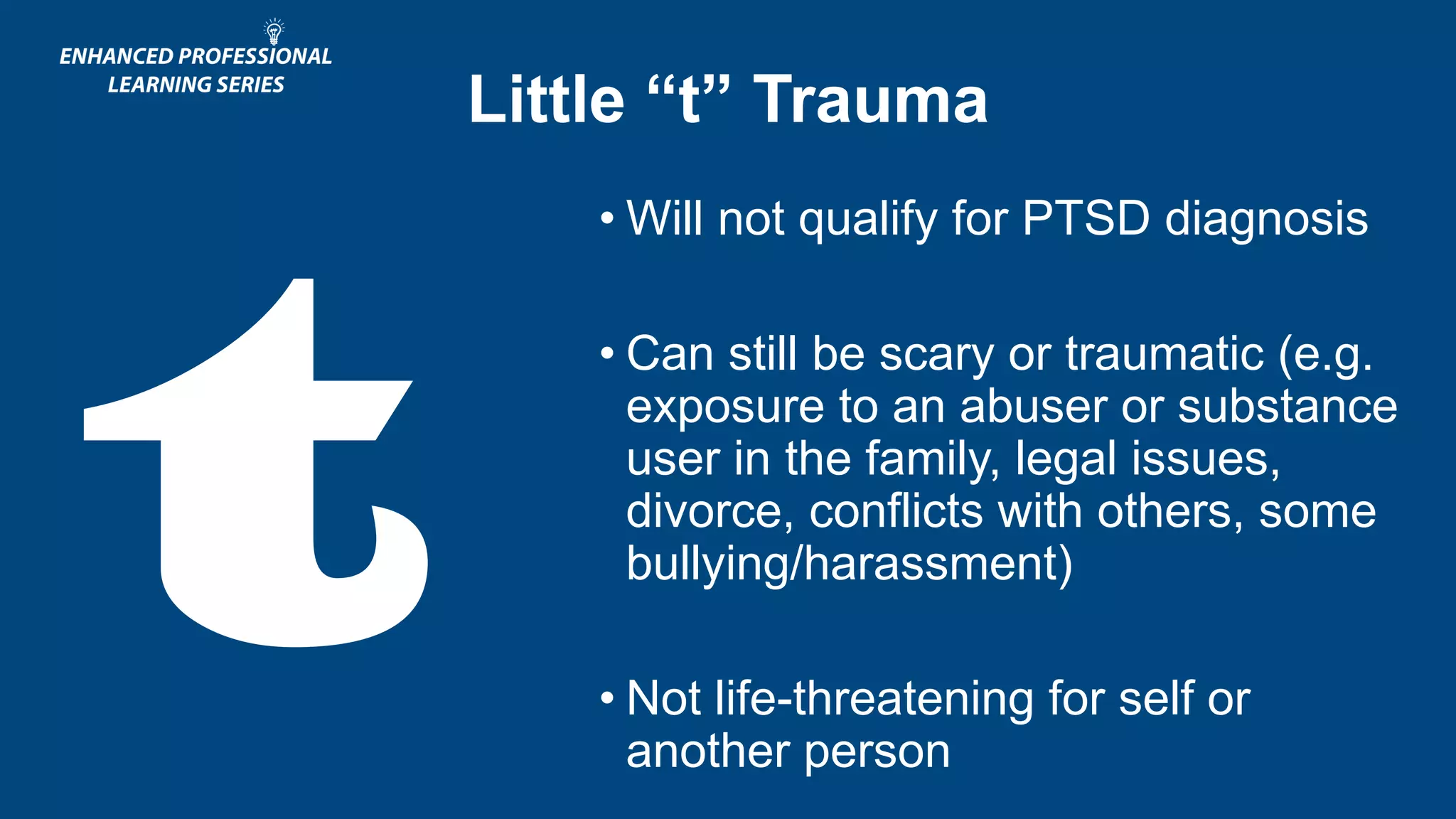
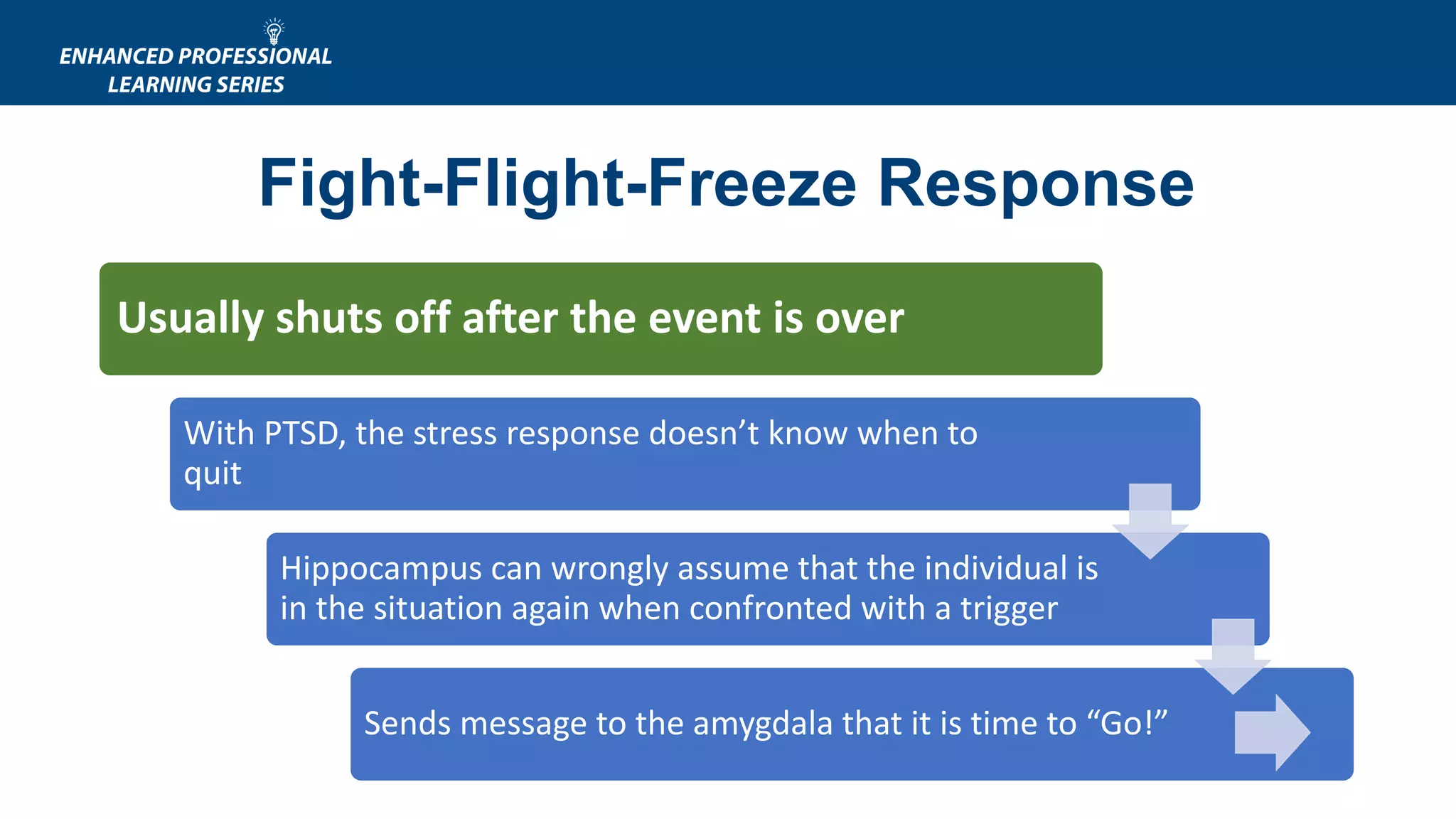
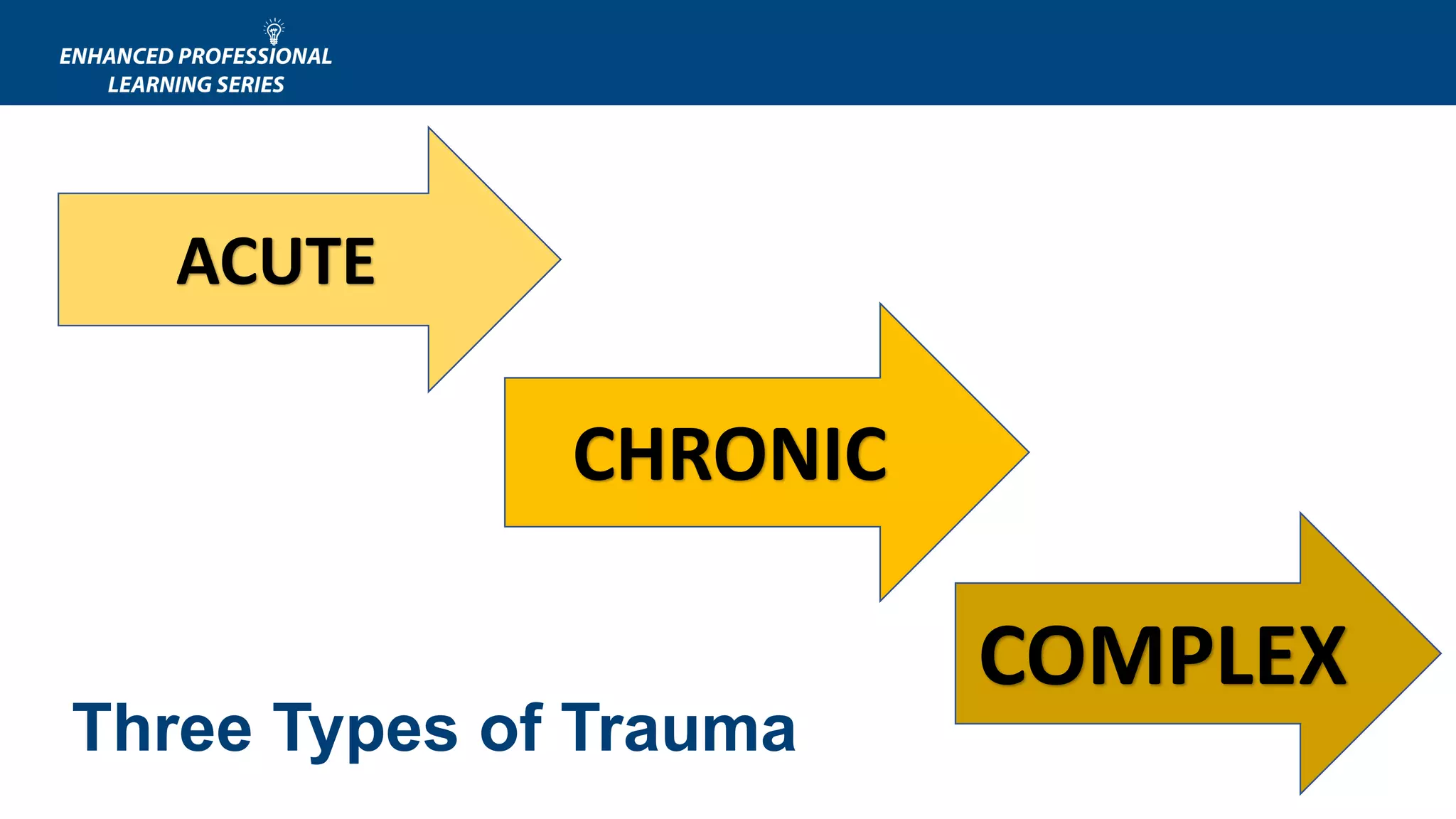
