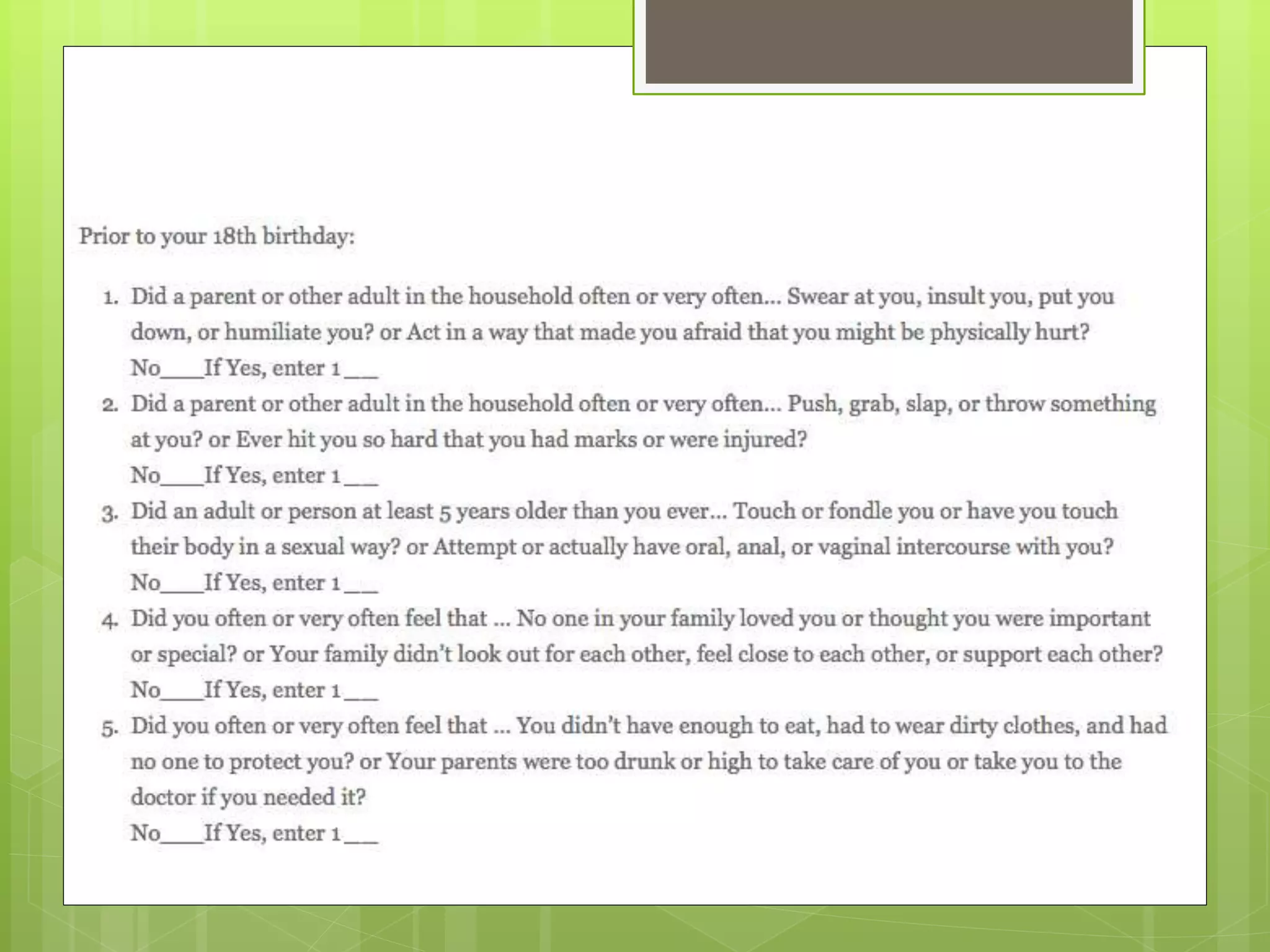
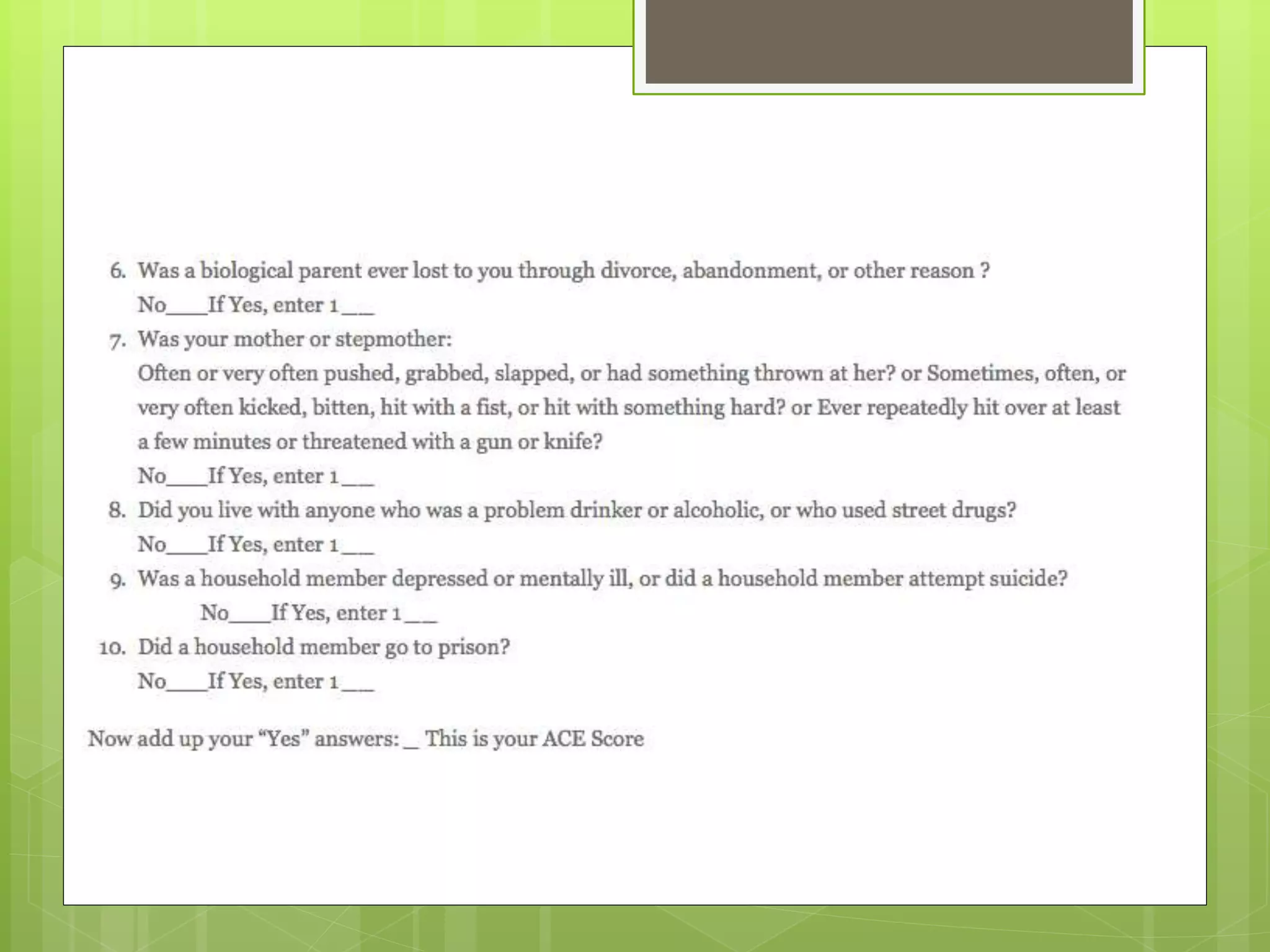
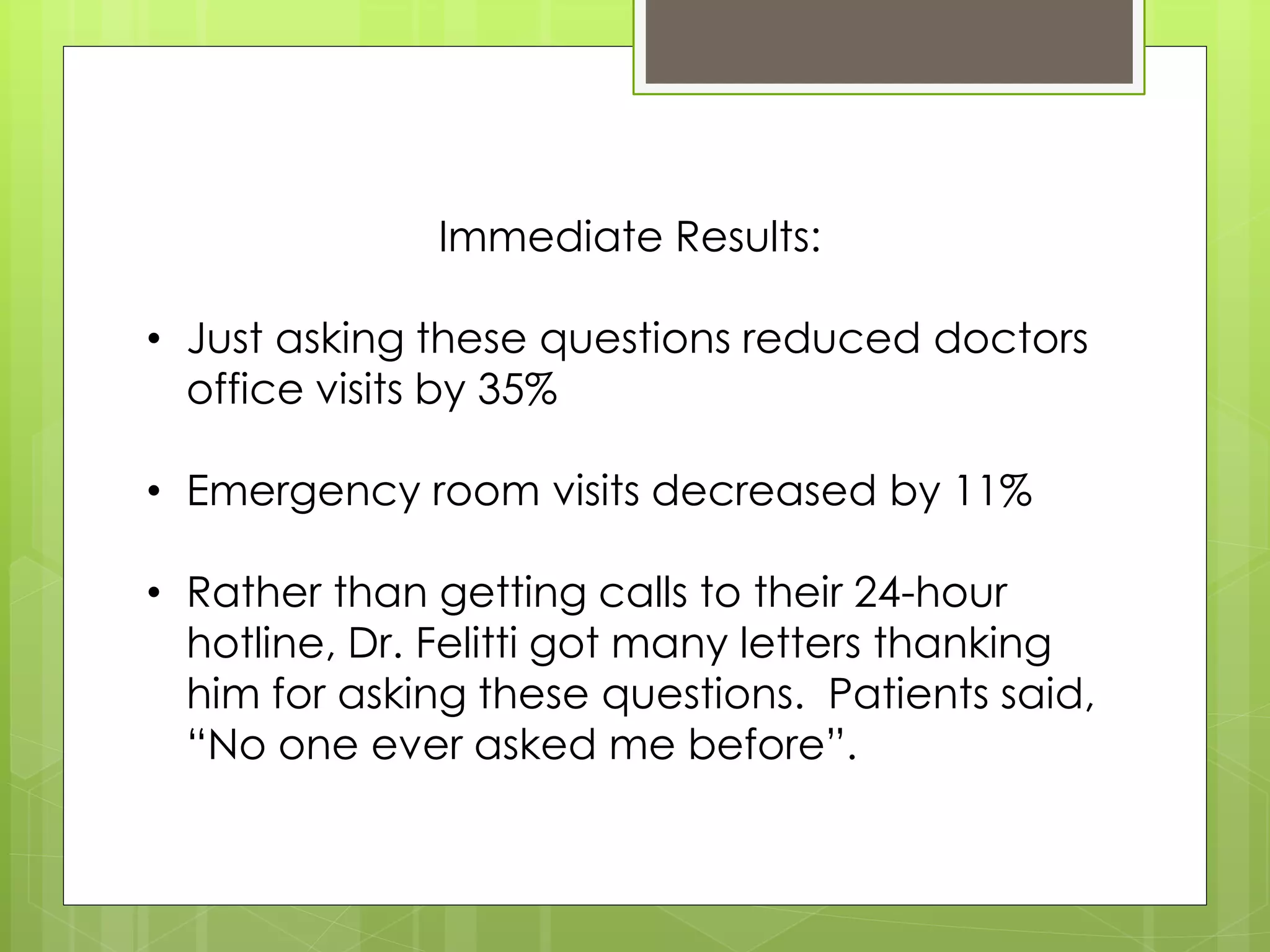
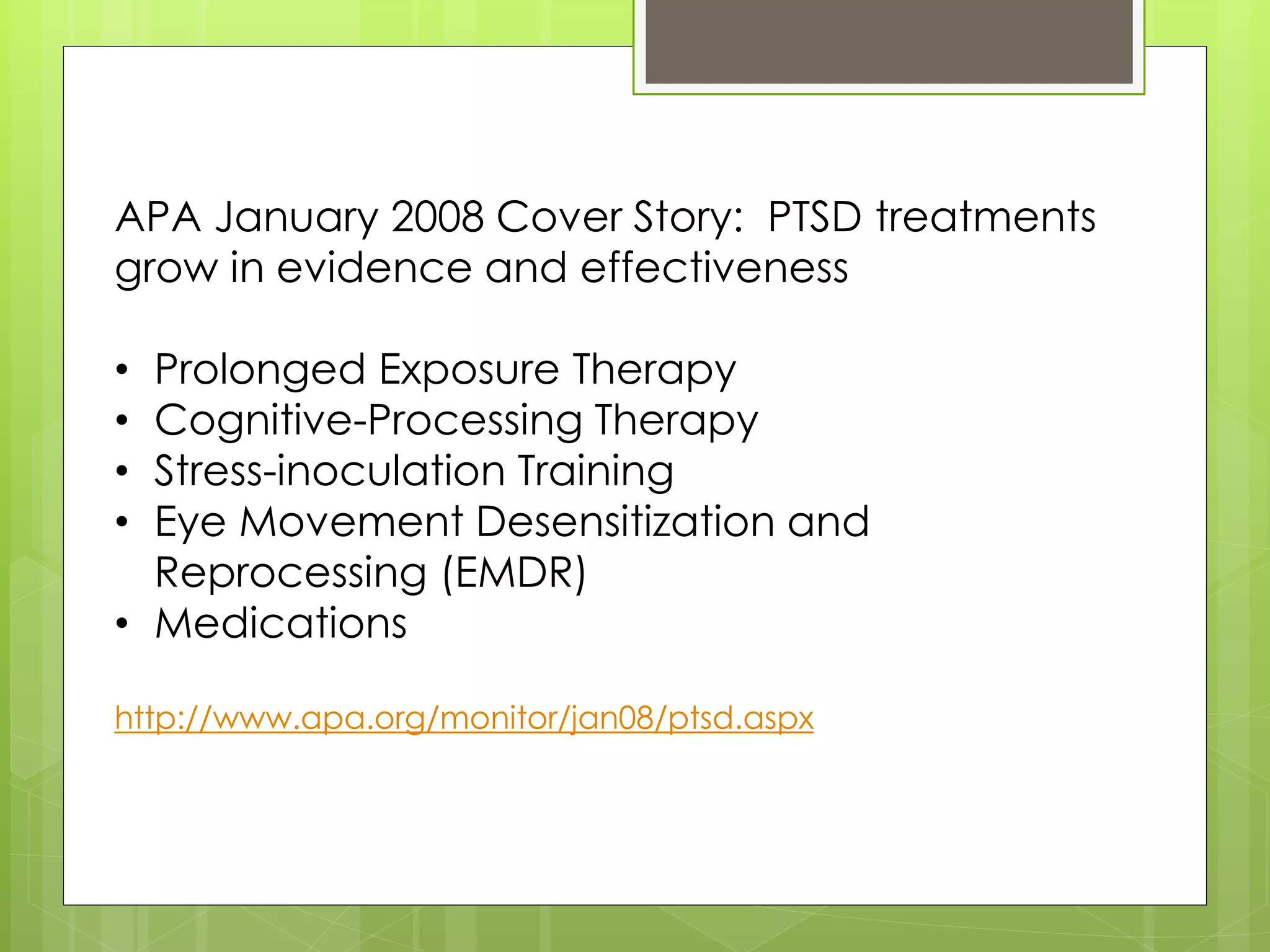
