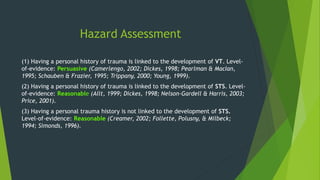
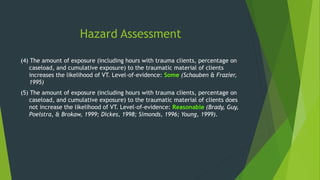
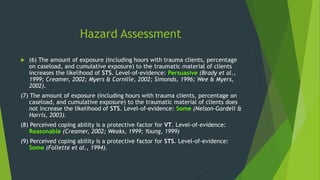
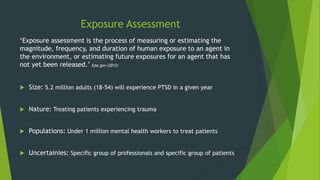
This document discusses secondary traumatic stress and its impact on mental health workers. It provides background on the concept, including early recognition in the 1960s-70s that working with trauma clients can negatively impact caregivers' mental health. Terms like secondary traumatic stress, vicarious traumatization, and compassion fatigue are defined. Symptoms are similar to PTSD and include changes in beliefs and somatic complaints. Risk factors include personal trauma history, exposure level to clients' trauma, and poor coping abilities. Prevention strategies focus on self-care and organizational support. Gaps remain in definitions, treatment options, and addressing stigma around mental health issues in these professions.