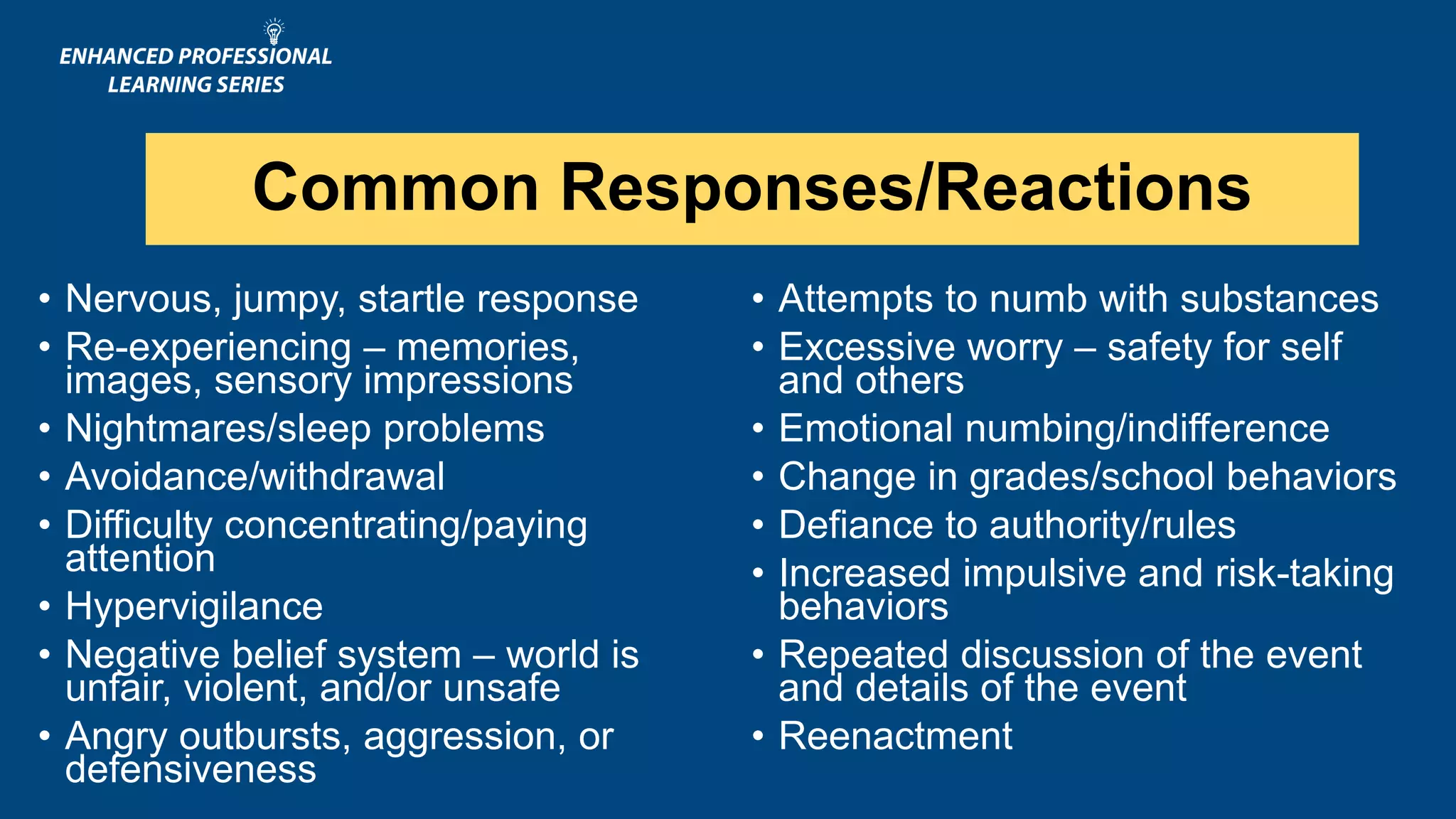
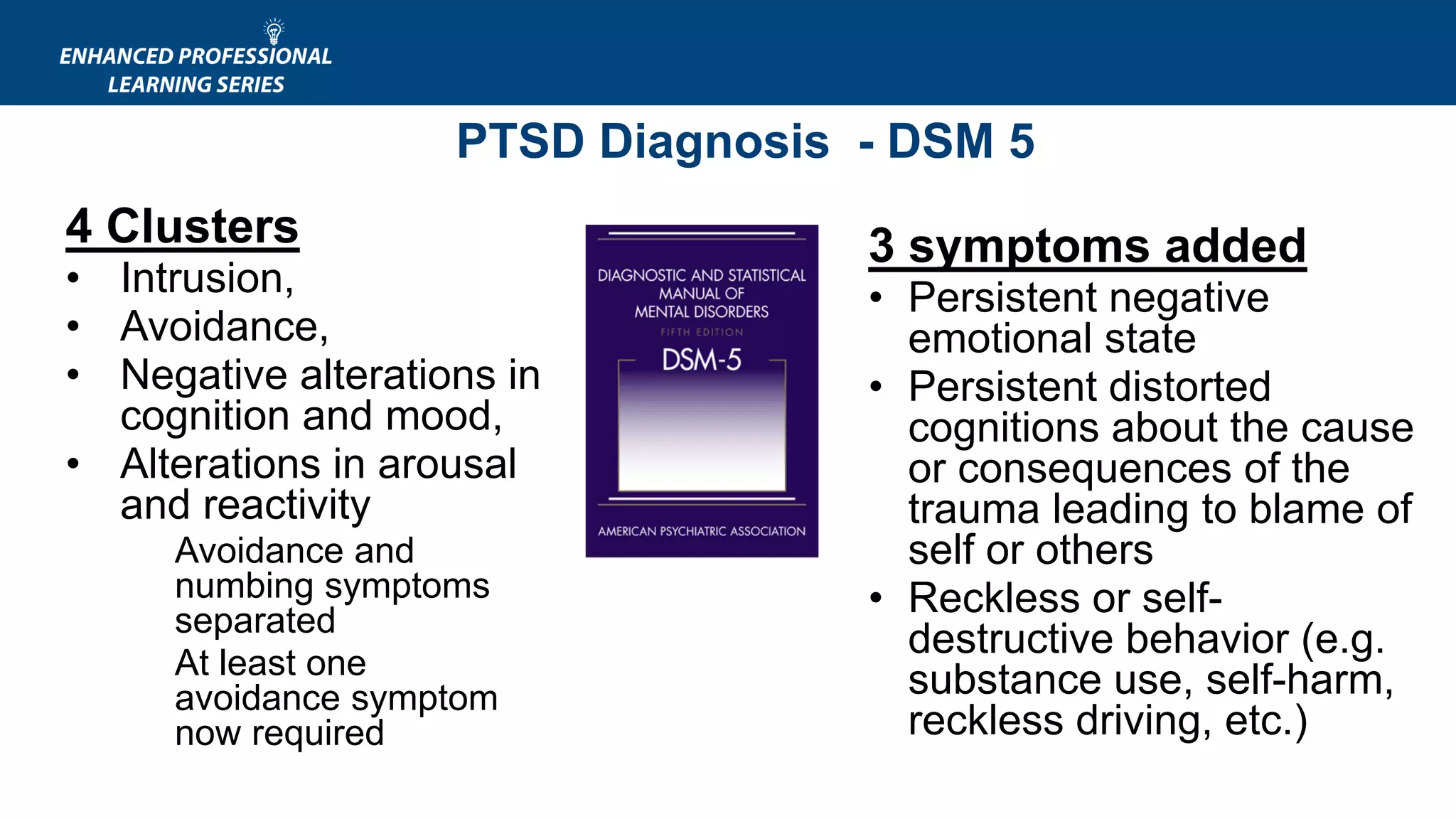
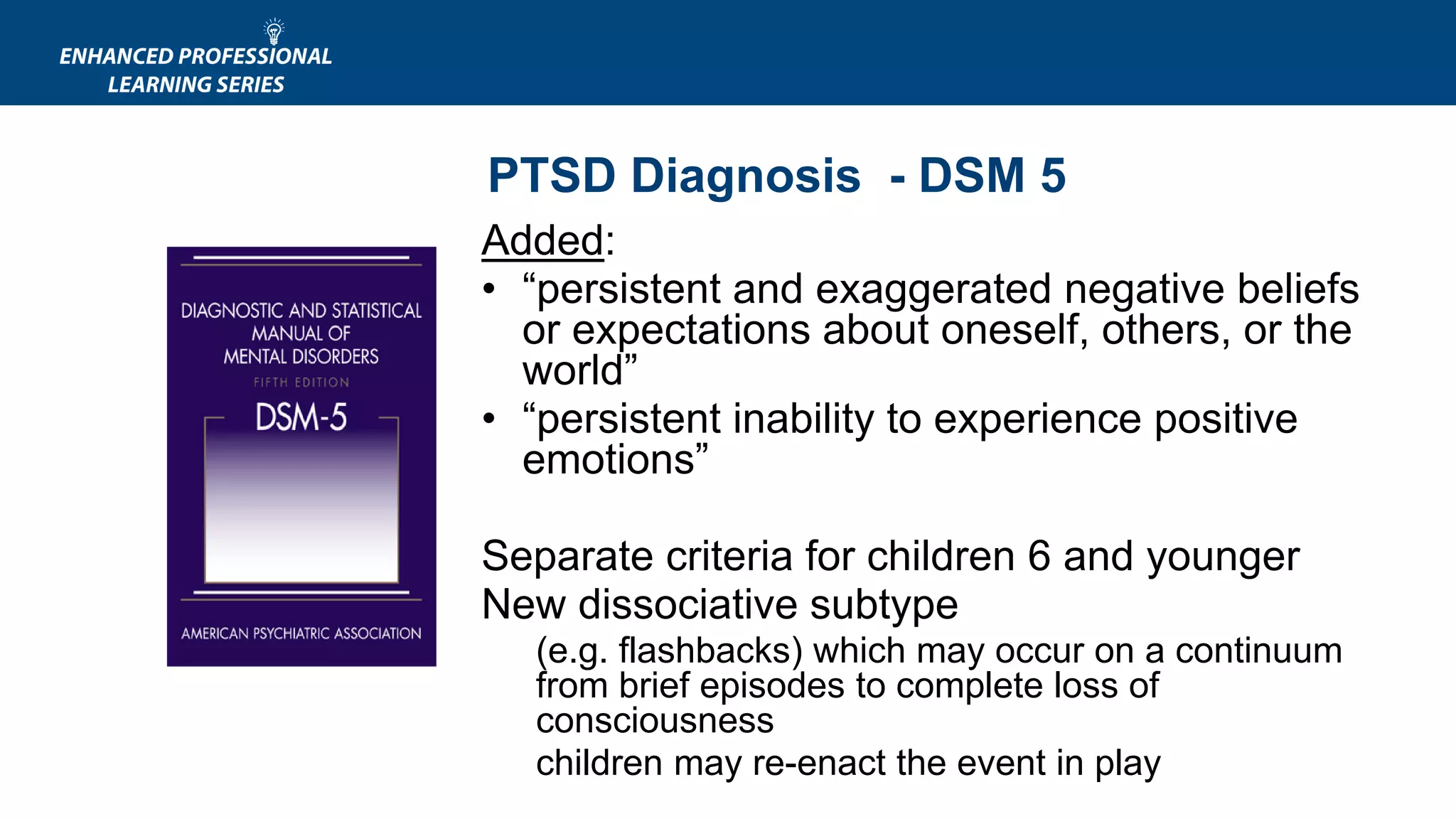