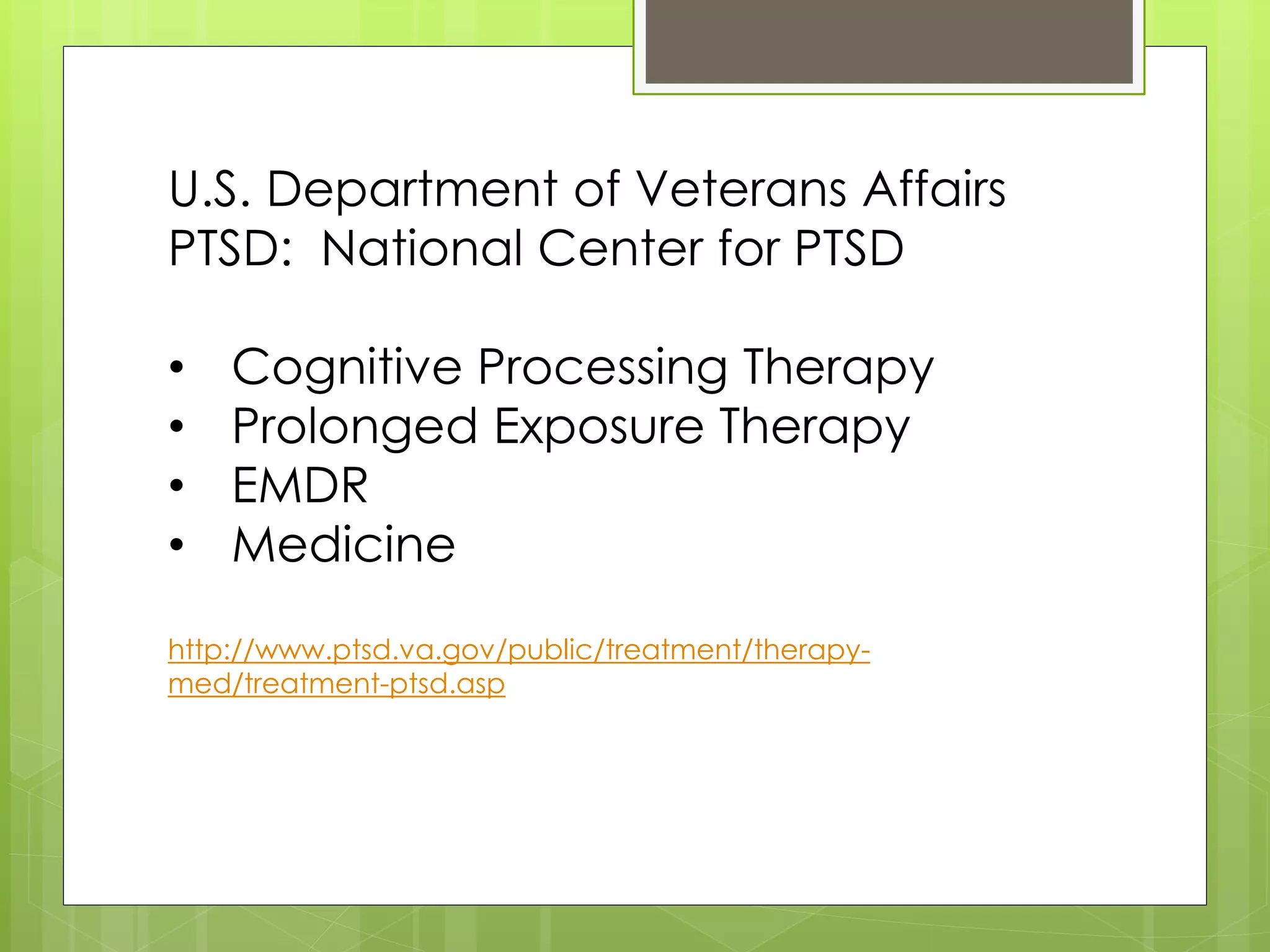
The document summarizes the introductory meeting of the Trauma Informed Care Network (TICN) held on March 14, 2014 in Salt Lake City, Utah. TICN was formed in 2013 by mental health and medical professionals to increase collaboration and education around trauma-informed care. The meeting discussed the impacts of trauma, goals to increase awareness and access to treatment, and potential initiatives for the network such as establishing a speakers bureau and website. Attendees were asked to sign up for the network and its provider list.