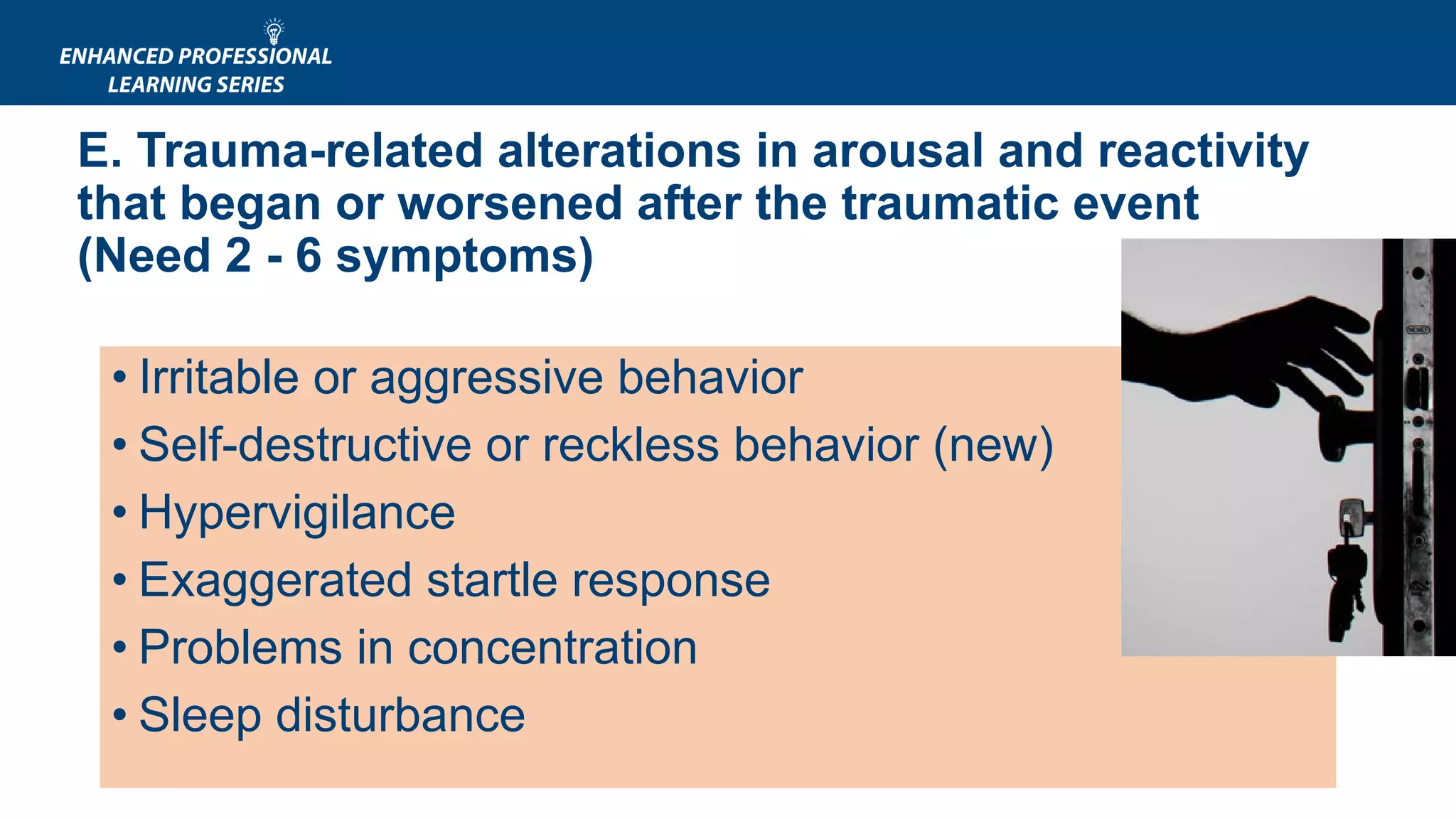
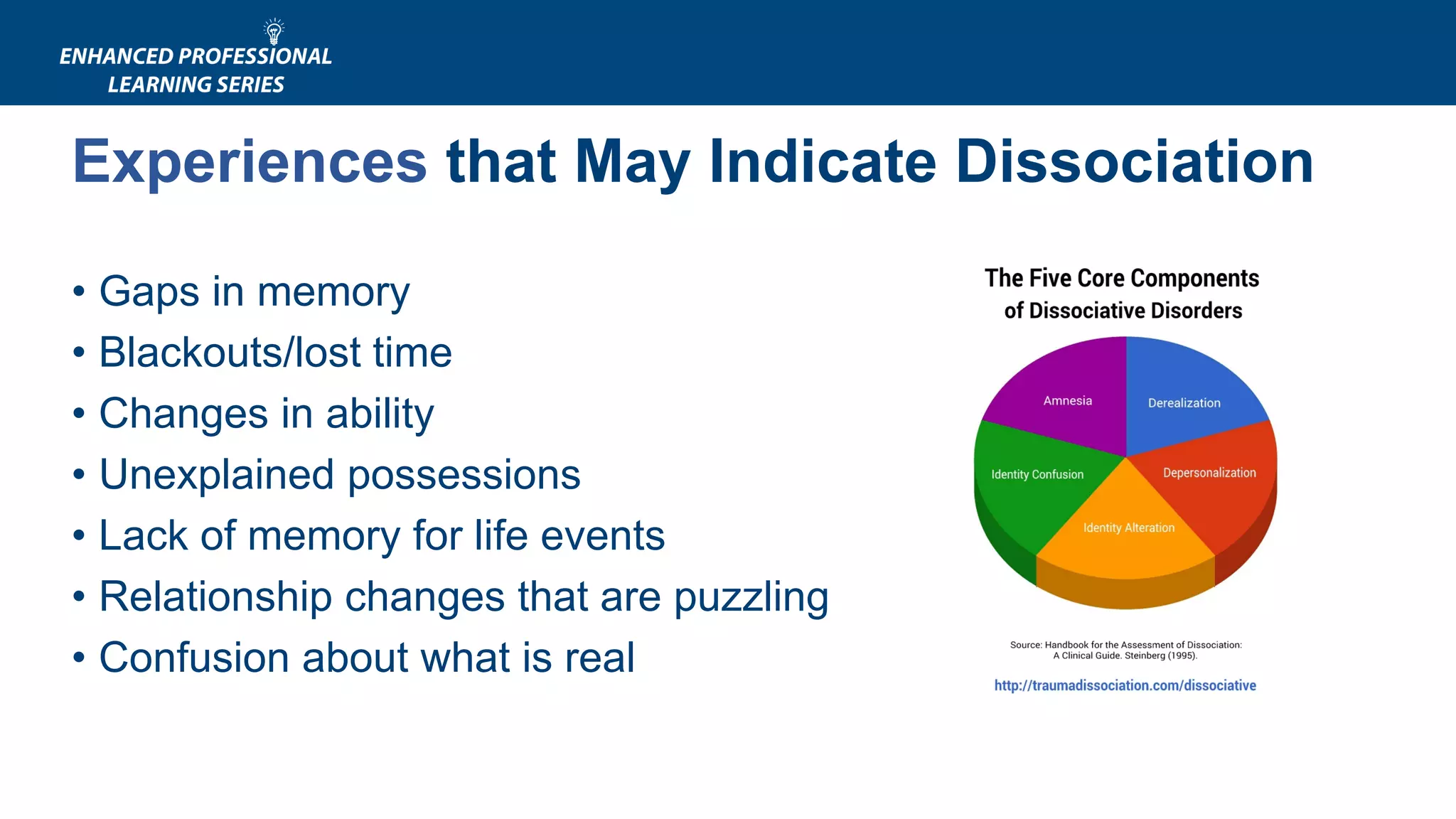
This document provides an overview of a 6-week training series on integrating a trauma-informed approach in behavioral health settings. The training covers understanding the impact of trauma, its effects across the lifespan and on the body and brain, and implementing a trauma-informed care approach. Key topics include the prevalence and types of trauma, common trauma responses, PTSD diagnosis, and dissociation. The training emphasizes creating a culture of trauma-informed care through organizational policies, staff training, and identifying and appropriately serving trauma survivors.